What It Means When You Get Your Period Early
Most women probably remember the first time they had their period. No matter how prepared you were, it was most likely still a scary or weird thing to experience. After all, you are bleeding from a place where blood never used to come out before. And then they tell you it will last for a week and happen every month until your 50s? Terrifying. But then you eventually get into this rhythm, and if you are lucky enough, you can pretty much tell when your period is about to come. Some women only experience mild discomfort, while others cycle through intense cramps, mood swings, and other annoying period symptoms. Because of this, it is no surprise that women don't particularly enjoy getting their periods, and it can get really distressing if it comes unexpectedly.
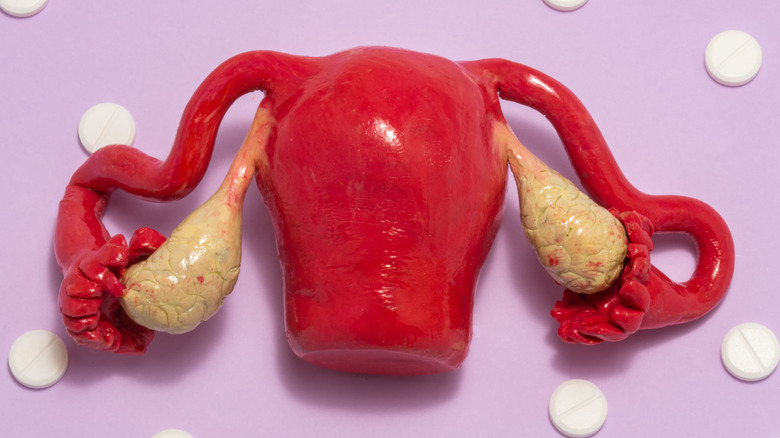
According to the Office on Women's Health (OWH), the average menstrual cycle lasts around 28 days, but this can vary among women. Bleeding occurs on the first day of your menstrual cycle, and ovulation (i.e., the release of an egg from the ovary) occurs 14 days before the start of your next period. For example, if your cycle lasts for 30 days, you will typically ovulate on Day 16. Aside from normal fluctuations, many things can cause periods to come early, such as hormone imbalances, lifestyle habits, and certain medical conditions. But other times, bleeding from your vagina may be something else entirely, and may not even be related to your period at all.
You are experiencing puberty
Puberty is a stage in life where the body undergoes many physical changes. It can begin around 8 to 13 years old, and may last for as long as six years. Girls develop breasts, pubic hair, and acne; go through a growth spurt; and get their first period. This unique physical transformation is brought on by dramatic changes in the body's hormone levels (via Sutter Health).
As the University of California San Francisco (UCSF) explains, the menstrual cycle is tightly regulated by the hypothalamic-pituitary-ovarian (HPO) axis. The hypothalamus (a structure located deep in the brain) secretes a hormone called gonadotropin-releasing hormone (GnRH) which stimulates the pituitary gland (also a structure in the brain) to secrete follicle stimulating hormone (FSH) and luteinizing hormone (LH). FSH stimulates the ovaries to produce estrogen (which thickens the lining of the uterus), while LH promotes the release of an egg from a follicle (i.e., ovulation). The follicle where the egg came from turns into a corpus luteum, which secretes the hormone progesterone. Progesterone turns the uterus into a habitable environment for an embryo to implant, but if fertilization does not occur, the lining of the uterus is shed and menstruation occurs.
This cycle is still immature during puberty, which means that girls will normally experience irregular periods that may not follow a particular schedule. According to WebMD, it can take up to two years before cycles become regular, but if irregular periods continue beyond that, something else may be causing it.
You are undergoing perimenopause
Similar to puberty, perimenopause leads to fluctuations in hormone levels. Perimenopause is the time in every woman's life where you transition into menopause, which is the complete cessation of menstruation. This process occurs gradually, and can last anywhere from 2 to 10 years (per Johns Hopkins Medicine). Periods can come early or late, and you may experience heavy bleeding, as well as other symptoms of menopause like hot flashes, problems with sleep, and mood swings (via Harvard Health Publishing).
It has been a well-known fact in the scientific community that women are born with only a specific amount of eggs in their ovaries, and their bodies do not have the capacity to produce more. This means that the older you are, the more menstrual cycles you have gone through, and the less eggs you have left in your ovaries. Eventually, your reserves will be completely depleted of functional eggs, and your ovaries will no longer be able to produce enough hormones to cause menstruation (via Healthline).
Interestingly however, a scientist named Jonathan Tilly published a study in 2004 where he claimed that he found stem cells in the ovaries of mice capable of making new eggs. In 2012, he and his team isolated germ cells from women's ovaries and implanted them into female mice, which he also claimed was able to stimulate egg production. Although the majority of experts do not support this, there are still a few who are trying to look into it further.
Sexually transmitted infections are to blame
Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) can be caused by pathogens like viruses, bacteria, and parasites. The Mayo Clinic states that you can have an STI without knowing it (i.e., asymptomatic STI), but some common symptoms include itching, pain during sex or when peeing, abnormal discharge from the cervix or vagina, heavy menstrual bleeding, and bleeding between your periods.
Usual infectious culprits of irregular periods are chlamydia and gonorrhea. A condition known as pelvic inflammatory disease (PID) occurs when these bacteria spread past the vagina and cervix, and infect other organs of the female reproductive tract like the uterus, fallopian tubes, and ovaries. As the Cleveland Clinic explains, PID is common among women in the United States (1 million cases every year) and untreated gonorrhea and chlamydia infections are responsible for 90% of all cases. The other 10% may be caused by abortion, childbirth, gynecologic procedures that involve the pelvis, and intrauterine device (IUD) insertion. If you have PID, you will most likely experience pain or tenderness in your abdomen, and you may also have fever, chills, nausea, vomiting, a malodorous vaginal discharge, and erratic periods or spotting throughout your cycle. Repeated episodes of PID can damage and scar your fallopian tubes, which can cause long-term pelvic pain, infertility, and ectopic pregnancy.
Healthline adds that untreated STIs can also lead to other dangerous complications like certain types of cancer (e.g., cervical), increased susceptibility to HIV, organ damage, and even death.
You are exercising too much or your weight changed drastically
Exercise is essential to staying healthy and protecting yourself from long-term illnesses like heart disease, diabetes, and osteoporosis. But when done excessively, even something as beneficial as physical activity can cause serious consequences.
Intense exercise has been associated with abnormalities in menstrual cycles as well as problems with fertility in women. These problems have been most commonly associated with high-performance athletes such as runners, weightlifters, and gymnasts. According to the American Fitness Professionals & Associates (AFPA), intense exercise can alter hormone levels, metabolism, and ovarian function, which altogether cause a disruption in the HPO axis, leading to irregular periods. Other factors that may also play a role include low body fat percentage (fat helps in estrogen production), early training (prior to puberty), increased testosterone in the body (including anabolic steroid use), and physical and mental stress.
Often coupled with exercise, a balanced diet is also part of observing a healthy lifestyle. Mount Sinai explains that dramatic and abrupt changes in your weight (whether you gain a lot or lose a lot), as well as the types of food that you eat, can cause your hormones to go out of whack and lead to irregular periods. According to a 2022 article from Bentham Science, this is particularly evident in people with eating disorders like anorexia nervosa. Additionally, unhealthy habits such as smoking and heavy alcohol use can also disrupt regular menstrual cycles and possibly cause heavier and more painful periods.
You are under stress or you changed your normal routine
Stress is a widely used term with a broad definition. It is defined by Buoy Health as the physical, emotional, or mental response your body experiences after exposure to certain strains or situations. During times of stress (including sleep deprivation, fasting, and physical exhaustion), the body produces a hormone called cortisol (via WebMD). Normally, cortisol helps the body manage energy sources, keep inflammation down, regulate blood pressure, maintain blood sugar levels, control the circadian rhythm (sleep-wake cycle), handle stress, and maintain internal balance.
Like the HPO axis, cortisol is regulated by the hypothalamic-pituitary-adrenal (HPA) axis (via Simply Psychology). The hypothalamus secretes cortisol releasing hormone (CRH), which stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH), which in turn causes the adrenal glands (organs on top of the kidneys) to secrete cortisol. When cortisol levels in the body increase to significantly high levels, the body tries to counteract this by decreasing production of hormones from the hypothalamus. While the downstream effect leads to a decrease in cortisol levels, the hormone GnRH, which is also produced by the hypothalamus, decreases as well. When GnRH levels drop, FSH and LH levels also drop, which prevents estrogen release and ovulation from happening (via Flo Health).
Similarly, changing your normal routine (e.g., working alternating day and night shifts) can also cause irregular periods. Although more studies need to be done, researchers believe that this may possibly be due to abrupt changes in your circadian rhythm (per Healthline).
You have polycystic ovarian syndrome
According to the National Institute of Child Health and Human Development (NICHD), polycystic ovarian syndrome (PCOS) is defined by a group of symptoms that are largely caused by hormone imbalance in women of reproductive age (i.e., females who have already started menstruating and have not reached menopause). It is diagnosed in women who have at least two of the three following characteristics: irregular or absent periods due to anovulation (i.e., absence of ovulation), symptoms of high androgen levels (e.g., excess hair on the face and body), and abnormal growths in the ovaries. Not all women with PCOS have growths in their ovaries, but if they do, these growths are said to be follicles that stopped developing due to anovulation.
Aside from menstrual irregularities, women with PCOS also have problems with fertility. The Centers for Disease Control and Prevention (CDC) says that PCOS is the most common cause of infertility in women in the U.S. Unfortunately, most women only find out they have PCOS when they are already trying to get pregnant but are unable to do so. Women with PCOS may also have patches of dark, velvety skin (i.e., acanthosis nigricans), and they are at an increased risk of developing other health conditions like diabetes, heart disease, high blood pressure, obstructive sleep apnea, stroke, depression, and anxiety.
Although PCOS is a long-term illness, a doctor can help you manage it. Medicines exist that can help regulate periods, treat skin symptoms, and help women get pregnant.
There are benign growths in your uterus
Benign growths in the uterus include polyps, leiomyomas (i.e., fibroids), and adenomyosis. Based on a 2019 article published in Fertility and Sterility, during the reproductive years, 8% to 12% of women will have polyps, 35% will have adenomyosis, and 70% of white people and 80% of Black people will have fibroids.
According to the Center for Menstrual Disorders, a polyp is a growth inside the uterine cavity, while fibroids are growths in any part of the uterus (inside, outside, or within the wall). Meanwhile, the Cleveland Clinic explains that adenomyosis occurs when the tissue that lines the inside of the uterine wall (i.e., endometrium) grows into the muscular layer of the wall (i.e., myometrium). All three of these abnormal growths can cause irregular periods, but they are each unique in terms of management.
About 27% of endometrial polyps resolve on their own after a year, but they also tend to recur 15-43% of the time. That being said, polyps can be removed through a procedure called polypectomy, but it's important to remember that it is very likely that they will come back. On the other hand, adenomyosis relies heavily on estrogen, which means that after menopause, symptoms often resolve spontaneously. But before that, adenomyosis can be managed using pain medications, hormonal birth control, or surgically removing the uterus (i.e., hysterectomy). Fibroids are treated similarly, but a myomectomy can also be done to remove fibroids while preserving healthy tissues in the uterus (via OWH).
You have other health conditions
Because the menstrual cycle is heavily regulated by hormones, certain conditions that can cause an imbalance in the body's hormone levels can also affect your period. Some of these conditions include type 2 diabetes, thyroid problems, and inflammatory bowel disease (IBD).
Women with type 2 diabetes are more likely to experience anovulation, which will cause them to have irregular periods. Likewise, studies suggest that women with irregular periods are more likely to develop type 2 diabetes compared to women with regular cycles. It is thought that irregular periods are related to high insulin levels in the body, which can lead to insulin resistance and cause type 2 diabetes (via Medical News Today). It is also worth noting that women with PCOS often have insulin resistance as well, and more than half will develop diabetes by the age of 40 (per the CDC).
Similarly, problems with the thyroid can cause many changes in the body. Per the Cleveland Clinic, the thyroid gland produces hormones that are important in maintaining balance in almost all processes in the body (e.g., metabolism, heart rate, body temperature, digestion). Specifically in women, thyroid hormone imbalance can cause early or late puberty and periods, anovulation, pregnancy complications, and even early onset menopause (via Johns Hopkins Medicine).
Although the reasons are still unclear, a 2014 study published in the journal Inflammatory Bowel Diseases found that cycle irregularities are common in women with IBD, especially changes in the length of their cycle.
You are taking certain medications
Medications are necessary to treat certain health conditions and are beneficial when taken appropriately. However, all drugs have their own side effects, and the decision to take a drug often relies on whether or not its benefits outweigh the risks. According to the U.S. Food & Drug Administration (FDA), adverse drug effects can be mild or severe, with the most common ones including upset stomach and drowsiness. In women, some drugs can cause changes in menstrual cycles, especially ones that affect the body's hormones.
Hormonal birth control (e.g., oral contraceptive pills, hormonal IUDs) mimics the body's natural release of hormones and often makes periods lighter, shorter, and more regular (per WebMD). Meanwhile, progestin-only pills can cause bleeding in between your periods during the first few months of taking the pill. Similarly, warfarin and aspirin (drugs that help prevent the formation of blood clots) increase a person's risk of bleeding, and can manifest in women as bleeding between periods. In women with thyroid problems, taking thyroid medications can also make periods irregular, which is why it is important that thyroid hormone levels in the body stay within normal limits. Likewise, antiepileptic drugs and chemotherapy can also cause absent or irregular periods.
Texas Health Care Obstetrics & Gynecology adds that herbal supplements can also cause irregular cycles in women, including ginseng, soy protein, and ginkgo biloba. Additionally, the Banyan Treatment Center warns that illicit drugs like cocaine and opioids can affect menstrual cycles and interfere with ovulation.
Implantation bleeding versus early period
When you experience bleeding or spotting from your vagina, the immediate thought is almost always that it is that time of the month again. But not all bleeding is caused by periods. If you are sexually active, implantation bleeding may be the cause.
The American Pregnancy Association explains that implantation bleeding occurs around 2 weeks after fertilization of an egg by a sperm, which is right around the time a regular period starts. In some women, it can happen earlier than their regular period, but bleeding is usually lighter and shorter in duration. It is called implantation bleeding because it is caused by the attachment of the fertilized egg to the inner lining of the uterus, and can be experienced by up to one-third of pregnant women. Although implantation bleeding and periods can present with similar symptoms (e.g., cramping, mood swings, breast tenderness, lower back pain), they are very different from one another.
One of the ways you can differentiate between them is by taking a home pregnancy test. This test detects the level of hCG in the body, which typically increases as pregnancy progresses. However, results can be falsely positive or falsely negative, so taking another pregnancy test after missing your next expected period will provide you with a more accurate result. If you are still unsure or you have concerning symptoms like persistent bleeding, pelvic pain, and weakness, you should consult your doctor as soon as you can (per Medical News Today).
Pregnancy loss versus early period
Pregnancy loss can either be a miscarriage or a stillbirth. According to the CDC, a miscarriage is the loss of a baby before 20 weeks of pregnancy, while a stillbirth is the loss of a baby at or after 20 weeks of pregnancy. Since women do not experience periods while they are pregnant, a miscarriage can be mistaken as a period, especially in the first few weeks of pregnancy or if they were unaware that they were pregnant.
Eight out of ten pregnancy losses occur during the first trimester (per Medical News Today). Many factors can contribute to a miscarriage, including genetic problems with the fetus, structural problems in the uterus or cervix, underlying medical conditions like diabetes and PCOS, intrauterine infections, and improper implantation. It is important to remember, however, that miscarriages are usually not preventable, and can happen without any clear reason.
During a miscarriage, pregnant women may experience bleeding (which may initially be light spotting, then heavy bleeding), passage of blood clots or grayish tissue, abdominal cramps that are often worse than period cramps, and low back pain. If you are experiencing any of these symptoms, even if you think you aren't pregnant, you should seek medical help right away. If it is in fact a miscarriage, all products of conception in your uterus should be removed, including the fetus and the placenta. Otherwise, you may end up with an infection, experience prolonged bleeding, or develop other complications (via the Cleveland Clinic).
Cesarean scar defect and bleeding after menses
If you had a cesarean section in the past and are experiencing abnormal bleeding, you may have a cesarean scar defect. A cesarean scar defect, a.k.a. isthmocele (via Hysteroscopy Newsletter), is often overlooked as a cause of irregular bleeding. The Mayo Clinic estimates that two-thirds of women who have had one or more births via cesarean section may have a cesarean scar defect, and around one-third of them have bleeding after the end of their regular period.
Not much is known about isthmoceles, but with cesarean section becoming more and more of a popular mode of delivery among pregnant women, the rate of cesarean scar defects are increasing as well. During a cesarean delivery, a cut is made on the uterus to access the baby. The cut is then sutured and typically heals within a few months. A 2016 article published in MD Edge explains that improper healing can cause the area of the suture to thin and form a pouch where blood can accumulate and eventually cause abnormal bleeding, pelvic pain, pain during sex, and infertility. Although the exact reason why the pouch develops is still unknown, it is suspected that certain surgical techniques, patient factors, and pregnancy factors increase the risk.
An isthmocele is typically diagnosed based on symptoms and findings on imaging tests (e.g., ultrasound, hysterosonography, hysteroscopy). Once the presence of a defect has been confirmed, management is aimed at relieving symptoms and restoring fertility through hormone therapy and/or surgical repair (via Hysteroscopy Newsletter).
Cancer and abnormal bleeding
One of the most common symptoms of cervical and endometrial cancer is abnormal vaginal bleeding. This can be seen as spotting, bleeding between periods, bleeding after sex, heavy or prolonged bleeding, or bleeding after menopause.
Cervical cancer is often caused by human papillomavirus (HPV), but not everyone with HPV will develop cervical cancer. It is frequently detected in women between 35 to 44 years old, and was formerly among the most common causes of cancer death in women in the United States, per the American Cancer Society (ACS). Mortality rates have dropped since regular screening using the Pap test was implemented. Aside from abnormal bleeding, women with cervical cancer may also have unusual vaginal discharge, pain during sex, pelvic pain, and bladder and bowel problems (via ACS). If your doctor suspects you have cervical cancer, they may take a sample from your cervix and have it analyzed in the lab.
On the other hand, according to the American College of Obstetricians and Gynecologists (ACOG), endometrial cancer often occurs in older postmenopausal women, but it can also be seen at an earlier age, especially in women who have hereditary conditions that increase their risk of developing cancer (e.g., Lynch syndrome). Other factors that can increase a woman's risk include high estrogen levels in the body (e.g., PCOS, estrogen-only pills) and being overweight with a body mass index (BMI) of more than 25. Symptoms are similar to cervical cancer; unfortunately, no screening tests are available for endometrial cancer.
What you can do
If you are experiencing irregular periods, one of the most important things to do is to keep track of your bleeding episodes and day-to-day symptoms. You can do this by marking it on a calendar, or using a period tracker application on your phone. Doing this will help you see patterns and fluctuations in your cycles that you may have never noticed before (via Buoy Health).
Self-care is also an important part of helping your body maintain internal balance. Flo Health advises women to avoid stress by practicing yoga, meditating, or doing something you enjoy (whichever works best for you). Although life in general can get pretty busy, try your best to eat a balanced diet, exercise regularly, and maintain a healthy weight. Aim to get enough good sleep every night (or day, if you work night shifts).
Healthline adds that ginger, cinnamon, and pineapple may help relieve menstrual symptoms. They are often used to help with irregular periods, but this has yet to be clinically proven. Some studies suggest that vitamin D can also help regulate menstrual cycles. Whether or not this is true, vitamins and minerals in general are essential for the body to function properly, so keep your daily recommended intake in mind when choosing the food that you eat and drink.
Lastly, consult a healthcare professional whom you trust and are comfortable with. Regular appointments with your doctor can help identify problems early on and correct them to prevent serious complications.