IBS Explained: Causes, Symptoms, And Treatments
Irritable bowel syndrome, commonly referred to as IBS, is a gastrointestinal disorder that causes abdominal discomfort as well as changes to one's daily bowel habits. According to the Cleveland Clinic, there are three different types of IBS: IBS-D, IBS-C, and IBS-M. In people with IBS-D, chronic diarrhea is the most prominent symptom, while those with IBS-C deal with chronic constipation. People with IBS-M alternate between chronic diarrhea and chronic constipation.
IBS is a fairly common disease. According to the International Foundation for Gastrointestinal Disorders (IFFGD), between 10 and 15% of the world's population has IBS. In the United States, between 25 and 45 million people, or 7.5-13% of the population, have the disease. Per the IFFGD, though IBS is common, many people don't seek out medical attention for their symptoms because they're uncomfortable discussing their bowel habits with their doctor. Because of this, many patients deal with their symptoms for years before getting a definitive diagnosis and subsequent treatment. For this reason, recognizing the symptoms of IBS and knowing how to pursue treatment options is crucial for getting a diagnosis and combating the symptoms.
The most common symptoms of IBS
IBS includes a wide range of symptoms, per the UK's National Health Service (NHS). Not everyone experiences the same symptoms, and the severity of the symptoms varies. Some people experience mild but persistent discomfort. For others, IBS is debilitating.
The most common symptoms of IBS are gassiness, bloating, abdominal cramps, stomach cramps, and changes in your bowel movements. Gassiness occurs when excess gas builds up in the gut (per Medical News Today). This can manifest as gurgling sounds in your stomach or gut, abdominal or stomach cramps, bloating, or farting a lot. Severe gas buildup can cause pain in the chest and shoulders. Bloating is often described as a feeling of being "too full," or pressure in the abdomen (via the NHS). Abdominal and stomach cramps refer to sharp, dull, or achy pain in the stomach or lower abdomen (via Cleveland Clinic). This pain is often the result of gas buildup.
IBS also causes a marked change in your bowel movements (per NHS). Some people experience diarrhea, while others experience constipation. Though occasional diarrhea and constipation are normal, experiencing either of these symptoms for an extended period of time is not normal, and is often a sign of IBS or another digestive disease (via Mayo Clinic). Many of these symptoms occur soon after eating and are relieved after a bowel movement. However, some people with IBS experience these symptoms pretty much all the time.
Less common symptoms of IBS
Some people with IBS have additional symptoms that perhaps aren't obviously related to the gut. Though these symptoms are less common, many people with IBS will experience them at some point. According to the NHS, these symptoms include: fatigue, backache, and bladder issues. According to Science Direct, fatigue is a particularly common symptom — more than 50% of people with IBS experience fatigue at some point. And according to a study published in the medical journal BJUI, between 9 and 20% of people with IBS also experience bladder problems including an urgent need to urinate, feeling like they can't empty their bladder, waking in the middle of the night to urinate, and loss of bladder control.
Like chest and shoulder pain, back pain can also be caused by gas or gastrointestinal dysfunction. Though the majority of patients with IBS experience back pain, per a study published in Gut, their pain isn't usually recognized as a symptom of IBS.
Risk factors for IBS
According to the IFFGD, women are more likely to have IBS than men — in fact, two-thirds of people with IBS are women. People younger than 50 are more likely to get the disease than those who are older. However, people of all ages get IBS, including children.
Some people are also more likely to get IBS based on their life circumstances or their medical history, according to the National Institutes of Health. For instance, someone who has a family member with IBS is more likely to develop IBS themselves. Contracting a severe intestinal infection also puts people at risk for developing IBS. And according to the Mayo Clinic, people with mental health issues, especially depression and anxiety, are more likely to get IBS. Experiencing severe adverse life events — such as domestic violence, sexual assault, emotional abuse, and other trauma — also ups someone's risk for developing the condition.
What causes IBS?
Doctors and researchers still haven't identified exactly what causes IBS, according to the IFFGD. However, they widely agree that gut sensitivity is part of the cause. In people with the condition, things like stress, eating certain foods, gastrointestinal infections, hormonal changes, gas, and stool formation trigger muscle contractions in the gut that lead to the common symptoms of IBS.
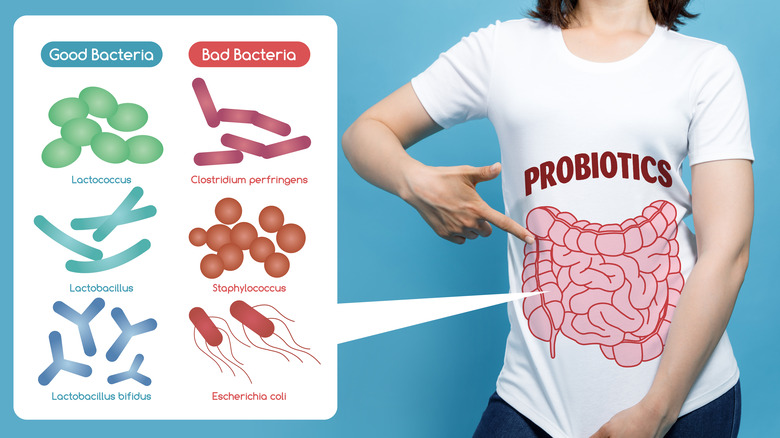
Many professionals who've studied IBS believe that the increased gut sensitivity is due to miscommunications between the brain and the gut. Proper gut function relies on signals from the brain to the gut, and vice versa. When this communication is disrupted, the gut becomes more reactive. Still other doctors and researchers believe that IBS may be caused by an imbalance in the gut bacteria. Most of the bacteria in our guts are "good" bacteria that help regulate our digestive functions. However, "bad" bacteria can grow in the gut as well, disrupting the gut's ability to break down food into waste, which can lead to the common symptoms of IBS.
How IBS impacts quality of life
Research has determined that having IBS can have a significant negative impact quality of life. One 2018 study conducted found that people with IBS experience depression at a much higher rate than those who don't have IBS — about 13% of the study participants had depression so severe they needed to be hospitalized (via Przeglad Gastroentologiczny). Similarly, an earlier study found that patients with IBS rated their quality of life lower than people without IBS, with the severity of a patient's symptoms directly correlating to a decrease in quality of life.
In 2015, the American Gastroenterological Association conducted a survey on people with IBS to determine how their symptoms impacted their daily lives. This survey found that 22% of the respondents couldn't predict when their symptoms would interfere with their daily lives. It also found that people with IBS had trouble adequately doing their jobs an average of nine days every month because of their symptoms, and that they missed work or school due to the condition. Three quarters of the respondents were "frustrated or depressed" because of their symptoms. Unfortunately, the fatigue, pain, and GI symptoms associated with IBS can make it difficult for sufferers to fully participate in life the way they want to.
Diagnosing IBS
Unfortunately, getting diagnosed with IBS can be a difficult process because there is no test for the disease (via Mayo Clinic). According to the NIH, diagnosis is based on an analysis of your medical history and long-term symptoms, and on ruling out other potential conditions or infections that can cause similar symptoms. The first symptom doctors look for when diagnosing IBS is abdominal pain. However, abdominal pain by itself isn't necessarily indicative of IBS — so doctors look for a combination of abdominal pain with another classic IBS symptom such as a change in the number of bowel movements you have each day, or a change in the appearance of your poop. If you've started to have loose stools, diarrhea, or constipation multiple times a week, that could also indicate IBS. When you have one or both of these symptoms combined with abdominal pain, your doctor may diagnose you with IBS.
However, the frequency and persistence of your symptoms is also a key part of diagnosing IBS. To warrant an IBS diagnosis, your symptoms need to occur at least once a week for at least six months. However, if your symptoms are severe and fairly frequent, your doctor may diagnose you with IBS before the six-month mark.
Is it IBS or something else?
Another complication in the treatment of IBS is that several other gastrointestinal diseases share similar digestive symptoms. According to WebMD, ulcerative colitis, microscopic colitis, and Crohn's disease are often misdiagnosed as IBS. All of these conditions are caused by inflammation in the digestive system. In addition, food allergies and sensitivities, especially lactose intolerance and Celiac disease, can be mistaken for IBS. Lactose intolerance occurs when the digestive system can't break down lactose, a sugar found in dairy products. Though it doesn't harm your digestive system, it does cause very uncomfortable symptoms. Celiac disease, in contrast, does damage to your digestive system. With Celiac disease, your immune system responds to gluten as a foreign invader, so it attacks your digestive system when you eat gluten.
Other conditions like diverticulitis, pancreatitis, gallstones, endometriosis and Small Intestinal Bacterial Overgrowth (SIBO) can also look similar to IBS. Because a number of conditions share overlapping symptoms, your doctor may need to perform blood, stool, or other tests to rule out these possibilities before making a diagnosis (per Mayo Clinic).
Comorbidities with IBS
According to IFFGD, several other digestive diseases or symptoms can occur alongside IBS. Dyspepsia (an umbrella term for digestive pain felt under the rib cage) and heartburn are commonly experienced by those with IBS. Inflammatory bowel diseases like Celiac disease, ulcerative colitis, and microscopic colitis — which often get misdiagnosed as IBS — can also co-occur with IBS. When you have both an inflammatory bowel disease and IBS, it can be very difficult to figure out which condition is causing your symptoms, making it hard to determine the proper treatment.
IBS also commonly co-occurs with several non-GI illnesses. For reasons that haven't yet been identified, people with IBS often also have fibromyalgia, interstitial cystitis (painful bladder syndrome), migraines, chronic pelvic pain, or Myalgic Encephalomyelitis (chronic fatigue syndrome). Many people with IBS experience more than one co-occurring illness. For example, one person might have IBS, ulcerative colitis, and migraines.
According to a research article published in The Annals of Family Medicine, the reasons why certain conditions occur together are complicated and often can't be determined. Sometimes multiple chronic conditions occur together because they both have the same common cause, like a systemic autoimmune illness. However, multiple chronic conditions can also occur together by chance.
IBS and SIBO
SIBO (small intestinal bacterial overgrowth) occurs with IBS so often that doctors and researchers have begun to investigate whether SIBO causes IBS, whether IBS causes SIBO, or whether both diseases have a common cause. According to a study published in the medical journal Gut and Liver, as many as 78% of patients with IBS also have SIBO.
SIBO happens when the balance of bacteria in the small intestine is disrupted, according to the Mayo Clinic. Typically, a specific event, like a surgery or disease, slows down the digestion of food in the small intestine. When the food is stuck in the small intestine for too long, bacteria begins to proliferate — including bacteria that doesn't actually belong in the small intestine. This knocks the balance of bacteria in your gut all out of whack, leading to very uncomfortable GI symptoms.
Many doctors now believe that SIBO plays a factor in the development of IBS. Often, people who undergo treatment for SIBO also experience a marked improvement in their IBS symptoms. So, if you've been diagnosed with IBS, getting tested for SIBO is a good idea. SIBO can be diagnosed with a breath test, or by testing a sample of the small intestinal fluid via an endoscopy.
Treatment for IBS
Since IBS is a fairly common disease, your primary care provider (PCP) should be able to diagnose you and work with you on an initial treatment plan, according to Verywell Health. That said, your PCP might not be the best fit to address IBS long term. IBS is widely misunderstood, and many providers aren't quite sure how to approach treatment. If your provider doesn't feel like they have the expertise necessary to guide your treatment, they can refer you to a gastroenterologist.
There is no definitive treatment that works for every IBS patient. According to Johns Hopkins Medicine, each person requires an individualized plan that may combine multiple approaches. Many doctors may recommend starting with dietary changes, lifestyle changes, and mental health treatment, though medication may be prescribed if symptoms can't be managed through these means alone. Because there's no cure for IBS, the goal of treatment is to manage symptoms and improve quality of life (via MedicineNet). Working with a treatment team — which may include your PCP, a gastroenterologist, a nutritionist, and mental health professionals — you should be able to devise a treatment plan that effectively manages your symptoms.
Dietary changes for IBS
Though dietary changes are often a major part of IBS treatment, there's no "IBS diet" that will help every person, per the NIH. Each body is unique and has its own sensitivities, so each person has to figure out what diet works for them by making changes over an extended period of time. However, some food triggers are so common among IBS patients that your doctor may advise reducing or eliminating them. For instance, doctors often recommend cutting out gluten and/or dairy, which cause flare-ups in some IBS patients. Eating more fiber is also key, as it can help keep bowel movements consistent and less painful. However, it's important to add fiber gradually, because too much fiber too quickly can lead to gas and bloating.
For many with IBS, the low-FODMAP diet can ease symptoms and help them identify the food triggers they should avoid. According to Johns Hopkins Medicine, FODMAP stands for "fermentable oligosaccharides, disaccharides, monosaccharides and polyols." These are all short-chain carbohydrates that can be difficult for our digestive systems to process, leading to uncomfortable symptoms like gas, cramping, constipation, and diarrhea. The low-FODMAP diet involves cutting out foods that contain these short-chain carbohydrates for a short period — typically between two and six weeks — and then slowly reintroducing foods to see if symptoms return. If a given food causes a flare-up, it should be limited or cut out entirely.
Medications for IBS
According to John Hopkins Medicine, several medications, both over-the-counter and prescription, are often included in a treatment plan for IBS. For those dealing with constipation, laxatives and muscle relaxants may be beneficial. For those dealing with loose stools or diarrhea, antidiarrheal medications might help. Some patients also get relief from antibiotic therapy because it helps balance the bacteria in the gut, which could be the root of the problem. Low-dose antidepressants may also help because they help manage stress and anxiety, and they can assist in making the gut less reactive to triggers.
The Mayo Clinic states that fiber supplements and anticholinergic medications can help to regulate and soothe your gut, and pain medications can bring relief from symptoms like bloating that cause discomfort.
If none of these medications provide symptom relief, your doctor may prescribe a medication specifically for IBS like Alosetron (Lotronex), Eluxadoline (Viberzi), Rifaximin (Xifaxan), Lubiprostone (Amitiza), and Linaclotide (Linzess), all of which can aid in the digestive process.
Lifestyle changes and mental health treatments for IBS
Lifestyle changes and mental health treatment are essential parts of an IBS treatment plan, according to the IBS Network. One study published in the medical journal Gut and Liver examined the impact of lifestyle changes such as managing stress, quitting smoking, avoiding alcohol, and exercising on IBS symptoms. At the end of the nine-week study, participants reported significantly reduced stress and pain levels and rated their overall quality of life higher.
Since mental health has a major impact on digestive functioning (per Harvard Health), addressing mental health issues is also crucial to IBS treatment. Per WebMD, multiple forms of therapy can be helpful, including traditional talk therapy, cognitive behavioral therapy (CBT), hypnotherapy, and biofeedback sessions. Many people also find that implementing a meditation practice or undertaking relaxation techniques — such as getting a massage — can aid in managing stress, which can lead to symptom improvement (per WebMD).