The Different Ways You Can Receive Chemotherapy
Most of us know that chemotherapy, or "chemo," is drug treatment for cancer. Chemotherapy drugs are cytotoxic – meaning they work by killing the cancerous cells (via the American Cancer Society). Within the larger class of chemotherapy treatments for cancer, however, there are a variety of ways that specific medicines work. Health education on these details can help you or a loved ones know what to expect from the chemotherapy process and how to best plan for treatment.
Interestingly, chemotherapy has roots in the World War II era (via the American Cancer Society). It was discovered that mustard gas could trigger toxic cellular changes in servicemembers who had been exposed to it. The U.S. Army began studying anti-cancer measures (as protections against possible weapons) and found that a compound called nitrogen mustard could fight lymphoma, leading researchers to discover a family of chemicals called alkylating agents. Alkylating agents could, amazingly, damage the DNA of cancer cells, destroying them. Soon afterward, pediatric pathologist Sidney Farber showed that a substance closely related to folic acid could treat acute leukemia in children. From here, chemotherapy research and treatment continued to evolve into our modern protocols. There are a variety of ways that chemotherapy is administered today, according to the type and severity of cancer.
Oral chemotherapy medications
When we think about chemotherapy, it may conjure up images of injection therapy, since that's what's usually depicted in television and film. In reality, chemo treatments can also be administered in a variety of other forms, one of which is oral medication (via the American Cancer Society). Just like other cancer medication treatment, oral chemotherapy is often given in cycles, allowing healthy cells to recover while simultaneously giving time for the medication to work during this "rest" period. Oral cancer medication prescriptions may come in capsule, pill, or liquid forms.
The Dana-Farber Cancer Institute emphasizes that oral chemotherapy meds are just as strong as intravenous (IV) chemo medication. Following provider protocols is critical for safety. Your medical provider will make sure you have clear instructions on when and how to take oral chemo meds, which is important not only due to the medication's strength, but also because of the cost of the doses. Side effects of oral chemo (such as nausea or vomiting) are common but should be reported to your doctor.
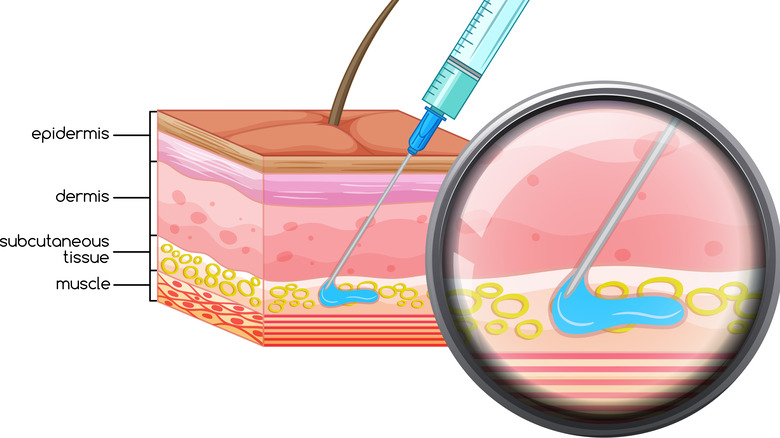
Subcutaneous chemotherapy injection
In October of 2022, the French National Centre for Scientific Research stated that a recent approach to subcutaneous chemotherapy may make it an increasingly realistic alternative to traditional intravenous chemotherapy. Subcutaneous chemotherapy means medication is injected into the tissue just under the skin, but not into veins or muscle. It's a simple process that doesn't require hospitalization the way IV therapy does. Unfortunately, because the ingredients that make chemo work are dangerous to the skin, subcutaneous chemo hasn't been used in the past, despite how much easier and more comfortable it could be for cancer patients. Researchers now know, however, that joining the active cancer ingredient paclitaxel with a water-friendly polymer can allow subcutaneous delivery to the bloodstream without causing skin irritation and toxicity. The Journal of the American Chemical Society has recently published research to this end, indicating that subcutaneous chemo could become a more common at-home cancer treatment in the near future. Early research has found subcutaneous chemo delivery to be more effective at fighting cancer than IV delivery in mice.
Intramuscular chemo injection
Intramuscular (IM) injection means that a substance or medication is injected directly into muscle tissue. Intramuscular chemotherapy is typically injected into the arm, upper leg, or glute muscle (via the Leukemia & Lymphoma Society). The frequency of the injections may range from weekly to a couple during a month, depending on your specific case and needs. As with other types of cancer drug treatments, intramuscular chemotherapy is sometimes given in cycles, with patients going on and off the medication in alternating spans (via Drugs.com). This allows healthy cells to suffer minimal impact. Intramuscular chemo shots may be administered at home or in a clinic. A medical professional may need to administer the medication injections, or a caregiver may be specially trained to provide intramuscular chemotherapy injections in a home setting. Chemotherapy in general, including intramuscular chemo, can cause a variety of side effects. Sometimes, IM chemo can cause pain at the site of drug injection. Be sure to discuss concerns with your medical provider.
Intravenous chemotherapy
Intravenous (IV) chemotherapy is a common form of cancer treatment (via the Leukemia and Lymphoma Society). Intravenous chemo is delivered directly into the bloodstream via a needle inserted into a vein, and is administered by a medical professional. This is the stereotypical chemo treatment we so often see in film. Because irritation of the veins can occur with repeated injection, a central line or catheter is sometimes used to deliver drugs more comfortably. A port, a kind of catheter meant for long-term use, is another delivery option. A port is usually placed under the skin of the chest and is used not only for drug delivery, but also sometimes for blood draws and nutrition.
Intravenous chemo can be given through IV push, IV infusion or continuous infusion (via Drugs.com). IV push involves meds provided via syringe over the course of only a few minutes. Intravenous or IV infusion is what most people imagine when they picture chemotherapy, and is typically provided over minutes or hours from a plastic bag of chemotherapy solution, through tubing and into a catheter site. IV infusion is sometimes regulated by an electric IV pump. Continuous infusion is the same, except that it may last for one to several days.
Intraventricular or intrathecal chemo
The human body's blood-brain barrier blocks many traditional chemotherapy medications from crossing into the cerebrospinal fluid, or CSP, explains an article published in Critical Reviews in Oncology/Hematology. For brain cancer treatment, intraventricular chemotherapy or intrathecal chemotherapy may be prescribed for this reason — because these methods of delivery can allow chemotherapy medications to reach cancer cells in the brain or spine. A surgical technique called Ommaya reservoir insertion can effectively facilitate the delivery of chemo drugs into the intraventricular cerebrospinal fluid (via the Canadian Journal of Neurological Sciences). The Ommaya reservoir device is implanted under the scalp. An attached catheter leads chemo meds into the ventricle of the brain so that it can infuse into the CSP. With intrathecal chemotherapy, the chemotherapy drugs are able to pass the blood-brain barrier via being directly injected into the spinal fluid (via Critical Reviews in Oncology/Hematology). Chemotherapy drugs circulate in the cerebrospinal fluid around the brain and spinal cord, where they can then kill cancer cells that typical, systemic chemotherapy cannot access.
Intraperitoneal chemotherapy
If you've ever taken a college anatomy and physiology class and had to do a mammal dissection, you might recall the peritoneum, a thin layer of tissue lining the abdominal cavity. When cancers develop in the abdomen — for example in the ovaries, stomach, or appendix — intraperitoneal chemotherapy is sometimes employed (via Massachusetts General Hospital). Intraperitoneal chemo (IP) is provided in a hospital or clinic, and allows cancer-killing drugs to be infused directly into the area of concern (the abdomen, or more specifically, the intraperitoneal space) as opposed to traveling through the body systemically via injection into the veins. The chemo is delivered into the body through a port in the abdomen.
Intraperitoneal chemotherapy is often prescribed for ovarian cancer, in conjunction with surgery (via the American Cancer Society). IP chemo may be used if the number of remaining cancer cells is fairly small. The chemo will be absorbed into surrounding tissues, which is important to ensure treatment of other nearby areas where the cancer may have spread. Since IP chemo utilizes a stronger concentration of anti-cancer medication, it may cause local side effects such as nausea, abdominal pain, appetite loss, vomiting, or kidney damage.
Intra-arterial chemotherapy treatments
Intra-ocular retinoblastoma is a type of cancer mainly seen in young children (via the American Cancer Society). It's typically diagnosed after a doctor or caregiver notices that the child's eye looks discolored or vision is impaired. Intra-arterial chemotherapy (IAC) is a method of treating retinoblastomas where chemo drugs are sent into the eye (via World Eye Cancer Hope). A tiny catheter inserted into the femoral artery in the groin while the child is under general anesthesia. Chemo drugs are delivered through the catheter into the ophthalmic artery. Only specialized clinical settings will offer intra-arterial chemotherapy, since it can present some serious risks. Child cancer patients who are navigating retinoblastoma can benefit from intra-arterial chemotherapy, which provokes none of the classic cancer side effects associated with IV chemo, since the drugs are delivered locally into the eye instead of systemically. Benefits and costs must be weighed carefully by the child's medical team, however. Potential risks to the child include retinal detachment, ophthalmic artery spasm, bleeding or loss of blood supply to the eye, or permanent vision loss. Less serious or temporary side effects may include issues such as drooping or swollen eyelids. Extra blood may collect in the forehead as well.
Intravesical chemotherapy
The Centers for Disease Control and Prevention (CDC) report that around 57,000 American men and 18,000 American women are diagnosed with bladder cancer every year. Researchers have found that bladder cancer risk factors include smoking and exposure to specific environmental chemicals. Smoking is a primary contributing factor, but genetic factors can also contribute to risk.
Intravesical chemo is a form of cancer treatment drug delivery where a catheter is utilized to carry medication directly into the bladder (via the American Cancer Society). Sometimes hyperthermic intravesical therapy is used, meaning that the chemotherapy solution is first heated to improve efficacy. In general, intravesical chemo is an option that cancer doctors use after intravesical immunotherapy is unsuccessful, or if the cancer has grown to a more advanced stage by the time of diagnosis. Common chemo side effects are largely avoided because this is a direct delivery method — drugs are sent straight into the bladder instead of traveling through the entire body. Side effects that are most commonly reported include sensations of burning or discomfort in the bladder, or sometimes blood in the urine.
Intrapleural chemotherapy
According to the American Cancer Society, when chemotherapy is administered directly into the chest cavity or pleural cavity, it's called intrapleural chemotherapy treatment. This kind of chemotherapy might be chosen if the cancer is located in the chest — for instance, mesothelioma or thymoma might be targeted with intrapleural chemotherapy (via University of Miami). A small catheter is inserted into a minor incision in the chest wall — the medication is inserted here and will end up circulating both through the chest and in the bloodstream (per the American Cancer Society). As with intraperitoneal chemo, intrapleural chemotherapy drugs are also sometimes warmed before administration (hyperthermic chemotherapy). This is most frequently prescribed post-surgery, and it is thought that the higher medication temperature increases the effectiveness of the medication.
Many patients receive intrapleural chemo in combination with IV chemo or other treatments (via University of Miami). Heated chemotherapy medication is given for a period of up to two hours, and is then cleared out of your body with a sterile solution. Like other more targeted forms of chemotherapy, intrapleural chemotherapy is known to provoke fewer side effects than systemic treatments.
Implantable chemotherapy
Brain cancers can be uniquely difficult to treat, since the blood-brain barrier blocks many forms of medication (via Columbia University Irving Medical Center). Neurosurgical researchers at Columbia University and New York-Presbyterian have recently tackled this issue with a new and innovative medical technology, the implantable chemotherapy pump. Although this treatment approach is still being researched, developed, and refined, it may be a game-changer in treating brain cancer. It would allow small amounts of chemo drugs to be released directly into the brain with minimal side effects.
Another chemo pump technology, originally developed at the University of Michigan, was innovated for the treatment of tenacious liver cancers (via University of Michigan). A Journal of Clinical Oncology research review found that patients with such implantable chemotherapy pumps lived two years longer than similar patients with none. The Gliadel wafer is another example of implantable chemotherapy (via Chemocare). After surgical removal of glioblastoma multiforme brain tumors, several dime-sized, dissolvable wafers are implanted. As the wafers dissolve, they release chemotherapy into the brain tissue over the course of weeks, killing residual cancer cells.
Topical chemotherapy
According to the National Cancer Institute, topical chemotherapy is defined as "treatment with anticancer drugs in a lotion or cream applied to the skin." Skin cancers such as cutaneous squamous cell carcinoma, basal cell carcinoma, and melanoma are often treated through surgical removal (via the Advanced Drug Delivery Review). In some cases, however, topical chemotherapy may be one of the more appropriate or effective treatments for skin cancer. Strong chemical drug treatments can be applied superficially, treating skin tumors directly with less toxic side effects than systemic chemotherapy.
The Skin Cancer Foundation advises that the two leading causes of skin cancer are sun exposure and tanning bed use, since ultraviolet (UV) rays can trigger reactive cellular changes. DNA damage caused by UV rays can create mutations in skin cells that eventually turn into tumors. For this reason, avoiding harsh sun exposure, sunburn, and UV tanning bed use can help you prevent skin cancers. Sunscreen use is also preventative.
Cancer prevention tips
If you have any concerns about skin cancer or any other type of cancer due to family history or symptoms, talk to your healthcare provider. According to the American Cancer Society, evidence-based screenings are important for reducing your cancer risk and maintaining a healthy body. Talk to your doctor about any concerning symptoms and maintain regular checkups with primary care, and be sure to promptly schedule any screenings recommended by your doctor. Your family doctor may also educate and empower you with preventative health education on topics such as what aerobic exercise can do for your cancer risk, how to do a self breast exam, and foods that may help you prevent cancer. Research indicates that several lifestyle factors contribute to cancer risk, including long-term, chronic stress, use of alcohol and tobacco, the consumption of certain foods (such as fried items and red meat), a sedentary lifestyle, and exposure to radiation (such as sunlight). Be sure to ask your doctor for more information to aid in cancer prevention and healthy lifestyle, in order to build the healthiest future possible.