Mistakes You Could Be Making If You Have Diabetes
Diabetes is a chronic condition relating to high blood sugar. Because it affects the body's use of or ability to make insulin, the metabolic process that relies on insulin becomes impaired. According to the CDC, about 10.5% of the United States population has diabetes, and another 34.5% of adults have prediabetes, a potential predictor of diabetes development. Moreover, the trend of diabetes diagnosis doesn't seem to be slowing down, rising from only a 4% prevalence of the condition back in 2000.
People with diabetes should visit their doctor regularly to manage the condition. Diabetes can affect several parts of the body, making it difficult to keep under control. Plus, a plethora of information on diabetes management can overwhelm patients, leading to mistakes while trying to control their diabetes. If you believe you might be mismanaging your condition, know that you're not alone. Continue reading to learn about common mistakes people with diabetes make and what to do about them.
You're not visiting the doctor enough
Before doing anything to manage your diabetes, you should seek the help of your doctor. Your primary care physician (PCP) is who will become your hub for information about your condition. The CDC recommends visiting your PCP once every six months to monitor your diabetes and make tweaks to your care plan, if necessary. However, if you're having trouble keeping your blood sugar under control, visiting every three months is a better plan. Your PCP's routine exams and blood tests are the best ways to keep a close eye on any potential problems.
Your PCP might recommend seeing other doctors, too, if you're having trouble eating healthy or working out or you're experiencing diabetes-related symptoms. For instance, an opthalmologist can check out any vision problems caused by diabetes, while a podiatrist can monitor your foot health, as nerve damage can be a problem for people with diabetes. Some doctors might also suggest adding an endocrinologist to your care team, as they're specifically equipped to handle diabetic challenges (via WebMD).
You're not using your medications properly
Diabetes management often consists of drugs that can help control blood sugar. Usually, they're in the form of pills or injections, depending on the severity and type of diabetes. Understanding exactly how to use your medication and getting into a routine of using it at the right times is crucial to successful diabetes management.
Oral medications are only for people with type 2 diabetes. If you're a forgetful medicine taker, you could have trouble remembering to take your pills. For people who manage their diabetes well through diet and exercise, forgetting a dose here and there might not matter much. But chronic forgetfulness and otherwise not-so-great diabetes management can become a problem. According to Healthline, you can take the dose as soon as possible after missing it, but don't take doses close together. Instead, call your doctor to figure out the best route, whether that's making up your dose or skipping to the next one.
Insulin injections can be even more challenging to juggle, especially if you're on a few different kinds. You'll need to understand the differences between rapid-acting, long-acting, and other types of insulin and when they're necessary to use. The American Diabetes Association notes that premixed supplies are available to make the medication process more manageable, so it's worth discussing with your doctor if you're having trouble juggling your insulin routine.
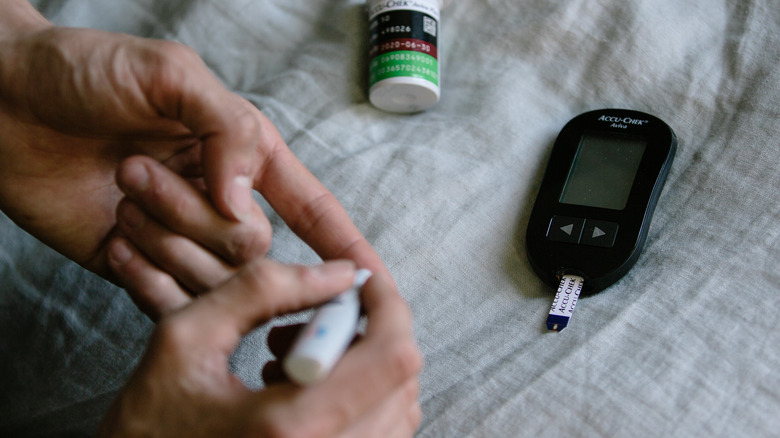
You're not checking your blood sugar enough
Blood sugar is the primary concern for people with diabetes. Still, that doesn't mean that everyone with diabetes checks it regularly as they should, and that mistake could be detrimental to a diabetes management plan.
To understand your specific goals for checking your blood sugar, check with your doctor. But the general guidelines suggest checking it several times each day, especially before meals and at bedtime. Some people may need to check more often, like after meals and before and after exercise. These blood sugar checks can help you plan your meals and show you how well you're staying within healthy blood sugar ranges. That means blood sugar levels between 80 and 130 milligrams per deciliter (mg/dL) before meals and less than 180 mg/dL two hours after a meal (via Mayo Clinic).
The CDC also recommends getting an A1C test twice a year, or possibly more often if your doctor thinks it's a good idea. This test measures your blood sugar levels over three months and gives an average count, which can provide a more accurate picture of how well you're controlling your diabetes.
You're not exercising regularly
Exercise is one way to make your blood sugar levels drop. Plus, it can improve insulin sensitivity, reduce cardiovascular risk factors, and increase muscle strength, all of which are important for people with diabetes (via the American Diabetes Association). If you're not getting enough physical activity, you could be making your diabetes worse.
It appears that exercise makes a rather significant difference in diabetes management, too. According to Harvard Health Publishing, studies have shown that exercise has the power to lower A1C values by 0.7% combined with various diets and medications. Other studies showed improvements in insulin resistance and heart health when people with diabetes added physical activity to their routines. Exercising after eating may be even more beneficial than fitting it in at other times of the day, as this period is when your blood sugar is highest and could use some help coming down.
A scientific review article published in the Cleveland Clinic Journal of Medicine found that practically any form of exercise — resistance training or cardio, for instance — can be equally as effective in managing diabetes. The authors note that all exercise reduces glucose levels and, when consistent, can lead to improved cardiovascular health.
You succumb to cravings a little too often
Having diabetes doesn't mean you need to stop eating everything you enjoy. But, there definitely are some foods that people with diabetes need to be more careful with, including processed ingredients and foods with refined carbs. Still, experts agree that when you manage diabetes well, you'll have a little more wiggle room to eat foods you love. Dietician Leanne Katzenellenbogen tells News 24, "Make sure your food tastes good; otherwise, it becomes difficult to sustain. Eating and food are such a big part of day-to-day life."
Problems happen when you're not careful about the "cheat" choices you make. For instance, eating a large slice of cake when you should have limited it to a few bites could throw blood sugar out of whack. Registered dietician Cynthia Sass tells Eat This, Not That!, "What matters most to your overall health is what you do repeatedly, especially over time. One analogy I use with my clients is this: if you're on a financial budget and on occasion you go on a little shopping spree, you aren't going to rack up a huge debt. But if you have no budget and splurge more frequently, you can easily max out your credit card."
Registered dietician Lori Zanini explains to EndocrineWeb that everyone's body functions differently, so it's crucial to understand yours and what affects your blood sugar most. Then, work to find "reasonable substitutes" to the foods you should avoid so that you don't feel deprived.
You're yo-yo dieting
A healthy diet is a priority for people with diabetes. But some diets are difficult to sustain, especially if you feel like you can't eat any of the foods you enjoy. With a difficult-to-follow diet often comes yo-yo dieting, which refers to the on-and-off cycle of dieting.
The problem with yo-yo dieting for people with diabetes is that it usually causes weight fluctuations (via Healthline). Research concludes that ups and downs in body weight could be a risk factor for diabetes. For example, one 2019 study published in the Journal of Clinical Medicine found that, even in participants under 65 years old and with normal glucose tolerance, body weight fluctuations increased the risk of developing diabetes. Another 2018 study in Diabetes Research and Clinical Practice found that the participant group with the highest average successive variability of weight (ASVW) had the highest risk of diabetes.
A 2018 study played out over 16 years and determined how body weight fluctuations over a longer period affected diabetes risk and mortality. The results indicated that initial body mass index (BMI) played a role in how much a person's weight fluctuation impacted their diabetes risk. To sum up: Higher BMI combined with ups and downs in body weight could contribute more to diabetes than weight fluctuations alone.
Your drinks sneak in a lot of sugar or carbs
If you live with diabetes, you likely already know some of the primary sources of carbohydrates that you should try to avoid or limit. For instance, refined pasta, cake, and ice cream are not the best choices for people watching their blood sugar, as these high glycemic foods can spike blood sugar quickly.
But what about the drinks you have each day? They're important to monitor, too. However, it can be easier to forget about tracking them simply because we don't always think of drinks the same way as foods. But according to the Harvard T.H. Chan School of Public Health, drinks with added sugars or artificial sweeteners "are the single largest source of calories and added sugar in the U.S. diet." Sugar, of course, leads to a higher carb count in drinks, and carbs turn into sugar in the body. The Harvard T.H. Chan School of Public Health also says that drinking one or two sugary drinks a day can increase diabetes risk by 26%. Increasing artificially-sweetened drinks by just 4 ounces a day leads to an 18% higher risk.
You don't drink enough water
Water is essential for every person to drink each day to prevent dehydration. But people with diabetes should take even more care to ensure they're getting enough water. Nutrition professor Dr. Stavros Kavouras tells Discover that dehydration can impair glucose metabolism, based on the results of a study he and his research team conducted in 2017. Kavouras explained that the study's participants were dehydrated for just three days before their glucose metabolism was affected. According to Kavouras, water certainly isn't the only thing that affects or increases the risk of diabetes, but it does play a role.
According to the Harvard T.H. Chan School of Public Health, some people have a difficult time switching to plain or sparkling water if they're used to drinking a lot of sugary drinks or sodas. If that's the case, try naturally-flavored sparkling water or water with healthy additives, like lemon or lime slices or fresh herbs.
Water isn't the only way to stay hydrated, either. Healthline lists several beverages that people with diabetes can drink to prevent dehydration without adding loads of sugar and calories. Tea, unsweetened coffee, and low-fat milk are good options.
You don't get good sleep
A lack of sleep could make it more challenging to control diabetes, according to the CDC. Without the recommended seven hours of sleep each night — at a minimum — your body may become more resistant to insulin, have a harder time losing weight, and make you feel hungrier the following day. You also might have more cravings for carbs and sugary foods without enough Zzz's the previous night.
Irregular sleep has become a common problem for people in the United States, many of which have busy and fast-paced lives. However, Eve Van Cauter, PhD, explains to the National Institute of Diabetes and Digestive and Kidney Diseases that interruptive sleep patterns are especially harmful to people with prediabetes and diabetes. "Studies show that many sleep problems are associated with insulin resistance, prediabetes, and diabetes and have a significant impact on glucose tolerance," Van Cauter says. "For example, there is experimental evidence that if you take healthy volunteers and force them into a schedule where sleep does not occur consistently during the night, the result is a decrease in glucose tolerance and insulin sensitivity."
Van Cauter admits that more research is necessary to determine whether improving sleep patterns can consequently improve diabetes management. However, some research has shown that extending sleeping time leads to improved insulin sensitivity.
You don't manage your stress
Feeling stressed? If so, your stress could be part of why your diabetes has been difficult to manage lately. The American Diabetes Association explains that when you feel stressed, your body produces stress hormones in response. Among other changes to the body, these stress hormones make blood glucose rise. Therefore, chronic stress can continually affect your blood sugar levels, regardless of the other things you do to manage them.
A review article in the Journal of Neurology and Psychology further examines the relationship between stress and diabetes. Evidence shows that the longer stress occurs, the more challenging it becomes for the body to adapt to changes. Over time, stress can affect the immune and endocrine systems, both of which play a role in diabetes. Furthermore, women seem to be more impacted by the effects of stress and a higher risk of diabetes than men. Stress can also exacerbate complications in the elderly, like retinopathy and neuropathy.
If you're having a hard time dealing with stress, try relaxing techniques like yoga, meditation, and aromatherapy.
You love eating salty foods
Salt intake is often associated with high blood pressure, but evidence suggests that it could also increase the risk of type 2 diabetes and make diabetes more difficult to manage. According to Medical News Today, salt can contribute to insulin resistance and weight gain. Furthermore, it can be especially harmful to people with a specific form of diabetes known as latent autoimmune diabetes in adults (LADA). This autoimmune version of diabetes may be affected by salt intake because excess salt can "accelerate autoimmunity and play a role in the [disease development] of LADA," researcher Dr. Bahareh Rasouli tells Medical News Today.
One of Rasouli's studies found that consuming just one extra gram of sodium each day led to a 43% increased risk of type 2 diabetes and a 73% increased risk of LADA development. Plus, the effect continued with each extra gram of sodium.
Unfortunately, sodium is in a lot more food items than many people realize. Diabetes UK lists breakfast cereals, ketchup, pickles, and cheese as sneaky items that contain a high amount of salt. Of course, processed foods, bacon, canned foods, and salty snacks also top the list. To reduce your daily salt intake, Diabetes UK suggests measuring the salt you add to food instead of sprinkling it and cooking from scratch as much as possible rather than relying on processed foods.
You don't take care of bumps and scrapes
Diabetes can cause delayed wound healing, as high blood glucose interferes with the healing process. Unfortunately, a small scrape or bump can quickly translate into a worsened condition. For some people with diabetes, what started as a wound — especially on the foot — can lead to amputation if not treated quickly and adequately (via Healthline).
A 2020 study published in Nature Communications examined inflammation in response to diabetic foot ulcers, which commonly occur in people with diabetes when a foot wound worsens rapidly or isn't taken care of properly. Researchers compared samples from the ulcers to samples from normal-healing wounds to note differences in the healing process. Ultimately, they found that inflammation, tissue-repair genes, and immune cell activity were less efficient in diabetic wounds than in healthy wounds (via National Institute of Health).
Per Healthline, it's vital to keep tabs on your body and immediately treat wounds. Additionally, care for your wounds each day and see your doctor if it doesn't seem to be healing.
You refuse to cut your smoking habit
Smoking is unhealthy for several reasons; this isn't breaking news. However, people with diabetes may not know just how bad it can be for their diabetes management. According to a report from the U.S. Department of Health and Human Services, smoking can even cause type 2 diabetes, with smokers increasing their risk for developing the condition by as much as 40%. The report also notes that smoking is linked to an increased risk of obesity, higher levels of cortisol which can create more visceral fat, and affect hormones. Together, the heightened chances of obesity from smoking may contribute to its connection with diabetes.
The U.S. Food & Drug Administration adds that nicotine can decrease the efficacy of insulin. When insulin doesn't work as well as it should, the body needs more of it to control blood glucose. Regular smoking can, therefore, cause the body to ramp up insulin production to accommodate. The FDA suggests quitting smoking as soon as possible, but doing so with the support of your doctor, help lines, and other resources that can help you kick the habit long-term.
You're ignoring other symptoms
Sometimes, these other conditions that stem from diabetes are caught before a diabetes diagnosis. Diabetes sometimes throws out early warning signs that signal there's a problem with your body that you should get checked out, like blurry vision, slow-healing wounds, numbness or tingling in the body, frequent urination, and excess thirst (via Medical News Today).
It's important not to ignore these symptoms, as high blood sugar affects more than insulin and the body's response to insulin. High glucose can also damage the nervous system, vision, and digestion. It even has links to cardiovascular health, affecting blood vessels, blood pressure, and stress on the heart (per Medical News Today). Kidney disease is another concern for people with diabetes, as diabetes causes narrowing blood vessels, affecting how much blood the kidneys get. Over time, the kidneys become less efficient at filtering out waste (via the National Kidney Foundation).
If you spot early warning signs, it's a good idea to visit your doctor. According to the American Diabetes Association, early intervention can slow diabetes progression or delay its development.