What Happens If You Are Given The Wrong Blood Type During A Blood Transfusion?
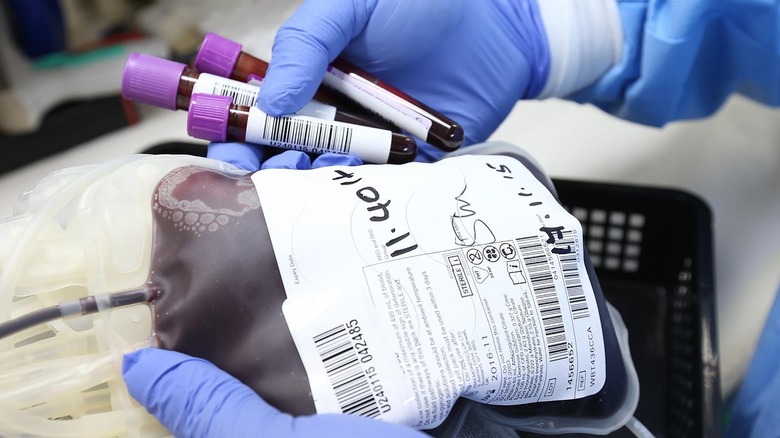
A blood transfusion is a process in which blood is taken from a donor and delivered intravenously to another person. There are a number of reasons why you might need a transfusion, such as having suffered major trauma, a surgery that resulted in a loss of blood, an illness that caused anemia, hemophilia, and certain cancers (via the Cleveland Clinic). The most common transfusions involve red blood cells, which carry oxygen and remove waste from the blood. Patients may also receive a whole blood transfusion, although this is less common (via the Mayo Clinic).
While everyone's blood is made up of the same components, it's important to note that blood is not the same. Antigens, surface markers found on red blood cells, exist in different forms in different people, which is what creates blood types. The body's immune system reacts to antigens, and if antigens that are different from the patient's blood type are detected, the immune system will attack the donor cells (via the National Center for Biotechnology Information). This is why it is important that a donor is given the correct blood type during a transfusion.
Why is blood type important?
Blood type is determined by the presence or absence of two antigens found on the surface of red blood cells. These antigens are labeled A and B, along with a protein known as the Rh factor. The presence or absence of this protein determines if a person's blood type is positive or negative. The six blood types with either the A or B antigens are A+, A-, B+, B-, AB+, and AB-. Blood types that have neither antigen are type O and are classified as either O+ or O-. Type O negative blood is a universal blood type, meaning that it can be given to any recipient. Type O negative is in high demand at hospitals (via the American Red Cross).
Given that there are eight different blood types, it's crucial that a patient be paired with their matching type (unless type O negative is on hand). If you receive blood that has different antigens, your body's immune system will attack the donor cells with antibodies. This is what is known as a hemolytic transfusion reaction, or an ABO incompatibility reaction, and it can be serious (via MedlinePlus).
If you receive the wrong blood, chances are that you'll know fairly quickly. Symptoms include fever, chills, difficulty breathing, and nausea. Upon detecting a reaction, the medical staff will stop the transfusion and attach a saline drip to try and prevent stroke, kidney failure, or blood clotting (via Healthline).
Transfusion reactions are rare
There are a number of organizations in charge of keeping the blood supply in the U.S. safe. These include the Centers for Disease Control and Prevention, the U.S. Food and Drug Administration (FDA), and the National Institutes of Health. Donors are rigidly screened and asked a series of questions to determine if they are in good health and disease-free. In addition, all donated blood is tested for pathogens and blood type to ensure that it is properly labeled and goes to the correct, matching recipient when needed (via the Centers for Disease Control and Prevention).
Although you may never need a blood transfusion, it's a good idea for you to learn your blood type in case the situation ever arises. You can find out your blood type in a variety of ways, including asking your doctor, checking the next time you have blood drawn, or donating blood. You can also purchase an at-home blood test, although these aren't FDA-approved. If you have access to your birth certificate, it will also have your blood type (via Banner Health). The better prepared you are, the less risk you'll face if you ever require a blood transfusion.