Macular Degeneration Explained: Causes, Symptoms, And Treatments
According to the Centers for Disease Control and Prevention (CDC), vision impairment is the ninth leading cause of disability among American adults. There are many conditions that can cause vision loss or even blindness, and age-related macular degeneration (AMD) is one of the most common. As the BrightFocus Foundation noted, roughly 11 million Americans live with some form of AMD — a statistic projected to balloon to 22 million by 2050. The estimated number of people living with AMD globally is 196 million, and that number is expected to rise to 288 million by 2040. AMD is a leading cause of vision loss for Americans over 60, and around the world AMD is one of the primary causes of uncorrectable blindness.
But what exactly is AMD? As the BrightFocus Foundation explained, it's "an irreversible destruction of the macula [part of the eye], which leads to loss of the sharp, fine-detail, 'straight ahead' vision required for activities like reading, driving, recognizing faces, and seeing the world in color." The global cost associated with AMD is estimated to exceed $340 billion. Although AMD can't be cured, treatments to prevent or delay the condition from advancing are available, and there are steps individuals can take to minimize their risk of getting AMD. There's still a lot we don't know about the condition, and today's AMD research focuses on better understanding causes and risk factors, as well as pioneering new treatments and potential cures.
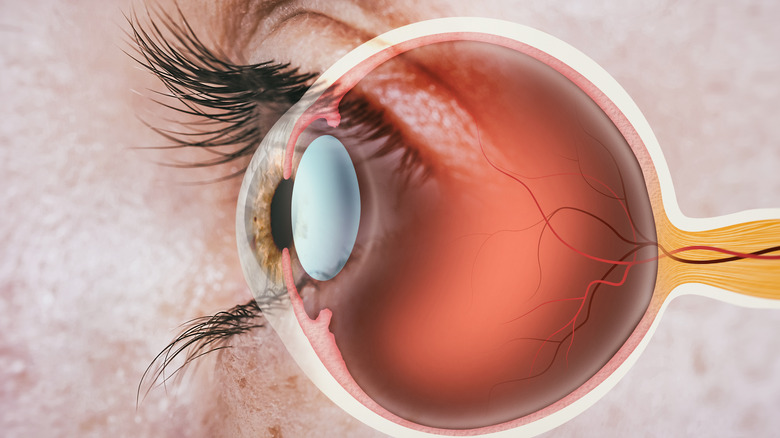
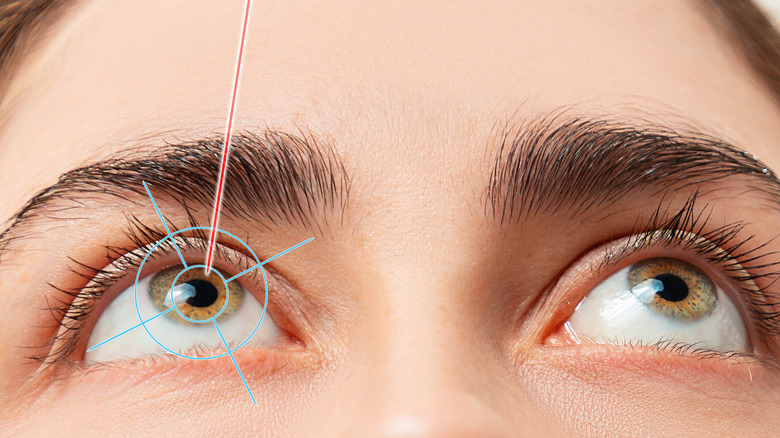
Eye anatomy
To better understand AMD, it's important to know a bit about the anatomy of the eye and how it allows us to see.
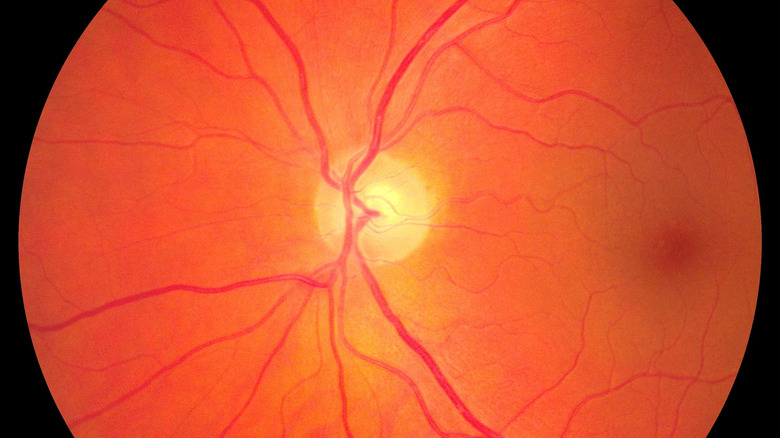
As the American Academy of Ophthalmology explains, at the front of the eye is a clear dome-shaped structure called the cornea, and behind the cornea is a small space filled with aqueous humor, which helps maintain proper pressure inside the eye. Behind this liquid-filled space is the iris (the colored part of the eye), which surrounds the pupil. Behind the pupil is the lens, and behind the lens is a space filled with a jellylike substance called vitreous humor. At the very back of the eye is the retina. The tiny central portion of the retina is called the macula, and the rest of the retina is known as the peripheral retina. The optic nerve connects the back of the eye to the visual center in the brain.
Light is focused through the cornea and lens onto the retina. The retina is the light-sensitive part of the eye, and special cells there called photoreceptors change light into energy that's transmitted to the brain via the optic nerve. There are two types of photoreceptor cells found in the retina: rods and cones. Rods allow us to see in low-light conditions, while cones allow us to perceive color. Cones are also responsible for central, high-detail vision.
Dry AMD
There are two types of AMD: dry and wet. According to the American Macular Degeneration Foundation, the dry form is much more common, accounting for about 90% of cases.
In dry AMD, the layers that make up the retina's macula gradually thin (atrophy), which decreases their ability to function properly. Dry AMD is also known as non-neovascular AMD or non-exudative AMD, because there's no leakage of fluid from blood vessels behind the retina as there is with wet AMD. In the early stage of dry AMD, the pigment of the macula changes. For some individuals, this is as far as their dry AMD gets, and they may not experience any vision changes.
In other cases, however, dry AMD gets worse over time. As the National Eye Institute explains, there are three stages of AMD: early, intermediate, and late. Usually, dry AMD progresses slowly over the course of several years. It's possible to have dry AMD in either both eyes or only one eye. The BrightFocus Foundation notes that late-stage dry AMD can cause significant vision loss. In addition, some cases of early-stage dry AMD may turn into wet AMD, which is the less common but more serious form of the disease.
Drusen and dry AMD
But what exactly triggers the deterioration of the macula in dry AMD? According to VisionAware, the answer is drusen.
Drusen are small white or yellow deposits that form beneath the macula, damaging it. These deposits are made up of waste products such as proteins, fats, and cholesterol. As dry AMD progresses, the number and size of individual drusen deposits increases. While drusen don't necessarily cause vision loss, they are a risk factor for AMD progressing to vision loss.
Drusen are quite common. According to the American Macular Degeneration Foundation, almost everyone over 50 has at least one drusen. Perhaps because they're so common, not everyone agrees that drusen directly cause macular degeneration. Per the American Academy of Ophthalmology (AAO), while drusen is unlikely to cause AMD, "having drusen increases a person's risk of developing AMD, and they may be a sign of AMD." The AAO notes that drusen are a natural part of aging, and that a few small drusen don't indicate a problem. Small drusen don't cause any symptoms but can be seen during an eye exam. Drusen themselves don't require treatment, but an ophthalmologist will want to keep an eye on their size and number as a way of monitoring for AMD.
Wet AMD
According to the BrightFocus Foundation, wet AMD is far less common than dry AMD, but also more serious. It accounts for only about 10% of AMD cases but is responsible for 90% of AMD-related blindness. Unlike dry AMD, wet AMD isn't divided into stages, and is simply considered an advanced form of the condition. All cases of wet AMD begin as dry AMD, but most cases of dry AMD don't turn into wet AMD.
Per VisionAware, wet AMD is also known as neovascular because of the development of abnormal blood vessels. As VisionAware explains, "in this form, the degeneration of the macula causes the retina to create a protein called VEGF. This is made by the retina in order to protect itself and to create new blood vessels." These new blood vessels, however, are abnormal and weak. They break easily, leaking blood and other fluid that further damages the macula. Over time, this damage causes the formation of scar tissue, which can cover the macula and cause extreme loss of central vision. In addition to being likely to cause more severe vision loss, wet AMD also progresses more rapidly than dry AMD. Wet AMD is also known as exudative AMD because it involves exudation (leakage) of the newly formed blood vessels (via the American Macular Degeneration Foundation).
Vision changes with AMD
AMD can cause significant changes to vision and vision loss, but the severity of symptoms depends on the type and severity of AMD. As the National Eye Institute (NEI) states, "AMD is a progressive disease — that means symptoms usually get worse over time." There aren't any vision changes in early dry AMD. With moderate dry AMD, some people will still have no vision changes, while others will have minor symptoms. In late dry AMD and wet AMD, vision changes become obvious and can significantly impact daily life.
According to Johns Hopkins Medicine, vision changes that occur with AMD include blurry or fuzzy vision and the appearance of a dark, empty area (blind spot) in the center of an individual's vision. Straight lines will also begin to look wavy. This loss of central, detailed vision makes tasks such as reading, driving, and recognizing faces very difficult. The NEI noted that difficulty seeing in low light and colors appearing less bright are also common symptoms of AMD. Although advanced AMD can cause significant visual impairment and disability, the NEI pointed out that it doesn't lead to total blindness because peripheral vision isn't affected.
Johns Hopkins Medicine cautions that the symptoms of AMD, especially the more mild ones like blurry vision or difficulty seeing in low light, overlap with a number of other eye conditions, so any vision changes should be evaluated by an ophthalmologist.
Risk factors for AMD
As the name implies, the main risk factor for AMD is age. According to WebMD, about 2% of people in their 50s have AMD, but by 75, that percentage jumps to almost 33%. But age isn't the only risk factor.
Genetics plays at least some role, and more than 20 genes have been linked to AMD. Caucasians have the highest risk for AMD, at least in part because about a third have a gene linked to AMD. Black people have the lowest risk of developing AMD. Women are twice as likely as men to have AMD, but this may simply be because women tend to live longer than men. Having surgery to correct cataracts ups your chances of getting AMD. Unsurprisingly, having AMD in one eye means you're much more likely to get it in the other eye.
Although these risk factors are ones we have no say over, there are others that are more under our control. Smoking quadruples your risk of AMD, most likely because it reduces the amount of oxygen that reaches your eyes. High blood pressure and heart disease also increase your risk. Having a BMI over 30 may more than double your odds of getting AMD. An unhealthy diet and drinking lots of alcohol isn't a good idea in general, and these habits increase your risk for AMD. Individuals who spend a lot of time outside in the sun without adequate eye protection also up their risk.
Diagnosing AMD
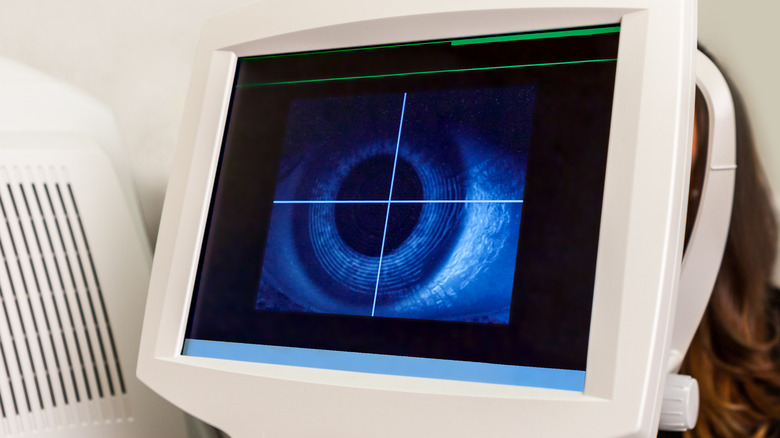
As the Cleveland Clinic explains, getting an annual eye exam is important, since early AMD doesn't cause any vision changes that you'd notice on your own. And because AMD treatments work best when the disease is caught early, having an ophthalmologist examine your eyes annually to spot the first signs of trouble is key to preventing AMD from progressing. During a standard eye exam, drops are used to dilate the pupil and the doctor uses a special lens to look at your retina, including the macula.
If the ophthalmologist needs to get a more detailed view of the back of your eye, they may use a technique called optical coherence tomography (OCT). This is a painless, noninvasive procedure in which a specialized machine takes detailed images of the retina and macula. If the doctor suspects wet AMD may be present, there are two techniques that can be used to check for blood vessel leakage under the macula. In fluorescein angiography, a yellow dye (fluorescein) is injected into an arm vein. It travels through your bloodstream and eventually reaches the blood vessels in your eye. A special camera tracks the dye and takes images that can reveal leakage under the macula. An alternative option is optical coherence tomography angiography (OCTA). Rather than injecting fluorescein dye, OCTA uses lasers, combined with the OCT camera, to produce three-dimensional images of blood flow in the eye, allowing doctors to identify any leakage from abnormal blood vessels.
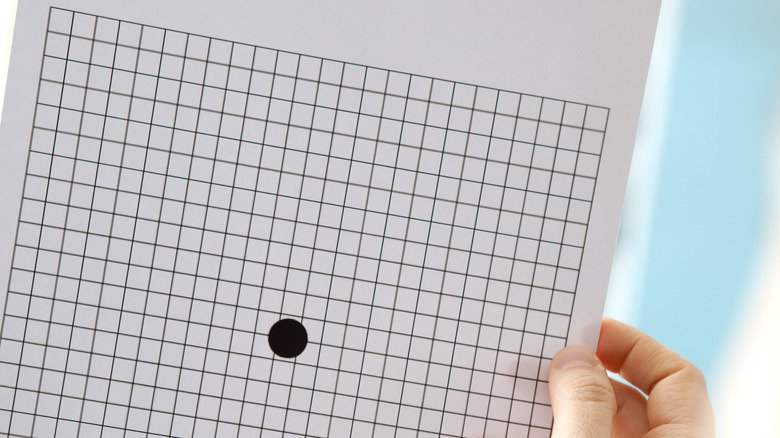
Monitoring your AMD at home
The techniques used to diagnose AMD require specialized equipment, but there's one simple test that ophthalmologists may use that you can also perform at home to check your vision.
As the American Academy of Ophthalmology (AAO) explains, an Amsler grid is made up of 324 white squares arranged in an 18 x 18 square, separated by black lines with a dot at the very center of the grid. To test your vision, you hold the Amsler grid 12–18 inches from your face and cover one eye. Staring directly at the center dot, take note if any of the black lines appear wavy or blurry, if any of the white squares look dark, or if any area on the grid appears blank. Repeat with the other eye. Because AMD usually progresses slowly, vision changes can happen so gradually that they're hard to notice in daily life. But the Amsler grid makes the vision changes characteristic of AMD very obvious. If you have AMD or are at high risk of developing it, the AAO recommends using an Amsler grid daily.
The ForeseeHome monitor is a more high-tech option for tracking the progression of AMD at home. According to the BrightFocus Foundation, the ForeseeHome monitor is the first device approved by the Food and Drug Administration (FDA) for monitoring dry AMD at home. The device scans each eye and can detect vision changes before they become apparent to the individual.
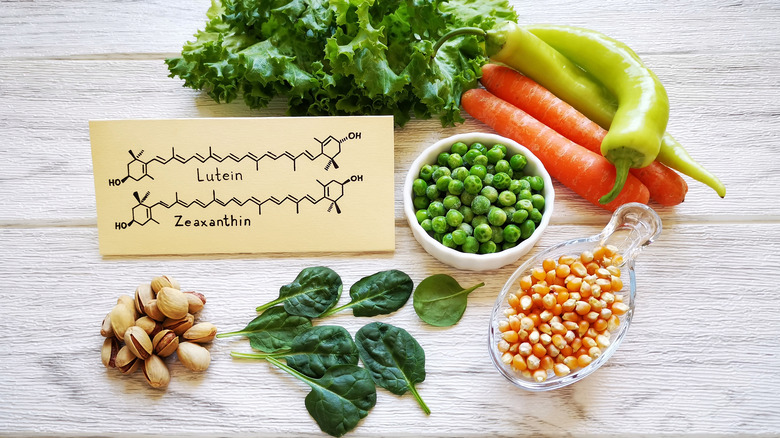
Nutritional supplements for AMD
As the Cleveland Clinic points out, there's currently no cure for AMD. But there are steps individuals can take to slow the progression of the disease. Nutritional supplements are key, although only two specific formulations have been clinically shown to be effective in managing AMD.
The National Eye Institute (NEI) funded the studies that produced the AREDS and AREDS2 supplements. These formulations were shown to help those with intermediate or late AMD, but didn't provide any benefit for those with early AMD or reduce the risk of getting AMD in the first place. Although AREDS and AREDS2 contain micronutrients known to promote eye health that are easy to find in food or other supplements, they feature much higher levels of these micronutrients. The AREDS formulation contains 500 milligrams of vitamin C, 400 IU of vitamin E, 15 milligrams of beta-carotene, 2 milligrams of copper, and 80 milligrams of zinc. AREDS2 contains the same quantity of vitamin C, vitamin E, copper, and zinc, but it doesn't contain any beta-carotene and instead has 10 milligrams of lutein and 2 milligrams of zeaxanthin. Both supplements are now available over the counter.
Although generally considered safe, the high doses of micronutrients found in AREDS and AREDS2 may negatively interact with certain medications. They may also slightly increase the risk for lung cancer in those who currently smoke or quit smoking very recently.
Managing AMD with anti-VEGF injections
For those with wet AMD, there are a couple of treatments that can be useful in managing the disease. As the American Academy of Ophthalmology explains, vascular endothelial growth factor (VEGF) is a protein produced by cells throughout the body that triggers the formation of new blood vessels. While VEGF's ability to stimulate creation of new blood vessels can be very beneficial in many situations, if the cells of the eye produce too much VEGF, it can lead to the development of the abnormal, leaky blood vessels that are the hallmark of wet AMD. Anti-VEGF drugs block the production of the VEGF protein, slowing or stopping the damage caused by the abnormal blood vessels. Anti-VEGF treatment stabilizes vision for about 90% of individuals, and for roughly one-third, it can actually improve vision.
There are currently three FDA-approved anti-VEGF drugs: Avastin, Lucentis, and Eylea, although a number of others are likely to be approved in the coming years. Research suggests that these three drugs are equally effective at treating wet AMD. Anti-VEGF drugs are also used to treat a few other eye conditions, including macular edema, diabetic retinopathy, and retinal vein occlusion. Anti-VEGF drugs are given as injections directly into the sclera (white) of the eye. The doctor numbs the eye beforehand, and uses an extremely thin needle to inject the medication. Injections are typically given every 4 to 12 weeks, depending on how an individual responds (via the BrightFocus Foundation).
Managing wet AMD with photodynamic therapy (PDT)
Another treatment option for those with wet AMD is photodynamic therapy (PDT). As Johns Hopkins Medicine states, PDT involves injecting a special light-sensitive medication called Visudyne (via WebMD) into a vein in an individual's arm. The medication travels through the bloodstream and collects in the abnormal blood vessels beneath the macula. The ophthalmologist then numbs the eye with anesthetic eye drops, inserts a special contact lens, and then shines a laser into the eye. The laser activates the Visudyne and causes it to create blood clots in the abnormal blood vessels. These clots seal off the vessels and prevents them from leaking fluid that would further damage the macula.
PDT isn't used as often today as it was in the past, since anti-VEGF drugs are more effective. Unfortunately, the results of PDT are often short-lived, since it doesn't stop additional blood vessels from forming, and those sealed up with blood clots may reopen. PDT makes both your skin and eyes extra-sensitive to light for a few days, so it's important to remain out of direct sunlight immediately following the procedure. PDT carries certain risks, including temporary eye soreness or loss of visual sharpness, reactions to the Visudyne, and appearance of new blind spots in your vision. Individuals need close monitoring after PDT to check for complications and the reemergence of leaky blood vessels.
Restoring vision with an implantable miniature telescope (IMT)
According to the BrightFocus Foundation, some people with late-stage AMD in both eyes may benefit from an implantable miniature telescope (IMT). An IMT is a special kind of artificial lens that provides magnification: one model offers 2.2x magnification, and the other offers 2.7x magnification.
IMTs work because even in advanced AMD where central vision is severely impaired, peripheral vision is still intact. IMTs magnify objects in the central field of vision so that they're large enough to be seen in peripheral vision. IMTs are inserted in a surgery similar to cataract surgery; the individual's natural lens is removed and the IMT (which is about the size of a pea) is implanted in its place. Individuals with an IMT can experience as much as a doubling in their visual acuity.
IMTs aren't a viable option for everyone, though. Individuals with wet AMD and those who've already had their natural lens removed because of cataracts aren't eligible. Individuals need to have a visual acuity that falls within a certain range and need to try out an external version of an IMT to gauge how well it will work for them. The surgery, while generally considered safe, does carry some risks. Surgery often results in about a 25% reduction of the epithelial cells lining the inside of the cornea. These cells are needed to keep the cornea clear, so the procedure is risky for people with a lower number of these cells to begin with.
Vision rehabilitation
Although there are ways to slow the progression of AMD, many people with the condition will eventually experience vision loss, and in some cases the decrease in their central vision may be so severe that it makes daily tasks such as reading and driving difficult or impossible. Vision rehabilitation, however, can help teach those with advanced AMD how to live with low vision.
As the BrightFocus Foundation explains, "vision rehabilitation, also known as low-vision rehabilitation, is a process through which individuals can pursue their independence and a good quality of life." A number of components can be incorporated into vision rehabilitation. A formal low-vision evaluation is often the first step and involves thorough testing of your remaining vision and education on tools and strategies that can assist with daily living. These tools and strategies may include magnifiers, telescopes, lighting and contrast modification. Additionally, changes can be made to your home environment to make daily activities easier and safer.
There are also a variety of private organizations and government-funded programs that provide additional resources, such as education and access to assistive technology. These groups can provide orientation and mobility training, which gives individuals the skills they need to navigate the world, including safely crossing streets and using public transit. Losing vision can be extremely challenging emotionally, so it's also important to connect with support groups where you can meet and interact with others going through similar experiences.
Preventing AMD
Since AMD can't be cured and can only be managed, taking steps to prevent it from developing in the first place is extremely important. Minimizing your risk for AMD centers on addressing those risk factors that are under your control. While you can't change your race or genes and can't stop yourself from getting older, there are many things you can do (or avoid doing) to reduce your risk of AMD. As the BrightFocus Foundation explains, if you're a smoker, quitting is one of the best things you can do to preserve your vision, especially if you already have early signs of AMD. Getting high blood pressure under control is also important. When out in bright sunlight, be sure to wear sunglasses and a hat to protect the eyes from UV damage.
Although the AREDS and AREDS2 dietary supplements haven't been shown to prevent AMD, people should strive to get these same micronutrients through a healthy diet. IN particular, eating foods rich in lutein and zeaxanthin may be beneficial. Foods with high lutein and zeaxanthin content include orange and yellow bell peppers, kale, broccoli, spinach, corn, zucchini, squash, kiwi, grapes, and egg yolks. Individuals should also aim to eat fatty fish (rich in omega-3s) at least twice a week.
Getting annual eye exams is critical, especially as you age. While these yearly checkups won't prevent AMD, they significantly increase the likelihood that the condition will be caught at an early stage.