5 Major Ways Autoimmune Diseases Are Treated
When your immune system mistakenly attacks healthy cells in your body, this is known as an autoimmune disorder (via Medline Plus). According to Johns Hopkins Medicine, there are over 100 autoimmune disorders each coming with its own treatment options. Some of these conditions include lupus, multiple sclerosis, rheumatoid arthritis, and thyroid disease, per Johns Hopkins Medicine. Although scientists don't know the exact cause of autoimmune diseases, various factors play a role — infections, tissue damage, and genetics can increase your risk, according to the source.
Over 50 million Americans suffer from autoimmune-related conditions, with symptoms including fatigue, low-grade fever, and difficulty concentrating (via WebMD). While everyone is at risk of developing an autoimmune disease, it's more common in women of working and childbearing age, according to WebMD.
The symptoms of most autoimmune diseases may not be fatal but can be chronic. However, some autoimmune diseases are cited in the top 10 leading causes of death in women below 65 years (via Physiopedia). Furthermore, autoimmune disorders represent the fourth largest cause of disability among women in the United States, per the source.
The good news is that various treatment options exist for autoimmune conditions. Although the treatments can't cure autoimmune diseases, they help control the overactive immune response or reduce pain for better day-to-day living (via Healthline). Listed below are five major ways autoimmune diseases are treated.
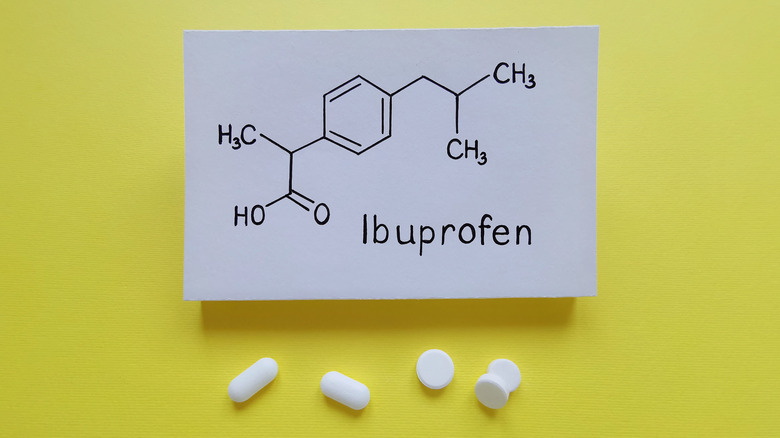
Anti-inflammatory medications
According to Medline Plus, inflammation (such as redness and swelling) is a common symptom of autoimmune disorders. To reduce inflammation, your doctor might prescribe an anti-inflammatory. These are part of a broad class of drugs called non-opioid analgesics, which are used by over 30 million people globally each day (via Medical News Today).
According to Healthline, over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs) such as aspirin, ibuprofen (Advil), and naproxen sodium (Aleve) are a common first-line treatment for autoimmune conditions like psoriasis and psoriatic arthritis because they can help reduce joint pain and swelling. NSAIDs can also reduce the action of inflammation-causing chemicals in people with lupus, per the Lupus Foundation of America. In one 2020 study published in the journal GLIA, anti-inflammatories showed promising results in slowing down the progression of multiple sclerosis. Taking anti-inflammatories via the intranasal delivery method might even help reduce inflammation symptoms in the brain, per the study.
While anti-inflammatories like NSAIDs can be effective in managing inflammation and pain associated with autoimmune disease, there are certain risks associated with long-term or excessive use (via Harvard Health Publishing). It's crucial to consult your doctor before taking any anti-inflammatory medications.
Corticosteroids
Corticosteroids come in various forms, including tablets, injections, sprays, gels, and creams. According to Medical News Today, doctors prescribe corticosteroids, like prednisone, to increase the effects of the hormone cortisol in the body, since the drug mimics this hormone. As the hormonal activity increases, the immune system, which activates inflammation in the body, becomes suppressed. This mechanism of action helps reduce inflammation symptoms, per Medical News Today. Corticosteroids can help reduce the inflammation, redness, and pain that come with autoimmune conditions like rheumatoid arthritis and systemic lupus erythematosus (via Cleveland Clinic).
However, gastrointestinal, heart, liver, thyroid, or kidney diseases as well as other medical conditions like diabetes, glaucoma, hypertension, or infections may affect the efficacy of corticosteroid treatment, per Healthline. After using corticosteroids, some people may be susceptible to side effects, including weight gain, high blood pressure, puffiness, hyperglycemia, depression, stomach irritation, and other skin infections, according to the source.
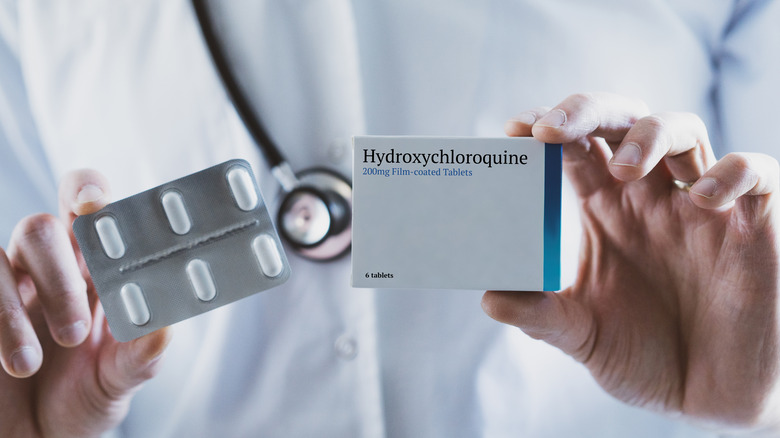
Immunosuppressant drugs
According to the American Academy of Allergy, Asthma & Immunology (AAAAI), in addition to steroids, immunosuppressant drugs like methotrexate, dapsone, sulfasalazine, and hydroxychloroquine can help with the treatment of various autoimmune diseases like lupus and rheumatoid arthritis. These drugs usually come as a tablet, capsule, liquid, or via injection (via Healthline). According to the Cleveland Clinic, immunosuppressants are potent in limiting the immune system from damaging healthy cells and tissues. According to the source, these drugs can help reduce symptoms and might even put certain diseases into remission.
Apart from reducing the production of inflammatory chemicals, some immunosuppressants also inhibit the actions of hyperstimulated immune cells, which helps control various symptoms of autoimmune diseases, per the Autoimmune Association. According to the source, healthcare providers consider immunosuppressants as part of the first-line therapy for most autoimmune diseases. However, immunosuppressants can increase your risk of infections as your body becomes less resistant, which makes treating infections more challenging, according to Healthline. Before prescribing the drug, your doctor will determine the specific drug that will effectively suppress your immune system and lead to fewer side effects. It's important to seek assistance from your doctor if you experience symptoms like fever or urination difficulties, per Healthline.
Painkillers
According to a 2017 study published in the Journal of Neuroscience Research, most autoimmune diseases have been linked with pathological pain. For instance, rheumatoid arthritis can cause severe swelling and pain (via WebMD). With time, inflammation from rheumatoid arthritis can affect your cartilage and bones, causing more pain and, in some situations, leading to disability. Besides anti-inflammatories and corticosteroids, your doctor might prescribe regular painkilling medications like acetaminophen (paracetamol), according to the NHS. These medications don't treat the condition but may be recommended while waiting to see a specialist for other treatments to help manage the autoimmune condition, per the NHS.
According to a 2020 article published by Informed Health Online, painkilling medications like acetaminophen are less effective for rheumatoid arthritis than non-steroidal anti-inflammatories. If you must use acetaminophen for pain relief from rheumatoid arthritis, the source advises using it in moderation, considering the possibility of side effects like liver and kidney damage, especially when taken in high doses. It's best to consult your doctor to prescribe an effective and safe dose — as a guide, the source advises keeping doses below 4 grams daily and to leave a six-hour interval between two doses.
Physical therapy
According to a 2017 study published in the journal Autoimmunity Reviews, physical activity is deemed safe when treating various autoimmune conditions like multiple sclerosis, rheumatoid arthritis, and inflammatory bowel diseases. Additionally, the incidence of these conditions is higher in people less engaged in physical activity, per the study. The source adds that people with rheumatoid arthritis who engaged in physical exercises reported a milder disease course with improved joint mobility.
As drug treatments for autoimmune diseases come with various side effects, physical therapy might be a better alternative. However, engaging in high-impact exercises like running and soccer might come with some risks, according to Medical News Today. Per the source, people with autoimmune diseases like rheumatoid arthritis may find low-impact exercises like swimming more favorable since they exert less pressure and stress on the joints.
According to another 2022 study published in the journal Autoimmunity Reviews, accumulating evidence supports the integration of exercise programs in managing multiple sclerosis. According to the study, physical exercise can significantly impact the quality of life by reducing fatigue and enhancing motor and cognitive function in people with multiple sclerosis.