Why The Left Side Of Your Head Hurts
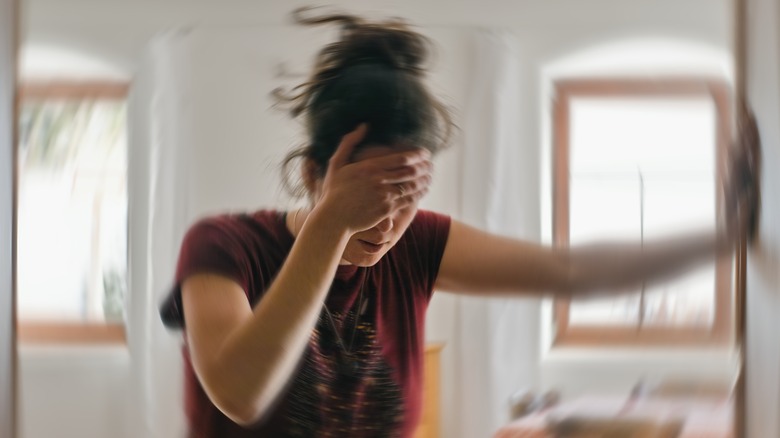
Whether it's a dull throb, a sharp sting, or a persistent ache, pain on the left side of your head can be alarming. Your head and face are comprised of an intricate maze of nerves, muscles, and blood vessels, and pain can arise from a disturbance of any one of these structures. Headaches or facial pain are most often benign and short-lived, however uncomfortable they may be. Tension headaches and sinus problems are some of the most common causes, along with migraines and cluster headaches. Underlying health conditions affecting the nerves, blood vessels, and brain are less common but more serious.
For some people, left-sided head pain is an acute, isolated experience; for others, it may happen more regularly and lower their quality of life. If the pain is a headache, you might wonder if your brain is affected. But don't jump to conclusions. Understanding the various causes of head pain can provide peace of mind and guide potential interventions, or guide you to visit your doctor for a more comprehensive assessment.
Migraines
A migraine usually feels like a pounding headache on one side, although it can impact both sides too. This headache can last from a few hours to days, making it tough to carry on with regular activities. Along with the pain, some people might have blurry vision, or feel sensitive to lights, noises, and smells; others might even feel sick or throw up (via the National Institutes of Health). Some get a kind of heads-up called an "aura" before a migraine hits, which can make them see light flashes or wavy patterns.
Scientists are still trying to determine what causes migraines, but they believe it has something to do with changes in brain activity that affect how nerves talk to each other and can even change chemicals and blood flow in the brain. Several things, like hormone changes, certain foods, stress, or even the weather, can cause a migraine. Migraines often start when people are teenagers or young adults. They're more common in women than in men, and if other people in your family have them, you might be more likely to get them too.
To handle migraines, it helps to know what triggers yours and try to avoid those things. Some changes in your daily habits and sometimes medication, which a doctor prescribes, can help. There are different kinds of medications: some you take when you have a migraine to help with the pain, and others you take regularly to prevent them from coming on so often or being so severe.
Cluster headaches
Cluster headaches are a series of relatively short but extremely painful headaches. Unlike migraines, which can last for hours or days, cluster headaches typically last between 30 and 45 minutes (via the Mayo Clinic). These headaches strike quickly, without the warning signs that some other types of headaches might have. A person may experience these headaches daily for weeks or even months, followed by a headache-free period that can last months or even years.
What's distinctive about cluster headaches is their pattern. During a cluster period, headaches usually occur at the same time each day. For instance, people might always get them in the early morning or at night. They often awaken people from sleep. The pain of a cluster headache is intense and is usually felt around one eye or on one side of the face. Symptoms can include a tearing or bloodshot eye, a drooping eyelid, facial sweating, or a runny nose –- all occurring on the same side as the pain.
The exact cause of cluster headaches is still unclear. However, their regular occurrence suggests they might be related to the body's biological clock, which is regulated by the hypothalamus. Moreover, factors like alcohol consumption can trigger a cluster headache in many people during a cluster cycle. Men are more likely to suffer from cluster headaches than women. Smoking or having a family history of cluster headaches also increases the risk. If you experience cluster headaches, seeking medical advice is crucial, as the pain can diminish your quality of life.
Sinus infection
Approximately 28 million Americans experience sinus infections in any given year (via Teledoc Health). Pressure and pain in the forehead, cheeks, or between the eyes are the most common symptoms. Sinuses are air pockets inside the head that can sometimes become inflamed or clogged, leading to the pain known as sinusitis. Pain may be on both sides of the head or just one side. Multiple factors, like allergies, colds, or chronic conditions, can trigger sinus infections.
The inflammation is the primary reason behind the discomfort. When sinuses swell, they prevent mucus from flowing freely. This stasis creates a breeding ground for bacteria, which can lead to infections. As a consequence, the buildup of pressure in the sinuses intensifies, and pain ensues. Other symptoms that may occur along with sinus pressure and pain include a stuffy or dripping nose, fatigue, a diminished sense of smell, or even an ache resembling a toothache. For those with severe conditions, they might even exhibit signs like fever, persistent coughing, or unpleasant breath.
Often, the pain fades with time or with basic remedies from the drugstore, but it's important to know when it's time for a doctor's opinion. If your discomfort persists for over seven days or is particularly intense, consider getting expert insights. Frequent or long-lasting sinus problems might hint at an underlying issue that requires a specialized approach to treatment. Being proactive in seeking medical advice can expedite recovery and alleviate pain.
Occipital neuralgia
Occipital neuralgia is a specific kind of headache that results in sharp, aching, or shock-like pain in the upper part of the neck, the back of the head, and behind the ears. Generally, this pain is on one side, but sometimes both sides can be affected. The main culprit behind this pain is the irritation or damage to the occipital nerves, which extend from the upper spinal cord to the scalp (via the American Association of Neurological Surgeons).
Various factors can contribute to occipital neuralgia. It could be due to physical stress, an injury to the back of the head, tension in that region, or a pinched nerve. Certain medical conditions, like osteoarthritis, tumors, infections, inflammation, diabetes, gout, and cervical disc disease, can also be responsible. Primary occipital neuralgia is when it's a standalone condition; secondary occipital neuralgia is linked to an underlying health condition.
Diagnosing the condition can be challenging because its symptoms often overlap with other headache conditions like migraines. To determine if someone has occipital neuralgia, doctors typically rely on physical and neurological examinations. Imaging, such as MRIs and CT scans, may also be utilized. Once diagnosed, treatments can range from simple measures like rest, warm compresses, and anti-inflammatory drugs to more advanced approaches like nerve or spinal cord stimulation surgery. If you suspect you have this condition, it's vital to seek medical advice for the right diagnosis and treatment.
Hemicrania continua
Hemicrania continua is a rare type of chronic headache that consistently affects only one side of the head. From Latin, its name essentially means "continuous one-sided headache" (via the Cleveland Clinic). Those who suffer from this condition endure constant pain that varies in intensity.
The symptoms include ongoing mild pain with sporadic bursts of more intense pain. These intense spells can feel like migraines and can last anywhere from 20 minutes to several days. Alongside this intensified pain, some may also experience eye pain, a drooping eyelid, tearing, a stuffy nose, eye redness, all of which will occur on the same side as the pain. Other symptoms can include nausea, vomiting, and a sensitivity to loud noises or bright light.
The exact cause of hemicrania continua remains a mystery, but certain factors, such as physical exertion and consuming alcohol, may amplify the pain (via Healthline). Timely diagnosis and treatment are vital given the ongoing nature of this headache. The most effective treatment is a type of non-steroidal anti-inflammatory drug (NSAID) called indomethaci. In fact, it's so effective that a strong positive reaction to indomethacin is used to confirm a diagnosis of hemicrania continua. However, due to potential side effects from prolonged use of indomethacin, doctors might suggest other treatments or medications to manage the pain if indomethacin is not well-tolerated.
Giant cell arteritis
Giant cell arteritis, commonly known as temporal arteritis, is a condition where the arteries, particularly those at the temples, become inflamed. The pain is typically localized to one side of the head (via Penn Medicine). The cause of giant cell arteritis has not been determined. However, it is understood that the condition involves the immune system attacking the body's arteries, leading to inflammation (via Nord). This inflammation can result in reduced blood flow, which in some cases can cause severe complications.
Symptoms of temporal arteritis vary, but often include a severe and continuous headache, tenderness of the scalp or temples, jaw pain while eating, blurred or double vision, and sometimes even complete vision loss. Such vision problems arise because the reduced blood flow affects the health of the eyes. Other symptoms might include fatigue, loss of appetite, fever, unintentional weight loss, and soreness and stiffness in the neck, hips, shoulder, and upper arm.
Temporal arteritis is most commonly diagnosed in people over the age of 50, and it appears to be more common among women and people of northern European and Scandinavian descent (via the Mayo Clinic). It can also be genetic. Given the potential severity of the condition, especially the risk of irreversible vision loss, it is crucial to consult a healthcare professional when symptoms arise. Treatment generally involves medications that reduce the inflammation of the arteries. Early diagnosis and prompt intervention are necessary to manage the condition effectively and prevent any long-term complications.
Trigeminal neuralgia
Trigeminal neuralgia (TN) is a severe and chronic pain condition affecting the trigeminal nerve. There are two trigeminal nerves on either side of the head, but TN typically only affects one. The condition leads to extreme, sporadic, sudden burning or shock-like facial pain that lasts from a few seconds to a couple of minutes per episode (via NHS). These attacks can occur in quick succession for days, weeks, or months.
The trigeminal nerve has three branches that control the sensations of the face, transmitting signals to the brain from the upper, middle, and lower portions of the face, as well as the oral cavity. The onset of TN pain is typically caused by a blood vessel pressing on the root of the nerve, triggering the malfunction. In some cases, the cause could be related to a tumor or multiple sclerosis.
TN typically affects people aged 50 and older, and it's more common in women than men. TN can go into remission, which means patients might experience no pain for long periods, sometimes even for years.
Dental traumas may be linked to TN. However, the symptoms of TN should not be confused with dental pain, which leads many to consult with dentists and undergo unnecessary dental procedures before the proper diagnosis is made (via John's Hopkins Medicine). Treatment for TN varies and can include medications, injections, or surgery. The primary goal is to find the most effective way to manage pain with the least number of side effects, enhancing the individual's quality of life.
Bell's palsy
Bell's palsy is a sudden and temporary facial weakness or paralysis affecting one side of the face, caused by inflammation or damage to the facial nerve (via the Mayo Clinic). The cause of the condition isn't fully understood, but it is believed to be an immune response and is often associated with viral infections. Many people who develop Bell's palsy have recently experienced symptoms of viral infections, like the flu or a cold. People who are pregnant, have diabetes, high blood pressure, or obesity are at an increased risk of developing Bell's palsy.
The symptoms of Bell's palsy usually emerge quite rapidly. The main sign is an unexpected weakness or paralysis on one side of the face, causing difficulty shutting the eye or mouth on the affected side. Other symptoms might include drooling, heightened sensitivity to sound in one ear, headaches, loss of taste, and pain near the jaw or behind the affected ear.
If you notice sudden facial drooping or weakness, it's essential to consult a doctor immediately to rule out severe conditions like a stroke. While there isn't a universal treatment approach for Bell's palsy, medications can help reduce inflammation and swelling. Some people might also benefit from physical therapy exercises to stimulate their facial muscles.
While the sudden onset of Bell's palsy can be distressing, the condition is often temporary, and most people fully recover within a couple of weeks to six months. Immediate medical attention and treatment can enhance the chances of a successful recovery.
Stroke
A stroke is one of the more severe causes of pain on one side of the head, and it is not something to take lightly. A type of stroke called a hemorrhagic stroke, which causes bleeding into the brain, is most likely to cause headaches (via Nebraska Medicine). Pressure causes blood vessels in the brain to weaken and rupture, which causes pain on one side or both sides. The pain can be severe and produce what is commonly referred to as a "thunderclap" headache. Unlike regular headaches or migraines, the onset of a thunderclap headache is sudden and rapid, and it is intensely painful.
In addition to a severe headache, other symptoms often accompany a stroke, including confusion, dizziness, difficulty speaking, visual disturbances, and weakness or numbness on one side of the body. It is this combination of symptoms that can help distinguish a stroke-related headache from other types of headaches. Certain people are at increased risk of hemorrhagic stroke, including people with high blood pressure, older people, and those who smoke or drink excessive amounts of alcohol.
Strokes are a much less common cause of head pain, but it's important to recognize the signs of a stroke and seek immediate medical attention if you experience them. Rapid intervention can make a significant difference in treatment outcomes and recovery potential.
Brain aneurysm
One of the most serious causes of one-sided head pain is a brain aneurysm, which is also one of the causes of hemorrhagic stroke (via the Mayo Clinic). A brain aneurysm is a bulge or ballooning in a blood vessel within the brain. Although many small brain aneurysms exist without causing complications, if one leaks or ruptures, it can pose significant health risks. Larger unruptured aneurysms can put pressure on brain tissues and nerves, potentially causing vision problems, pain above and behind one eye, dilated pupils, and numbness or weakness on one side of the face.
The symptoms of a ruptured brain aneurysm are immediate and severe, including a sudden and extremely painful headache. This may be accompanied by nausea, vomiting, a stiff neck, blurred or double vision, seizures, drooping eyelids, sensitivity to light, confusion, and loss of consciousness. The cause of a brain aneurysm is not always clear, but there are factors that can increase the risk, including genetic conditions, untreated high blood pressure, and atherosclerosis, which is the thinning of the blood vessel walls.
Ruptured brain aneurysms are rare, but they are serious. According to the Brain Aneurysm Foundation, 50% of people who experience ruptured aneurysms die, and 66% of survivors experience permanent neurological alterations. If you or someone you know experiences symptoms associated with a ruptured brain aneurysm, it's crucial to seek emergency care immediately.