Ventilators: A Comprehensive Guide
In 1928, doctors used the first ventilator to help a young patient with respiratory paralysis (per Harvard T.H. Chan School of Public Health). Originally called the "iron lung," the first respirator came into high demand during a polio epidemic a few years after its initial trial, because the machine could give short-term help to the body as nerves and muscles affected by the virus recovered (via STAT). In addition, this gadget made it so that respiratory failure no longer resulted in death.
According to the National Heart, Lung, and Blood Institute, ventilators move air in and out of your lungs through a mask or breathing tube. Used for patients who cannot breathe on their own, most ventilators are found in hospitals or medical transports, though some do exist for use in the home. Kathy Langley, a nurse and instructor at the University of Alabama Birmingham School of Nursing, explains to UAB News that "It becomes an external set of lungs. The ventilator allows the patient to rest and to heal while the machine does the work of the lungs."
Who needs a ventilator?
NBC News reports that ventilators are primarily used for patients unable to breathe alone, often due to illness or injury impacting the lungs. When someone cannot breathe adequately, they may not take in enough oxygen or expel enough carbon dioxide, resulting in either hypoxemia (low blood levels of oxygen) or hypercapnia (high blood levels of carbon dioxide), according to an article in JAMA.
MedicineNet further explains that getting oxygen in and carbon dioxide out is done through inflation and deflation of the tiny air sacs in your lungs, known as alveoli. However, there are numerous reasons why you might be unable to do so on your own and need the assistance of a ventilator. Some reasons doctors put people on ventilators include abnormal breathing (either fast or slow), severe heart disease, an acute asthma attack, chronic obstructive pulmonary disease (COPD), and acute respiratory distress syndrome (ARDS). Additionally, those with bacterial or viral lung infections, including pneumonia and COVID-19, may also need a ventilator, and those under general anesthesia during a surgical procedure need assistance breathing as well. Additionally, people in comas often need the assistance of a ventilator to prevent inhalation of oral secretions into their lungs, known as aspiration (per JAMA).
How ventilators work
When placed on a ventilator, a tube goes into your airways, and a device pushes air into your lungs through that tube (per Self). According to the American Thoracic Society, this endotracheal tube (ET tube) goes through your mouth or nose and into your windpipe. The other end connects to the ventilator. Oxygen is not only pushed into your lungs, but this machine also maintains pressure in your lungs so your alveoli don't collapse. Additionally, the ET tube enables medical professionals to suction out any mucous buildup.
The oxygenation and ventilation pressure settings must be personalized and monitored while you remain on the machine (via Self). The three types of breath settings available on a ventilator are controlled, assisted, and supported. REBELEM explains that when your ventilator is set to controlled breathing, it does all of the work, and breaths are delivered at a specific interval. The setting of assisted breaths gets activated when you try to breathe on your own and suck on the tube to create a change in pressure. The ventilator then takes over and does the breathing work for you. However, if you fail to initiate the breath, the machine still has a setting that causes it to breathe for you automatically. Finally, supported breath mode offers minor support to patients who can trigger the ventilator independently but who need help completing the breathing motions.
Volume-cycled ventilation
According to Respiratory Care, ventilators work through two phases: inspiratory, when oxygen flows into your lungs, and expiratory, when air is let out. The point at which a switch is made is referred to as cycling. Medical professionals use four variables to determine when cycling should occur: pressure, time, volume, and flow. When a volume-cycled ventilator is used, the inspiratory phase ends when a specific air volume is reached.
Volume-cycled ventilation is commonly used for those undergoing general anesthesia during surgery (via General Electric). This kind of ventilator delivers a specified volume of air during every inspiratory phase, which is the easiest mechanical way to assure the lungs are fully filled (via Merck Manuals)
The one drawback of using a volume-cycled ventilator is that there may be a delay in air sac inflation. This lag may reduce the time available for gas exchange, resulting in high inspiratory pressure and the risk of developing barotrauma. Barotrauma is the technical name given to the harm that can occur due to changes in air or water pressure (per MedlinePlus). One symptom of barotrauma that you may have experienced is discomfort in your ears while flying.
Pressure-cycled ventilation
Medical professionals use pressure-cycled ventilators to either partially or entirely aid patient-initiated breathing to reach a consistent airway pressure during each inhalation (per ScienceDirect). Once the pre-set airway pressure is met, exhalation begins. Though the force of the pressure remains the same for each inhalation, the volume of oxygen delivered changes depending on airway resistance, lung compliance, and ventilator stability (per Tracheostomy Education).
RT Magazine reports that pressure-cycled ventilators offer several patient advantages. First and foremost, the machine correlates patient needs and flow delivery. As a result, you are more comfortable and are less in need of sedatives and other medications while using the device. Furthermore, pressure-cycled ventilators enhance the air dispersion throughout the lungs, reducing barotrauma risk while improving the oxygen delivery to your arteries and tissues, especially during bronchospasms that cause high pressure and low distribution.
Pressure-cycled ventilation is most often used to remove patients from mechanical ventilation, enabling their lungs to take on more work with each breath (via Merck Manuals).
Non-invasive positive pressure ventilation (NIPPV)
Another form of ventilator used in the ICU is non-invasive positive pressure ventilation (NIPPV). NIPPV increases lung volume by offering positive pressure without intubation (via ScienceDirect). Air and oxygen get administered through a face mask, nasal mask, or nasal plugs.
According to Merck Manuals, NIPPV is delivered in one of two ways. Continuous positive airway pressure (CPAP) offers constant pressure throughout the breathing cycle. Bilevel positive airway pressure (BPAP) supplies the same continuous airway pressure as a CPAP during the inhalation phase, while expiratory positive airway pressure levels are lower (per ScienceDirect). The Agency for Healthcare Research and Quality reports that both forms of NIPPV offer indistinguishable pressure, volume, assist control, and ventilation assistance from other ventilators available in the ICU. However, NIPPV is for those who can spontaneously breathe independently and is best used on those who don't meet the criteria for intubation.
Intubation must be administered if the patient fails to stabilize within two hours of beginning NIPPV. But on the reverse side, NIPPV has proven to be helpful to patients when their breathing tubes are removed. Science Direct reports that if NIPPV gets immediately used after extubation, it reduces the need for reintubation and lowers mortality rates. In fact, a study published in Chest Journal shows that nearly eight out of 10 patients were successfully extubated within five days and infection risk was reduced when NIPPV was introduced after weaning. Furthermore, medical professionals reduced the average patient's ICU stay by three days using NIPPV, and cut costs by almost 60%.
What happens when you are put on a ventilator?
Going on a ventilator starts with the administration of a combination of sedatives and paralytic agents (per Insider). You may also get medication that causes you to become unconscious (via The Ohio State University Wexner Medical Center). Brian Boer, an ICU doctor and pulmonologist at the University of Nebraska Medical Center, told Insider that this reduces gagging during the procedure. Yale Medicine's Lauren Ferrante, a pulmonary and critical care specialist, explains that it also helps prevent self-harm if you suffer from delirium or confusion while on the ventilator.
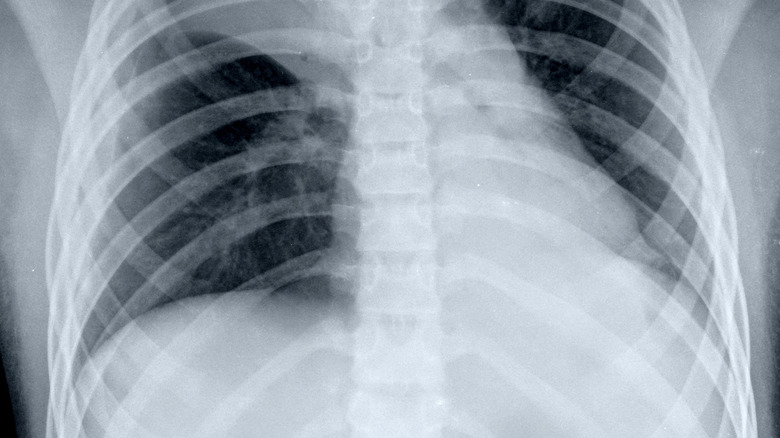
Dr. Boer further explained that a doctor uses a speculum to widen your airway and slides the breathing tube down to your lungs (via Insider). At that point, a small cuff gets placed around the tube to prevent particles from escaping, and then the machine gently pumps highly oxygenated air at a steady rate, simulating breathing. You will also have a feeding tube inserted into your nose or mouth because you can't eat while on a ventilator. Finally, the medical team takes an x-ray to ensure proper placement and an ultrasound to check for proper lung inflation. The entire process takes around 15 minutes.
What to expect if your loved one is placed on a ventilator
Medical professionals at Mount Sinai warn those visiting patients on ventilators that the person will be sleepy due to the medication they're given. Also, communication will be limited when the patient is awake due to their inability to speak.
Various tubes and wires will be attached to a monitor so the medical team can track your loved one's heart and respiratory rate, as well as their blood pressure and oxygen saturation, and make machine adjustments as needed (via American Thoracic Society). Patients are also watched closely for mucous accumulation in their chest. If this occurs, the mucus is suctioned out to help prevent pneumonia and to ensure enough oxygen reaches the patient's lungs (per Mount Sinai).
Ventilator Safety explains that every hospital has procedures to follow if the ventilator alarms sound and policies to ensure proper care. In addition to administering tests to determine when the patient is ready to be removed from the ventilator, while on the machine your loved one will get medication to prevent peptic ulcer disease, and someone will brush their teeth regularly. Additionally, the patient might be fitted with compression stockings so they don't get deep vein thrombosis, and their healthcare team will move them frequently to avoid muscle loss and pressure sores.
How long might someone be on a ventilator?
The American Thoracic Society explains that ventilators help to maintain life while someone heals. However, ventilators on their own do not treat the illnesses or accidents that caused their initial need. Therefore, those caring for you while you're on a ventilator do their best to ensure your time on the device is as limited as possible.
However, the ultimate length of time depends on several factors. One element that comes into consideration is your health before you needed a ventilator. For example, if your lungs weren't strong before you were intubated or you have other damaged organs, your stay on a ventilator would be longer than someone who didn't have the additional problems. Pulmonologist Lauren Ferrante at Yale Medicine adds that the initial reason your doctor chose to use a ventilator also comes into play when determining how long you will need it. These machines may be used for just a few hours during surgery, or for days to weeks in the case of lung injuries and severe illnesses like pneumonia. Additionally, she adds that the longer you stay on a ventilator, the weaker your lungs become.
Weaning off a ventilator
When the medical staff in the ICU believes you are ready to be weaned off the ventilator, they begin the process by reducing the pressure setting on the machine (via Physiopedia). Next, they will move you to a seated position and suction any mucous in your airway. Then, you will be given oxygen through a CPAP, and you will get asked to try and breathe on your own while being monitored. According to a review published in Revista Portuguesa de Pneumologia, this spontaneous breathing trial (SBT) lasts up to two hours, and if successful, you will be extubated at that point. Approximately 70% of ventilator-dependent patients get successfully weaned and can maintain spontaneous unassisted breathing after extubation.
The weaning process can occur quickly or take weeks to complete, depending on the length of time you were dependent on the ventilator and the severity of the illness that made the machine necessary in the first place (per Chelsea and Westminster Hospital). Some causes of weaning failure reported by Physiopedia include muscle atrophy, fatigue, diaphragm paralysis, and the patient feeling scared they may suffocate during the process.
Infections resulting from ventilator use
Though ventilators help keep you alive by aiding you in breathing when you cannot do so on your own, they are not without complications. One of the most common and the most serious is developing pneumonia or another chest infection while you are intubated (per the National Heart Lung and Blood Institute). In fact, the Virginia Department of Health reports that nearly 50,000 cases of ventilator-associated pneumonia (VAP) occur annually, and this type of illness accounts for close to 40% of all hospital-related pneumonia infections.
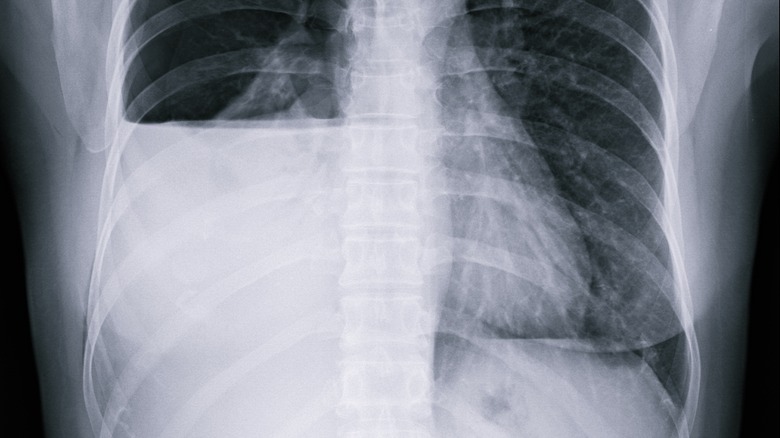
Merck Manuals defines VAP as occurring after at least two full days of intubation. The infection results from a breach of your airway defense system. When you are on a ventilator, you cannot cough or clear mucous that accumulates in your lungs, resulting in bacteria pooling in both the tube cuff and the tube itself. Signs of VAP include fever, increased white blood cell count and tracheal secretions, and decreased oxygenation. Testing for VAP consists of a chest x-ray and blood culture. If you have the infection, VAP gets treated with antibiotics.
According to a study published in Tanaffos, VAP occurs in up to one-quarter of all ventilated patients. And it's a quite serious complication, as the mortality rate for VAP is nearly 50% (via Institute for Healthcare Improvement).
Collapsed lung (pneumothorax) from ventilation
Another complication of being put on a ventilator is developing a collapsed lung. Medically referred to as pneumothorax, Penn Medicine explains that this condition results from air leaving your lungs and entering the space between your lungs and the wall of your chest. According to the American Thoracic Society, this happens because being on a ventilator causes lung weakness that can result in a hole in the lungs. In turn, this means the ventilator won't work as effectively, because the pressure from the escaped air makes it difficult for your lungs to expand fully (per Penn Medicine).
While many collapsed lungs get diagnosed through a chest x-ray, CT scans are considered the gold standard in diagnosing pneumothorax in ventilated patients. In fact, a review in the Journal of Thoracic Disease shows that CT scans were 30% better at identifying a pneumothorax. Once the pneumothorax is identified, doctors insert a tube into your chest to drain the leaking air. The tube gets removed once your lung has healed (per the American Thoracic Society).
Ventilator-induced lung injury
According to Benumof's Airway Management (Second Edition), ventilator-induced lung injury (VILI) is defined as acute lung damage resulting from the use of mechanical ventilation. Patients most often present with hypoxemia when VILI occurs. Doctors diagnose VILI by ruling out other causes of low blood oxygen levels through CT scans and x-rays, according to Ventilator-Induced Lung Injury (VILI).
Clinics in Chest Medicine details four types of VILI: barotrauma, volutrauma, atelectrauma, and biotrauma. Barotrauma and volutrauma are both caused by high lung pressure. Atelectrauma is attributed to the stress on the lung caused by repeated opening and closing of alveoli while on a ventilator (per European Society of Intensive Care Medicine). Finally, biotrauma is an inflammatory response to mechanical lung injury.
Researchers reported in Nature Communications that part of the reason ventilation can lead to lung injury is that the body sees the ventilator as an invader. To fight this enemy, inflammation occurs. Your body then releases a microRNA to combat the irritation. However, the body fails to make enough to fight the ventilator it perceives as the enemy. The researchers note, though, that if this bodily response can be harnessed and the microRNA more effectively delivered, it may help to prevent lung injury during ventilation — though more research on this issue is needed.
Atelectasis resulting from being on a ventilator
Another type of lung collapse brought on by a ventilator is known as atelectasis. This issue affects just part of the lung, not all of it (per MedlinePlus). According to the Mayo Clinic, one cause of atelectasis is your air sacs filling with fluid. OpenAnesthesia reports that underinflation and compression can also cause atelectasis in ventilated patients, especially if they're obese. According to Merck Manual, atelectasis results from a blockage and can be caused by inhaling a foreign object or from something pressing from the outside of the lungs.
Atelectasis indicates that this type of lung collapse affects as many as 90% of those who've undergone general anesthesia. Up to 20% of the time, it occurs before surgery begins. However, it can happen up to 72 hours post-op as well. Atelectasis usually presents without symptoms. Treatment, according to Johns Hopkins Medicine, includes repositioning your body so the lung can re-expand and/or mucous can drain, and tapping on your chest to loosen additional mucous.
Inability to discontinue ventilator support
According to a review published in the British Medical Journal, one in five ventilated patients fails to come off the machine the first time their medical team tries to wean them. The number of failures tends to increase as patients stay ventilated longer. The primary reason many patients fail to wean is the disproportion between your muscles' work while breathing and their capacity to do the job (per Cancer Therapy Advisor). Another cause of failure is cardiac disease resulting in inadequate blood flow and oxygen delivery to your respiratory muscles, causing fatigue.
The best way to determine if a patient is ready to be weaned off a ventilator is by performing a series of tests that show oxygen concentration, artery tension, and pressure and sedation levels (per the British Medical Journal). These evaluations can be performed daily, lowering the number of patients who remain intubated for longer than 21 days and decreasing mortality rates. The most common sign of failure is rapid shallow breathing upon disconnection of the ventilator.
Medical professionals sometimes perform a tracheostomy on patients who fail to wean (via the Intensive Care Hotline). During this procedure, a tube gets placed in their neck, allowing them to breathe. Tracheostomy is easier to tolerate, decreases sedation, makes suctioning and talking easier, and improves the ability to brush teeth and maintain oral hygiene. As the patient heals further, eventually the hope is that the trache tube can also be removed, and the patient will breathe entirely on their own again (per the Intensive Care Hotline).