Signs You Should See A Spine Specialist
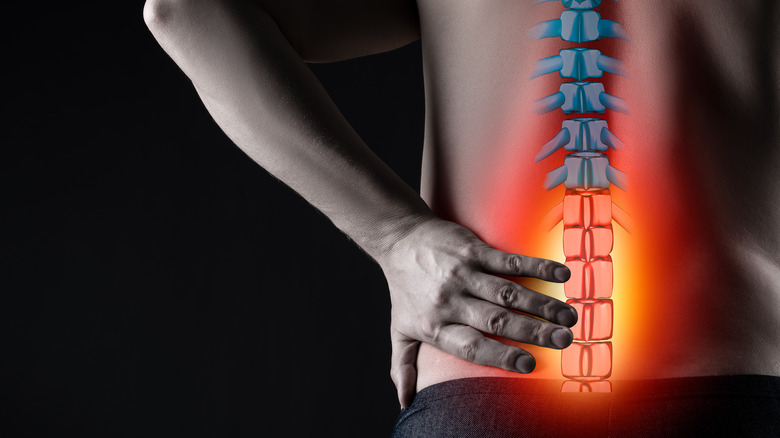
Also referred to as your backbone, the structures that make up your spine enable you to perform everyday motions such as sitting, walking, and bending (via Cleveland Clinic). Made up of 16 different parts, including your back muscles, cervical spine, ligaments, and discs, your spine also helps to support your body weight, spinal cord, and the nerves that run through the area (per Cedars-Sinai).
Your spine has 33 vertebrae separated into five sections. At the top is the cervical or neck area, where seven vertebrae allow you to move your head. The middle or chest area is your thoracic spine and has 12 vertebrae. Finally, the lumbar part of your spine is located toward the bottom and has five vertebrae that connect to your pelvis and allow you to bear weight and lift things (per Cleveland Clinic). Below the lumbar spine is a triangular-shaped bone called the sacrum. The sacrum is a large bone comprised of five sections that fuse before birth (per Cedars-Sinai). Beneath your sacrum, you will find your coccyx. Also called your tailbone, this area consists of four fused vertebrae that form the bottom of your spine (via Cedars-Sinai).
According to the Mayo Clinic, 80% of the population has back pain at some point in their lifetime, and nearly a quarter have experienced it in the past three months. But while back pain is common and can sometimes be resolved with rest and at-home treatments, there are some symptoms that signal you need to see a spine specialist. Let's dig in.
Chronic pain
A 2006 survey published in the Journal of the American Medical Association (JAMA) found that over 10% of those questioned suffered from chronic lower back pain. Additionally, a 2015 research review of nearly 30 studies found that among adults between the ages of 20 and 59, nearly 20% have chronic back pain (per Faculdade de Saúde Pública da Universidade de São Paulo). That number rises to over 25% after the age of 60.
The National Institute of Neurological Disorders and Stroke (NINDS) defines chronic back pain as that which lasts at least 12 weeks. Approximately 20% of those with back pain still have symptoms after one year, regardless of treatment. According to Spine-health, chronic pain can get worse over time, and it doesn't have to be consistent or have a medically diagnosable cause.
Duke Health recommends taking an over-the-counter pain reliever and applying ice to the affected area for the first two days of pain. If your pain persists, use a heating pad for the next few days. If your pain continues and forces you to change your routine, medical professionals at the Mayo Clinic recommend you make an appointment with your doctor.
Neck pain
According to Practical Pain Management, over 30% of American adults see their doctor for neck pain annually. Of those, nearly half will be diagnosed with chronic neck pain. Additionally, at some point, between 20-70% of adults in the U.S. report suffering life-changing neck pain. Spine-health describes several different ways that neck pain can present. For example, some patients have stiff necks that cause them to be unable to move in certain ways. Others have one spot that hurts, or characterize their pain as less intense but covering more neck area. In addition, headaches and muscle spasms often accompany neck pain.
The cervical spine — the portion of your spinal column that is contained in your neck — is comprised of nerves, bones, joints, ligaments, and muscles. In between each vertebra of your cervical spine is a shock-absorbing disc. Pain can come from any of these structures and result from age, poor posture, arthritis, degeneration, an accident, or injury, according to the American Association of Neurological Surgeons (AANS). Neck pain often results from a spinal canal narrowing that puts pressure on your spinal cord or your nerves. Since most of the nerves in your body go through your neck, the issue causing pain can also create problems in another part of your body.
Healthgrades recommends seeing a medical professional immediately if your neck pain results from an injury or accident. Make an office appointment if stretching, massage, and applying ice or heat don't relieve your pain.
Shoulder pain
According to Spine-health, shoulder problems often result from poor posture, not lifting items correctly, and overuse. As a result, you end up with tendon issues, instability, arthritis, or breaks that cause pain, according to the OrthoInfo. Shoulder pain can also result from the complicated relationship the structures of your shoulder have with your back (per Laguna Orthopedic Rehabilitation). The two body parts share a muscle known as the trapezius that connects your shoulder to your upper back at the scapula (shoulder blade). The scapula enables shoulder movement. If either the trapezius or the scapula is the problem, shoulder pain could result.
Most shoulder pain can be treated at home with ice and over-the-counter pain medication, and if it doesn't get better in two weeks, see your doctor (per Medline Plus). However, if your pain comes on suddenly, seek immediate medical attention as it may be a sign of a heart attack, especially if the pain travels to your chest, jaw, or neck and is accompanied by shortness of breath, dizziness, or sweating.
Headaches
Headaches result from different mechanisms triggering specific nerves (via Cleveland Clinic). These nerves then disturb your muscles and blood vessels, resulting in the pressure and pain that is known as a headache.
The Journal of Headache and Pain published a review that showed that there seems to be a relationship between chronic low back pain and chronic headaches. Professor Martin Underwood from Warwick Medical School said, "In most of the studies we found that the odds were about double — either way, you're about twice as likely to have headaches or chronic low back pain in the presence of the other" (via Science Daily). Underwood notes that this may imply that in some people, both conditions might originate from the same cause. He says, "It suggests the possibility of an underpinning biological relationship, at least in some people with headache and back pain, that could also be a target for treatment."
Medical professionals at the Mayo Clinic recommend you see a doctor if your headaches are happening more often or are more painful than usual, if they don't get better when you use over-the-counter drugs, or if they interfere with your normal activities.
Stiffness
When your back is stiff, you may feel like it's stuck and tight, making movement painful or difficult (via Premiere Pain Centers). Johns Hopkins Medicine reports that back stiffness is the most common symptom associated with several forms of spinal arthritis, which is a common health problem. Indeed, eight out of ten people over the age of 55 have some degree of cervical spine osteoarthritis (via Spinal Osteoarthritis). Furthermore, over two-thirds of those between 45-64 have facet joint arthropathy, a kind of arthritis that impacts the spinal joints. That number rises to almost 90% after the age of 65.
In addition to arthritis, disc degeneration and poor sitting posture also cause your back to feel stiff (per Spine-health). Healthline adds that repeated heavy lifting, unexpectedly moving oddly, and being out of shape can cause back stiffness.
St. Luke's Health recommends over-the-counter pain medication and RICE (rest, ice, compression, elevation) for the first two to three days of back stiffness. On day three, you can start to apply some heat. See a doctor if the stiffness doesn't improve after a few weeks, makes daily activities difficult, is awful first thing in the morning, or worsens over time (per Healthline).
Muscle spasms
According to Spine Universe, 80% of adults will experience a muscle spasm in the low back at some time, and once you've experienced one, your chances increase of having more. Muscle spasms occur when your muscles spontaneously contract. Muscle spasms often result in a pH drop that signals a release of the material that causes pain (per Deutsches Ärzteblatt International). Muscle Cramps adds that spasms can affect one or more muscles or muscle fibers and last a few seconds to a few minutes.
The most common causes of muscle spasms are overuse, accidents, and injuries (per Spine Universe). However, Spine-health recommends seeking medical attention for your muscle spasms if they last more than a week or two, as they may indicate osteoarthritis, degenerative disc disease, spinal stenosis, or a herniated disc. Additionally, spasms are a cause for concern because they interfere with your back muscles' ability to help you keep your balance and stability (via Spine Universe).
Stretching and strength training can help prevent muscle spasms in your back, but these exercises should not be started until the pain has subsided.
Bowel and bladder problems
Back pain that comes along with conditions like irritable bowel syndrome (IBS) is a circular issue in that Healthline reports that it could be what is known as "referred pain," discomfort that is felt in a different place than where it originates. In this case, back pain may actually originate in the gut and is due to issues like constipation, gas, or bloating that are common in those with IBS. Additionally, according to Medical News Today, constipation and bowel obstruction cause feces to get backed up. If enough poop collects in your colon, it presses down on your sacral nerves, resulting in pain.
However, the reverse can also be true: Sometimes back problems can lead to bowel and bladder issues. Central Florida Urogynecology explains that compression of the nerves in the lower back can cause overactive bladder, urinary retention, fecal incontinence, and severe constipation.
Exercising, drinking more water, and taking over-the-counter laxatives and painkillers may help relieve your symptoms (via Healthline). However, contact your doctor if the pain is extreme, doesn't let up with diet changes and other home remedies, or is coupled with bloody stool.
Leg weakness
Back pain with leg weakness is often a sign of damage or irritation to one or more of your nerves. While over-the-counter medication often relieves both symptoms, medical professionals at the University of Maryland Medical System warn that it could cause permanent problems if left untreated.
A common cause of leg weakness associated with back pain is stenosis. In fact, over one in 10 American adults have lumbar spinal stenosis, and that number doubles after the age of 60 (per JAMA). According to the American Academy of Family Physicians (AAFP), lumbar spinal canal stenosis occurs when the space where your nerves go from your back to your legs gets smaller. Stenosis results from bone and tissue growth caused by arthritis, falls, accidents, and wear and tear on your bones and joints. As this space narrows, your nerves get squeezed. And one side effect of stenosis is weakness.
According to Healthline, if leg weakness comes on suddenly, it might signify something serious that needs urgent medical attention. Additionally, the University of Texas Southwestern Medical Center states that if back pain and leg weakness are coupled with incontinence, it could be a severe illness known as cauda equina syndrome. This disease requires immediate surgery to decompress your nerves and reduce spinal cord nerve damage.
Numbness and tingling
The Merck Manual defines numbness as the partial or complete loss of sensation, and those affected by it might not feel touches, pain, temperature changes, or vibrations. Additionally, those experiencing numbness are often unaware of how their body parts are positioned, making them ripe for balance and coordination issues. Tingling, prickling, and a pins-and-needles sensation often accompany numbness. When numbness and tingling occur together, the Texas Spine & Sports Therapy Center refers to it as paresthesia.
Some spinal conditions — including sciatica, pinched nerve, spinal stenosis, and spondylolisthesis — can be responsible for numbness and tingling in the back or limbs (per International Spine Institute). Disc issues, including degenerative disc disease, and herniated or bulging discs, also cause paresthesia. Medical News Today adds shingles, spinal fractures, infections, tumors, fibromyalgia, and arteriovenous malformations to the list of possible causes of numbness and tingling.
The Spine Center recommends seeking emergency medical attention if symptoms of confusion, vision or speech changes, weakness, paralysis, or loss of bladder or bowel control accompany paresthesia. However, you can make an office appointment if you experience neck, back, or extremity pain or spasms along with numbness and tingling.
Fever
If you're an adult and your temperature rises beyond 100.4° F (38° C), you have a fever (via Merck Manual). If you have back pain and fever together, it might indicate one of a couple health problems.
Kidney and bone infections are two common causes of fever accompanying back pain (via HealthPages.org). Your body refers kidney pain to your back due to the nervous system's wiring. While bone infections can occur anywhere in the body, when they happen in the spine, it results in low back pain with fever. Another less common cause of fever accompanying back pain is a spinal epidural abscess, or the buildup of infectious liquid in what is known as the epidural space, located outside the dural sac surrounding the nerve roots (per Matthew D. Hepler, MD, Pediatric and Adult Spine Surgery). As the pus accumulates, it compresses your spinal cord. In addition to back pain and fever, spinal epidural abscesses are often accompanied by bladder or bowel problems. In general, you see a doctor if you experience lower back pain with a fever, as it could indicate a serious health issue (per Medicover Hospitals).
Shooting pain
Your sciatic nerve runs through your pelvis and down the back of each leg (per Mayfield Brain & Spine). Sciatica describes it as the largest nerve in the body. Pain associated with this nerve is referred to as sciatica, and affects up to 40% of American adults at some point in their life, making it a common cause of shooting pain.
Sciatica results from several other conditions, including herniated or slipped discs that compress the nerve (via Healthline). Piriformis syndrome, when your piriformis muscle puts pressure on your sciatic nerve, is another cause, as are spinal stenosis and bone spurs. The location where the nerve is compressed determines the amount and position of your pain (per Spine-health). To provide a proper diagnosis of sciatica or the underlying condition that is causing it, your doctor must determine whether your pain is shooting/radiating or referred. While shooting pain moves through the body, referred pain is felt in only one spot — but this spot is in an area other than where the pain originates (per Healthline).
The Hospital for Special Surgery recommends seeing a doctor if you have shooting pain that has not improved after three days of rest, icing, and over-the-counter pain relievers. Seek immediate medical attention if your shooting pain is accompanied by leg weakness, incontinence, or numbness (per the UT Southwestern Medical Center).
Injury or accident
The Good Body reports that there are over two million back injuries annually in the U.S. Over 90% of these are due to poor posture and workplace injuries. In fact, over one million accidents involving the back occur at work each year, making up 20% of all workplace accidents. Furthermore, according to SpinalCord.com, over one-third of the over 2.3 million annual car accidents in the U.S. result in spinal cord injuries, which is more than are caused by violence, sports-related injuries, and medical complications combined.
Regardless of how a back injury occurs, the most common results are sprains, strains, and traumatic injuries, including herniated discs and fractures to the vertebrae (per MedlinePlus). Sprains occur when your ligaments are overstretched or torn (via National Institute of Neurological Disorders and Stroke). Strains are tears to your muscles or tendons. Traumatic injuries also harm your muscles and tendons. They can also put pressure on your spine and cause the discs in your back to rupture.
Cedars-Sinai recommends you seek medical attention if your back injury results from an accident. You should also see a healthcare professional if your pain gets worse or doesn't at least improve somewhat using home remedies for a few days, wakes you from sleeping, or doesn't go away within a month.
Types of spinal specialists
Various specialists can help you with spinal problems and back pain (per Mayfield Brain & Spine). However, speaking to Harvard Health Publishing, chiropractor Dr. Matthew Kowalski recommends seeing either your primary care physician or a chiropractor to have your back pain diagnosed. In fact, over one-third of those with back pain consult a chiropractor as their first step.
Another option is a physiatrist. Physiatrists specialize in physical medicine and rehabilitation (via Penn Medicine). According to spine surgeon James Dowdell of HSS, "A physiatrist is the primary care doctor of the back."
The spinal specialist you see depends on the issue you are experiencing and how bad it is affecting you. Mayfield Brain & Spine describes several doctors specializing in spinal issues, including neuro and orthopedic surgeons. In addition to surgical treatments, neurosurgeons also offer nonsurgical care for various neurological problems related to the spine. Orthopedic surgeons diagnose, treat, and help prevent musculoskeletal system disorders surgically and nonsurgically.
Prevention of spinal problems
The chances of developing back pain and spinal problems increase with age, and if you're pregnant, have arthritis or cancer, or are overweight or smoke (per the Office of Disease Prevention and Health Promotion).
However, there are several steps you can take in various aspects of your life to reduce your risk (via OrthoInfo). Begin by ensuring your mattress is supportive. Placing a pillow under or between your knees will ensure you maintain proper posture while you sleep (via CK Birla Hospital). Additionally, Spine-Health notes that it's essential to keep your back straight for at least an hour after you get up each morning to enable the discs in your back to return to their normal pressure.
The Office of Disease Prevention and Health Promotion also recommends you incorporate both muscle-strengthening and stretching exercises into your routine at least two days a week. Furthermore, it would be best if you sat in an ergonomic chair to help you sit properly and not slouch (via Spine-health). When lifting, bend at the hips, keep your chest forward, and hold the object close to your body (per Spine-health). To pick up a lighter thing off the floor, lean over the object, bend one knee, and use nearby furniture for support as you reach for the object (via OrthoInfo).