Breast Cancer In Men Explained: Causes, Symptoms, And Treatments
For the average person, when breast cancer gets mentioned, women immediately come to mind. And considering most men tend to believe they don't have breasts (only the chest and pecks) it's easy to see why breast cancer occurring in women only is the common belief. However, even men develop breast cancer and it affects them pretty much the same way as women, although less often.
The breast tissue found in women is also present in men, but in a much lower quantity. And this puts them at risk of breast cancer (per Cancer Australia).
In the United States, the American Cancer Society predicts that about 2,700 men will get diagnosed with breast cancer in 2022, and the illness will claim the lives of around 530 of them.
A 2019 study published in the JAMA Oncology that looked at the mortality rate of women versus men in relation to breast cancer found that, after getting the diagnosis and confirming the existence of breast cancer, men are much more likely to die from this cancer than women. And among the reasons why men have a higher death rate is receiving the diagnosis when it's too late — mostly when the cancer has advanced to deadly stages (via the National Cancer Institute). Scarce information about male breast cancer may contribute to the late diagnosis and higher mortality rate.
We aim to help you learn everything you need to know about breast cancer in men so you can save yourself by detecting it early and get quick treatment before it becomes fatal. The information can also help you save another man's life.
The causes
The Mayo Clinic explains that the actual causes of breast cancer in men haven't been fully confirmed yet. However, one thing is for sure — the cancer comes about after a sudden and quick division of breast cells that create a cancerous tumor. Medical experts suggest that certain aspects like hormones and changes in your genes have a strong link to the occurrence of the illness (per the American Cancer Society). Starting with hormones, constant fluctuations in hormone levels cause the increase in size and division of breast cells — altering the DNA sequence in the process and paving the way for breast cancer.
As for gene changes — although the cause of gene changes isn't known — there are two ways experts suggest genes may cause breast cancer. First, when there are changes in the DNA (the substance that forms your genes), the genes that are responsible for accelerating cell division together with the ones that slow down the same process get affected. In turn, cancer begins developing due to the altered genes. Second, if altered genes get passed from your parents or grandparents — who had breast cancer — to you, you may get breast cancer too. The inherited altered genes found to bring about male breast cancer are normally referred to as BRCA1 and BRCA2 genes which regulate the increase and decrease in cell growth and division (via Stanford Health Care).
The different types of male breast cancer
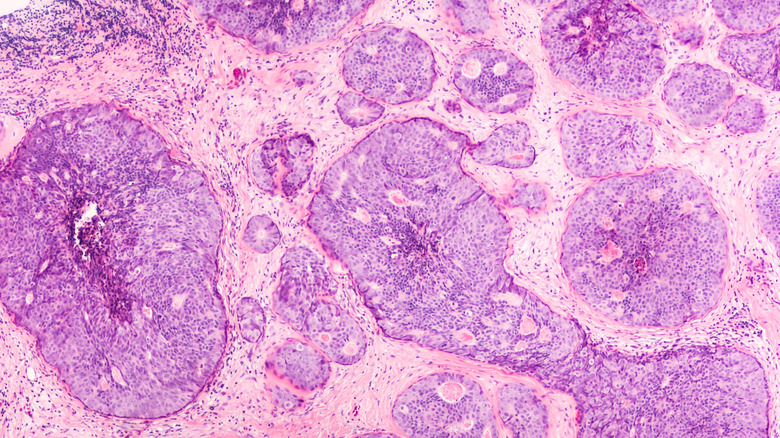
Breast cancer in men occurs in various types including ductal carcinoma in Situ and infiltrating breast carcinoma, explains Memorial Sloan Kettering Cancer Center. Ductal carcinoma in Situ is the type where the cancer-containing cells are present in your breast ducts. These cells don't affect the fatty tissue found in your breast and they also don't move beyond your breast to other body parts. The Perlmutter Cancer Center further adds that this type of cancer doesn't come about often and it's less severe compared to the second type — infiltrating breast carcinoma. Nonetheless, if the person who has it doesn't seek immediate medical attention, the cancer may advance, begin spreading and become dangerous with time.
In infiltrating breast carcinoma, the cancer mostly begins in your breast ducts (the slim tubes that transport milk to nipples) or the lobules (the milk-producing glands). It often stretches to other parts of your body like the breast tissue and lymph nodes and puts you at high risk. The Perlmutter Cancer Center also mentions Inflammatory breast cancer and Paget's disease as other types of male breast cancer. Inflammatory breast cancer resembles breast infection as it brings about redness and swelling on your skin. These two symptoms come about when the cancerous cells get to your breast skin and cause obstruction to the lymph vessels.
On the other hand, Paget's disease is a form of breast cancer that forms below your areola (the distinctly colored circular section on your breast that borders the nipple) and your nipple which makes them turn red, swell and even feel itchy.
Subtypes of infiltrating carcinoma
Infiltrating breast carcinoma comes in varying subtypes. The two most common subtypes are infiltrating ductal carcinoma and infiltrating lobular carcinoma (per the American Cancer Society). Infiltrating ductal carcinoma begins in the breast duct and spreads past the duct wall, and enters your breast's fatty tissue. It may even get to other body parts through your blood or through the network that carries the clear water-like fluid called lymph to your blood. The infiltrating lobule carcinoma subtype "is very rare in men, accounting for only about 2% of male breast cancers" (via American Cancer Society). It begins in the lobules and slowly finds its way to other breast sections and eventually other body parts.
Other recognized subtypes that are extremely rare include mixed carcinoma (that has a mixture of lobular carcinoma and ductal carcinoma's characteristics), adenoid cystic carcinoma (which occurs in your salivary glands, breast tissue, cervix, skin, prostate glands and various sections of your neck and head), low-grade adenosquamous carcinoma (which looks similar to a benign lesion and also has a less severe prognosis), medullary carcinoma (which mostly occurs in people with the BRCA1 altered gene), mucinous carcinoma (which develops in the mucin — the mucus cells — and which is less severe and can easily get treated), papillary carcinoma (which is distinctly characterized by protrusions like fingers known as papules), tubular carcinoma (which has a tube-like feature and may at times be present in the kidney or pancreas), metaplastic carcinoma (which keeps changing and can also get violent), and micropapillary carcinoma — which looks like the papillary serous carcinoma of the ovary, and spreads to the lymph node and shows aggressiveness (via Springer Link).
Risk factors
Certain factors including age increase your likelihood of developing male breast cancer. The risk of getting it heightens as you advance in age. The age at which most men get diagnosed with the condition is usually 65 years. Also, if in your family there's a man — perhaps your father, uncle, or grandfather — who's had it, chances are high that you may get it. If you also have more than two drinks every day, you stand the risk of getting male breast cancer. Additionally, if you don't exercise regularly, you could be at higher risk for developing breast cancer — exercise regulates your hormone levels and keeps them at favorable levels. Obesity is yet another risk factor (per the American Society of Clinical Oncology). The Cancer Causes & Control journal reports that obesity makes male breast cancer more likely to occur — mostly due to the hormonal interference it causes.
Additionally, the American Society of Clinical Oncology mentions that some treatments like those for prostate cancer and health conditions like liver cirrhosis and klinefelter's syndrome tend to boost estrogen levels and, as a result, increase the risk of male breast cancer. The American Cancer Society also highlights radiation treatment and other health issues like adult mumps, testicles that haven't descended, and surgical elimination of your testicles as other common risk factors.
The common signs of male breast cancer
The National Health Service insists that the one symptom that stands out across most male breast cancer cases is a breast lump. Certain features of the breast lump may help you determine if the lump is actually breast cancer — most lumps that occur in the breast are not always an indication of cancer. These features include a gradual increase in size, the lump occurring in one breast, the lump feeling knobby and rough, the lump is below the nipple or neighboring areas, not feeling any pain in the lump when it's touched, and there not being lump motion inside the breast.
Other than the lump, when you also notice you have swollen glands around your armpit, your nipple sinking in your skin, some discharge that's mixed with blood trickling down your nipple, redness, swelling, and hardening of the skin around your nipple, or a persistent nipple rash or sore, you should get checked by your doctor right away.
Some general symptoms like having a sickly feeling, feeling constantly exhausted, running out of breath, feeling itchiness in your skin coupled with a color change in your eyes and skin from normal to yellow, and pain in the bones may also indicate the possibility of breast cancer. The American Cancer Society also states that sudden appearance of dimples in your skin should be another cause for concern. Moreover, swelling around your shoulders — especially your collarbone — may mean the cancer may have begun spreading.
Diagnosing breast cancer in men
If you notice any of the above-mentioned symptoms, it's important to visit your doctor for a proper diagnosis. There you'll receive several tests and scans to help determine if you really have male breast cancer. Some of the common tests used in diagnosis include a breast ultrasound scan that checks for the presence and texture of a lump. Something you should prepare for is taking off your top as an ultrasound device gets placed on your chest and moved around for a clear image of the lump (if there is one) to be clearly seen on the screen.
Breast x-rays may also be part of your examination as they help expose lumps hiding in unexpected areas of your body. You may also need a breast biopsy — where the doctor extracts a tiny tissue of the breast, with the help of a needle, for further analysis (via the National Health Service).
The American Society of Clinical Oncology points out that a biopsy is the most accurate test for confirming the presence of cancer. There are a number of biopsies that help with diagnosing breast cancer: Fine needle aspiration biopsy (which works with a tiny and slim needle to extract a cell sample), core needle biopsy (which works with a needle that's much broader to extract bigger tissue samples), surgical biopsy (which extract a section of the lump, or the whole lump, through incisions), image-guided biopsy (used for instances where the doctor can't feel the lump) and sentinel lymph node biopsy (used to determine if cancer is present in the lymph nodes neighboring your breast).
The different stages of breast cancer
Staging breast cancer involves a well-known staging method referred to as the TNM system. T represents the tumor — how massive it is. N represents lymph nodes and seeks to determine if the cancer has reached any lymph nodes close to where the tumor is. M stands for metastasis, which shows the spread and effect of the cancer on other organs of your body and lymph nodes (per Memorial Sloan Kettering Cancer Center).
The American Society of Clinical Oncology further mentions that other numbers (one to four, for instance) accompany the letters T, N, and M, in the TNM system to give a clearer definition of the tumor. That means there are T1, T2, T3, and T4 categories and others that represent the exact category the tumor is in, size-wise.
The Memorial Sloan Kettering Cancer Center says there are five stages of breast cancer in men: Stage zero (where cancer cells haven't gotten beyond the breast duct and also haven't severely affected the fatty tissue in your breast), stage one (where the tumor's size is 2 centimeters or lower and hasn't touched the surrounding lymph nodes. If it has touched the lymph nodes, the extent shouldn't be more than 2 millimeters), stage two (where the tumor's size ranges from 2 to 5 centimeters and it's affected some armpit lymph nodes), stage three (where the tumor has not only affected the armpit's lymph nodes but other lymph nodes in your body) and stage four (where the cancer has gone beyond the lymph nodes to other organs like the brain, liver, lungs, or bones. Here, the size greatly varies.)
Surgical treatment
Treating male breast cancer through surgery comes with three options: Breast-conserving surgery, mastectomy, and sentinel lymph node biopsy. Breast-conserving surgery tries to conserve other unharmed breast sections. Lumpectomy — a popular type of breast-conserving surgery — aims to do away with the breast tissue that's cancerous together with some of the neighboring healthy tissue, and leave the other sections of the breast intact. Generally, breast-conserving surgery isn't common among men as it requires more breast tissue and men only have a tiny amount of it. Nonetheless, a few men opt for it when they don't want to have a mastectomy. A mastectomy involves getting rid of the breast entirely but leaving the muscles of the chest wall untouched (via the Memorial Sloan Kettering Cancer Center).
Per Breastcancer.org, there are three types of mastectomy: modified radical mastectomy (where the doctor removes your areola, nipple, the skin that covers your breast, the entire breast tissue, and a couple of lymph nodes in the armpit), simple mastectomy (where your doctor gets rid of the areola, nipple, your breast skin, and around two to five lymph nodes), and radical mastectomy (where your doctor get rids of everything that's targeted in simple mastectomy and also goes for the muscles of your chest wall). Radical mastectomy used to be the go-to type of surgery around the '70s but was later replaced and reserved for people who have cancer in their chest muscles and who had also undergone chemotherapy with no effective results.
As for sentinel lymph node biopsy, the Memorial Sloan Kettering Cancer Center notes that this form of surgery targets the sentinel lymph node "under the arm that is reached by tumor cells that have broken away from the tumor and spread through the bloodstream."
Non-surgical treatment options
Other than surgery, the National Cancer Institute mentions other interventions that help control and reduce male breast cancer which include chemotherapy, targeted therapy, hormone therapy, and radiation therapy. Chemotherapy involves working with medications that help minimize the cancer's growth and spread, by eliminating the cancer cells or inhibiting their division. Targeted therapy, on the other hand, targets particular cancer cells using medication without affecting normal cells. This is a much safer option than chemotherapy.
Some of the common forms of targeted therapy for men's breast cancer include tyrosine kinase inhibitors (that obstruct the tyrosine kinase enzymes which accelerate how cancer cells grow, take signals and divide), monoclonal antibody therapy (which works with synthetic proteins that help transport medication, radioactive materials and toxins to cancer cells), mammalian target of rapamycin inhibitors (which interfere with the mammalian target of rapamycin — a protein that's responsible for cell division and which increases the severity of cancer in your body), and cyclin-dependent kinase inhibitors (which inhibits kinase — an enzyme that's handles cell division, signaling, survival, and metabolism).
In hormone therapy, the treatment focuses on eliminating or regulating the effect of hormones such as estrogen and testosterone that play a role in the spread of cancer cells. Radiation therapy is a therapy that takes advantage of a high dose of radiation to completely clean out or regulate the growth of the cancer cells in your body. The American Society of Clinical Oncology also includes immunotherapy to the list of common non-surgical interventions for male breast cancer. Immunotherapy involves taking medication like pembrolizumab that powers up your immune system to deal with cancer cells.
Male breast cancer complications
Like all other types of cancer, if you get diagnosed with male breast cancer while it's still in the early stages, you stand a high chance of beating it and living a healthy life afterward (per the Mayo Clinic). However, when caught in the late stages, your chances of survival are extremely slim. The American Cancer Society points out that your chances of living an extra five years after diagnosis is 95% when the cancer is still within your breast and hasn't begun spreading, 83% if it's gotten to the neighboring lymph nodes, and 19% if it's gotten to the brain and other organs.
While treatment provides hope for managing the spread of cancer and sometimes eliminating it entirely, it may also drag along some nasty side effects with it. For instance, with surgery, there's a likelihood of experiencing needle-like sensations, becoming numb, having infections in the new wound, and sometimes feeling discomfort. Radiotherapy presents negative effects like getting a sickly feeling, exhaustion, short-term hair loss, and skin redness and soreness. Hormone therapy may decrease your urge for sex, make your moods unstable, make you add weight, have sleeping problems, and hot flushes. Chemotherapy may cause infertility, exhaustion, diarrhea, decreased desire for food, and proneness to other infections (via the National Health Service).
Prevention
As far as prevention goes, it's hard to protect yourself from male breast cancer since no confirmation of the real cause exists yet. However, you can work with some tips to help you minimize the risks.
Some of the things to keep in mind include a regular fitness program — engaging in moderate and intense fitness exercises has proven useful in reducing the chances of getting breast cancer in women. And since breast cancer in men and women is of the same nature, the same preventive measure can help men keep breast cancer at bay. You're advised to aim at working out moderately for a period between 150 to 300 minutes per week or do intense exercises from 75 to 150 minutes every week.
Also, you should watch out for weight gain and ensure you maintain modest weight (per the American Cancer Society). The Memorial Sloan Kettering Cancer Center stresses the importance of watching your diet. Fill your plate with plenty of vegetables (like peppers, mushrooms, cabbage, and tomatoes), whole grains (such as barley, brown rice, and quinoa), and whole fruits (kiwis and apples come to mind). If you decide to go for animal protein — like fish, chicken, eggs, or turkey — think one-third protein on your plate and two-thirds veggies, fruits, and whole grains.
Moreover, avoid alcohol — or ensure you don't have more than two drinks each day, according to the American Cancer Society.