Flu Explained: Causes, Symptoms, And Treatments
Before the era of COVID-19, the respiratory ailment people tried their hardest to avoid was influenza (the flu), and there's good reason for that. Even a mild case of the flu can leave you feeling miserable for days, and for some, the infection can be extremely dangerous or even deadly.
According to the Centers for Disease Control and Prevention (CDC), influenza and its complications killed almost 50,000 Americans in 2019, making it the ninth leading cause of death that year — and that was a relatively "light" flu season. Because the virus that causes influenza mutates easily, creating new strains each year, each flu season varies in terms of how many people get sick, how many are hospitalized, and how many die. The CDC noted that between the 2010-2011 and 2019-2020 flu seasons, annual cases in the United States ranged from a low of 9 million (during 2011-2012) to a high of 41 million (during 2017–2018).
One silver lining of the COVID-19 pandemic was that mask-wearing, improved hand hygiene, and social distancing made for a virtually nonexistent flu season in the winter of 2020–2021 (via Advisory Board). While the measures put in place to slow the spread of COVID-19 may have inadvertently also temporarily put the kibosh on the flu, influenza has a long history of causing pandemics of its own. Sudden, widespread outbreaks of the flu are substantially more dangerous than the seasonal flu and pose a significant public health risk.
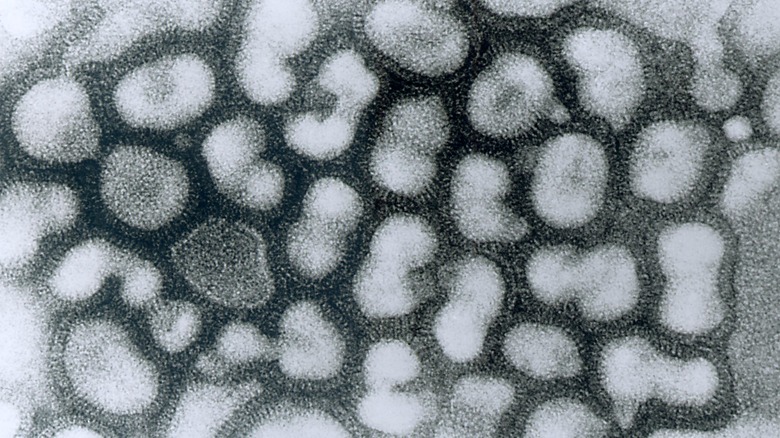
The viruses that cause influenza
Most people know that influenza is caused by a virus, but that's just the beginning of the story. There are actually 4 types of influenza viruses: A, B, C, and D. Influenza type D primarily affects cattle and doesn't cause disease in humans. Influenza type C causes only mild illness in people. Influenza types A and B cause the seasonal flu, with type B producing a more mild illness. Influenza type A is of most concern since it causes the most severe cases of seasonal flu and can also cause pandemics. Influenza A viruses are classified based on 2 proteins (antigens) on the surface of the virus: hemagglutinin (H) and neuraminidase (N). There are 18 different hemagglutinin subtypes (H1 through H18) and 11 different neuraminidase subtypes (N1 through N11). Influenza type A viruses are further broken down into genetically distinct groups and sub-groups. Strains of H1N1 and H3N2 are responsible for the current seasonal flu (via the CDC).
Influenza has stuck around because of something called antigenic drift. Antigenic drift occurs when small mutations emerge in the genes of the virus that affect the H and N antigens on its surface. Every time a flu virus replicates, there's a chance for a small mutation to occur. Over time, these small changes add up, making the virus less recognizable to our immune systems. This means that even if you've had the flu before, antigenic drift allows you to get it again (via the CDC).
What about bird flu and swine flu?
Some influenza viruses also infect animals and, in rare cases, these strains can infect humans. In the case of bird (avian) flu, there are 12 strains of influenza A virus that infect wild and domesticated birds, with 2 of them (H5N1 and H7N9) occasionally causing infections in humans. In most cases, people have gotten bird flu from close contact with infected birds or from eating the meat or eggs of sick birds. Person-to-person transmission of bird flu has also been reported, but it's very uncommon. Symptoms of bird flu are similar to those of regular seasonal flu, but bird flu is much more likely to cause complications. In fact, more than half of those infected with bird flu will die of the disease. However, there have been fewer than 500 bird flu deaths worldwide since 1997 (via the Mayo Clinic).
Swine flu refers to a strain of the H1N1 influenza virus. In 2009, this particular strain (formerly found in pigs and birds) jumped to humans. Because it was new, H1N1 caused a greater-than-usual number of infections and deaths around the world, earning it pandemic status. Since then, however, it has become one of the two strains of influenza that cause seasonal flu and, because our immune systems and vaccines have had time to adapt, it's significantly less deadly than it was back in 2009 (via the Mayo Clinic).
Who gets the flu and its complications?
Anyone can get the flu, but certain individuals are at greater risk of being infected or experiencing complications. Individuals who live or work in places where there are many other people, such as a nursing home or prison, are at increased risk because such close contact means influenza can spread rapidly. People staying at the hospital for other reasons are also more likely than the general public to get the flu. People with weakened immune systems are less able to fend off influenza and more prone to complications. Obese individuals and pregnant women are also more likely to have flu complications. Chronic illnesses, especially respiratory conditions such as asthma, also put individuals at greater risk (via the Mayo Clinic).
However, age is one of the biggest risk factors when it comes to the flu. The still-developing anatomy of infants makes it much harder for congestion to drain properly, increasing the risk of complications. Their immune systems are also still maturing. Daycare settings can become hotbeds of flu activity, especially when you consider the less-than-stellar hygiene habits of young children. On the other end of the lifespan, elderly individuals, particularly those living in care facilities, are also at increased risk. Our immune systems weaken with age, and older individuals tend to have more pre-existing chronic conditions that can increase the likelihood of complications. In fact, between 71-85% of influenza-related deaths are among those 65 and older (via Northwestern Medicine).
The most common flu symptoms
Symptoms of the flu begin 1-4 days after infection with the virus and usually last 5-7 days. Individuals with weakened immune systems may experience symptoms for longer, while those who've gotten a flu vaccine may have symptoms that are less severe and diminish faster (via the Harvard Medical School). Flu symptoms tend to hit hard and fast. Common complaints include a fever and chills, aching muscles, headache, a dry cough, extreme tiredness, a runny or stuffy nose, and a sore throat. Some people may also experience shortness of breath and eye pain, and children may have vomiting and diarrhea (via the Mayo Clinic). The Harvard Medical School notes that even after other symptoms have resolved, people often feel tired and drained for an extended period of time after battling the flu.
While most flu symptoms are what you'd expect from a respiratory illness, the full-body aches that usually accompany influenza can take people by surprise. According to Loma Linda University Health, body aches, like other symptoms of the flu, are actually the result of your body's attack on the virus and not the virus itself. Once the antibodies produced by our immune system "tag" the virus by binding to it, our immune system produces proteins that kill the virus. However, these proteins also cause painful joint and muscle inflammation.
Differentiating the flu from other conditions
No one enjoys playing the "Was that sneeze just allergies or am I coming down with the flu?" game. With the emergence of COVID-19, being able to differentiate one respiratory illness from another has become even more important. How can you tell the difference between influenza, the common cold, allergies, and COVID-19?
Some symptoms are the same across these 4 conditions. For example, all 4 often come with fatigue and a cough. Fever is common in cases of both influenza and COVID-19, but rare during a cold and not a part of allergies. Body aches are very common and can be severe with the flu, whereas they tend to be more mild with a cold, and may or may not show up with a COVID-19 infection. A stuffy or runny nose and sneezing are common with both a cold and allergies, but less likely to occur with the flu or COVID-19. A sore throat is common during a cold or the flu, but rare otherwise. Shortness of breath may be a sign of serious COVID-19 infection or the result of allergies. Allergies begin immediately after exposure to an allergen, whereas a cold and the flu have an incubation period of several days. COVID-19 can have an incubation period of up to 2 weeks (via Our Lady of the Lake). When in doubt, it's always a good idea to contact your doctor, who'll be able to provide additional guidance.
Spreading the flu
According to the CDC, influenza has an incubation period of 1-4 days, which means people may unknowingly spread the disease before they even have symptoms. The CDC specifies that people who have the flu are most contagious within the first 3-4 days after the illness sets in. Children and those with weakened immune systems may be contagious for even longer. When someone with the flu coughs, sneezes, or talks, they produce tiny water droplets that contain the virus. If these droplets are inhaled by someone else, that person can become infected. However, according to the Center for Infectious Disease Research and Policy, the influenza virus can also travel in aerosols, meaning that a sick person can spread the flu simply by breathing. The flu can also be picked up from contaminated surfaces and objects. It lives the longest (up to 48 hours) on hard surfaces like steel and plastic, but only about 8-12 hours on fabric (via Insider).
R0 (pronounced "R naught") indicates how easily an infectious disease spreads by estimating how many people one sick person will infect. For influenza, the R0 is between 2-3, meaning on average, 1 person with the flu will give it to 2-3 other people. For comparison, COVID-19's R0 has been estimated at between 1.5-3.5, while measles, a highly contagious disease, has an R0 of 12-18 (via Michigan Medicine).
Complications of influenza
For most people, the flu is a miserable but short-lived experience that doesn't have any long-term effects. For some, however — especially the very young, very old, and those with compromised immune systems or serious chronic health issues — getting over influenza can become a life-or-death battle. Complications of the flu include pneumonia, bronchitis, ear infections, asthma attacks, heart problems, and acute respiratory distress syndrome (via the Mayo Clinic).
Pneumonia is the most common (and one of the most dangerous) complications of influenza. Influenza usually infects the upper respiratory tract, but if it travels to the lungs, it can cause viral pneumonia. According to the American Lung Association, the air sacs [alveoli] of the lungs can fill with pus and other liquid. This blocks oxygen from reaching the bloodstream. Lack of proper oxygenation can cause organ damage and even death.
Influenza is one of the most common causes of viral pneumonia. As a 2010 paper published in Critical Care explained, influenza can also cause a secondary bacterial infection in the lungs known as bacterial pneumonia. In some cases, bacterial pneumonia co-occurs with viral pneumonia — a double whammy you definitely don't want. In other cases, bacterial pneumonia may occur after the influenza infection, without viral pneumonia ever being present. Battling the influenza virus, especially if it's made it to the lungs, can substantially weaken the immune system and the structural integrity of the lungs. This makes them more susceptible to opportunistic bacterial lung infections.
When to see a doctor and how flu is diagnosed
According to the Mayo Clinic, most people who get influenza don't need to see a doctor, since the immune system will clear the infection in about a week. However, anyone at higher risk of complications should see a doctor, who may decide that antiviral medications are a good option. You should also seek immediate care if you have emergency symptoms, such as difficulty breathing, chest pain, ongoing dizziness, seizures, or worsening of preexisting medical conditions.
If your doctor decides to test you for influenza, there are several options. Rapid influenza diagnostic tests (RIDTs) look for influenza antigens (the H and N proteins on the surface of the virus) and can provide results in just 10–15 minutes. These tests are quick and easy to perform, but not the most accurate, leading to the possibility of false negatives. RIDTs are better at detecting influenza in children compared to adults. Another test, known as a rapid molecular assay, looks for genetic material from the virus. It takes about 15–20 minutes, and is more accurate than an RIDT. The most accurate tests, such as viral cultures and reverse transcription polymerase chain reaction (RT-PCR) tests, can only be performed in special lab settings and may take several days to get results (via the CDC).
Treating the flu at home
For most people, treating the flu is simply a matter of giving your immune system time to work its magic. There are a few things you can do to make yourself more comfortable. First, get plenty of fluids, as the fever that usually comes with the flu can lead to dehydration. Second, get plenty of rest; this ensures your body can devote more resources to battling the virus. Third, you can take over-the-counter pain relievers like acetaminophen (Tylenol) and ibuprofen (Advil) to soothe achy muscles and bring down a high fever (via the Mayo Clinic).
It's equally important to know what not to do when you have the flu. Most importantly, don't take antibiotics (unless you have a diagnosed case of bacterial pneumonia). Antibiotics don't work against viruses, and overuse of antibiotics can wreak havoc on your friendly bacteria while encouraging the creation of drug-resistant "superbugs." It's also not a good idea to self-medicate with alcohol, since it contributes to dehydration and may rob you of the sleep your immune system needs. Nasal sprays are also not a good idea. They dry out the nose and throat, which can actually increase inflammation and irritation. Furthermore, the more you use them, the less likely they are to work (via Today).
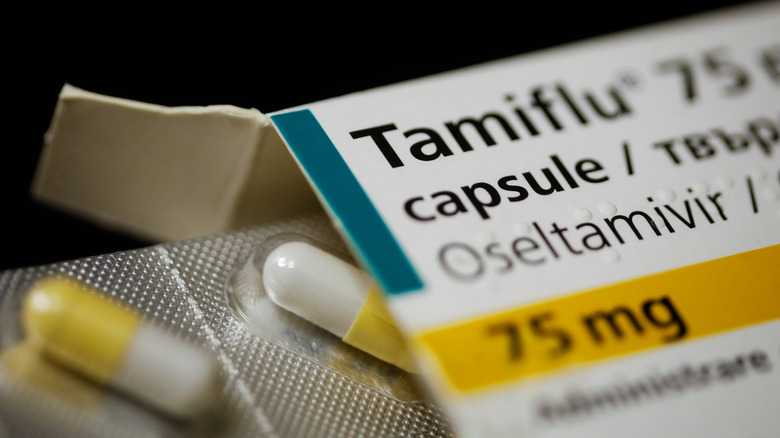
The use of antiviral drugs for the flu
While rest, fluids, and some OTC pain relievers are all that most people need to make it through the flu, those at risk of complications from influenza may be given antiviral drugs. As the Food and Drug Administration (FDA) explains, antiviral drugs available via prescription can reduce how long it takes for symptoms to improve. Antiviral drugs are most effective when treatment begins in the first 48 hours after symptoms appear. There are currently 4 FDA-approved antiviral medications for influenza: Rapivab (peramivir), Relenza (zanamivir), Tamiflu (oseltamivir phosphate), and Xofluza (baloxavir marboxil). Two older medications, amantadine and rimantadine, are no longer used today because influenza viruses have become resistant to them.
Antivirals come in several forms. Tamiflu and Xofluza are tablets taken by mouth, while Rapivab is injected and Relenza is inhaled. All are approved to treat influenza, but only Relenza and Tamiflu are approved to prevent the flu. The FDA points out, however, that these preventative antivirals are no substitute for getting a yearly flu shot. Tamiflu can be given to babies as young as just 2 weeks old, but the minimum age for the others varies from 2-12 years.
What you can do to prevent the flu
If you've had the flu before, you'll bend over backward to dodge getting it again. Luckily, protecting yourself from the flu isn't rocket science. The Mayo Clinic recommends common-sense strategies, such as avoiding crowded places, steering clear of people who are sick, washing your hands with soap and water for at least 20 seconds throughout the day, avoiding touching your face, and regularly cleaning high-touch surfaces. The Mayo Clinic noted, however, that the CDC doesn't recommend the general public wear masks to protect against the flu. However, healthcare workers caring for sick patients and for people with influenza may want to wear them. The Mayo Clinic pointed out that the mask you're wearing because of COVID-19 may also offer some protection against the flu.
When it comes to disinfecting surfaces, you've got plenty of options. A number of common household cleaning products can kill the influenza virus, including chlorinated bleach, hydrogen peroxide, rubbing alcohol, iodine, and detergents. The virus is also killed at temperatures above 167 degrees Fahrenheit (via the CDC).
What you should know about the flu vaccine
The best way to minimize your chances of coming down with the flu or its complications is by getting a yearly influenza vaccine. Flu shots have been in use in the United States since 1945 and are extremely safe (And no, you can't get the flu from a flu shot). There are several vaccine options. Some contain inactivated (killed) viruses, while others contain live attenuated (weakened) viruses. A third type, known as recombinant influenza vaccine (RIV), contains only pieces of genetic material from the virus. The live attenuated vaccine is given as a nasal spray, while the others are given as injections.
Each year, scientists create a new vaccine formulation based on which strains of influenza the World Health Organization (WHO), FDA, and CDC think are most likely to circulate during that flu season. Since influenza strains change often, it's important to get a flu shot every year. Children getting immunized for the first time should get 2 doses, spaced 4 weeks apart. For most, the ideal time to get vaccinated is September or October, before flu season sets in. Certain high-risk groups may need to be vaccinated earlier in the year.
The flu shot is not always 100% effective, as scientists can't always accurately predict which virus strains will emerge during flu season. However, the vaccine is about 40–60% effective in preventing influenza infection. It also excels in preventing complications, like pneumonia (via the Immunization Action Coalition).
The timing of flu season
The annual flu season coincides with winter. In the United States and elsewhere in the northern hemisphere, this means that it usually swings into action in December, reaches its peak in February, and dies down at the end of March. No one knows for sure why the flu is so prevalent in the winter, but there are a few factors that may play a role.
When it's cold outside, people tend to spend more time indoors with the windows closed. Close physical proximity to other people without adequate ventilation is a recipe for spreading the virus from one person to another. Research conducted in the 2000s using guinea pigs found that the influenza virus prefers cool, dry conditions. These conditions appear to allow it to live longer on surfaces and transmit more easily. Interestingly, in areas like the tropics where it never gets truly cold, influenza appears to prefer warm, high-humidity conditions. In addition, during the winter months, people tend to get less sun exposure, causing a drop in vitamin D levels. Vitamin D is critical for immune function, so lower levels might make us more susceptible to viral infections, such as influenza (via Harvard University).
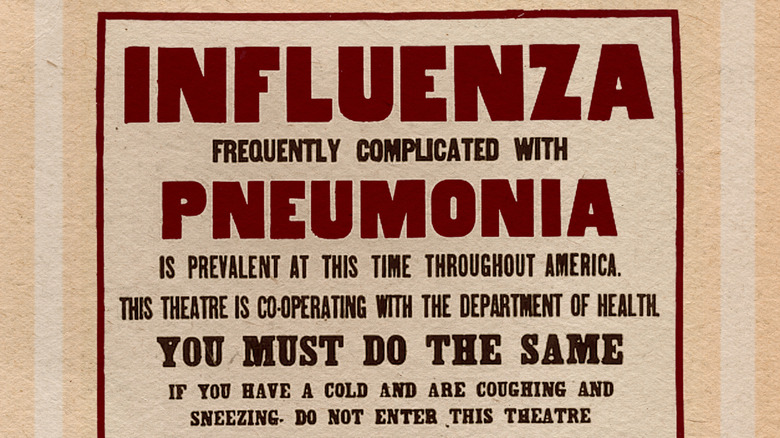
Understanding flu pandemics
Seasonal influenza is annoying and sometimes dangerous, but quite predictable. Every so often, however, new strains of influenza can cause devastating worldwide pandemics. This occurs because of antigenic shift. Unlike antigenic drift, where small changes to the proteins on the surface of the influenza type A virus accumulate over time, antigenic shift happens suddenly and produces totally new viral surface proteins. This can create a new influenza A subtype. Shift often occurs when an influenza virus "jumps" from its native animal population to humans. Since our immune systems have no prior experience with this new influenza virus, they tend to infect more people and cause more serious illness compared to the regular, seasonal flu. Often, after an initial pandemic, the new virus becomes one of the circulating strains that cause a seasonal flu (via the CDC).
Fortunately, flu pandemics don't happen often; there have been just 4 since the early 1900s. The 1918 flu pandemic (erroneously called the "Spanish Flu") saw the emergence of the H1N1 virus. Proportionately, it was the most severe pandemic in recent history. One-third of the world's population became ill, and about 50 million worldwide (including about 675,000 people in the United States) died. This pandemic was unique in that many who died were otherwise healthy people in their 20s, 30s, and 40s. The next flu pandemic was the 1957 H2N2 "Asian Flu," followed in 1968 by the novel H3N2 virus. The most recent influenza pandemic erupted in 2009 with the emergence of a new subtype of H1N1 (via the CDC).