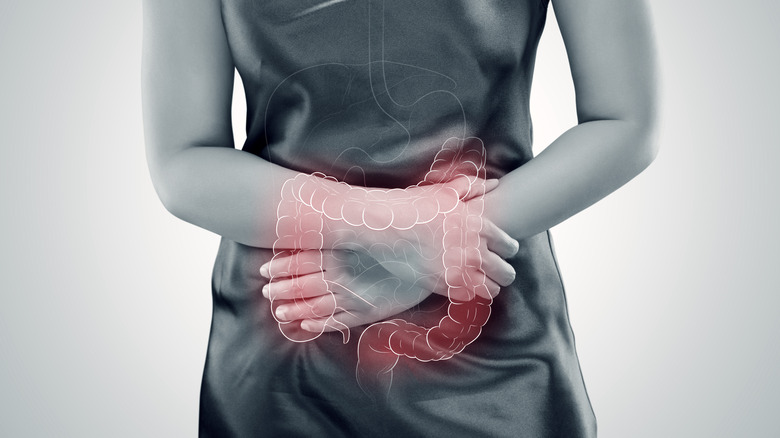
The Effects Of Crohn's Disease On The Body
Crohn's disease is an inflammatory bowel disease (IBD) characterized by inflammation of the gastrointestinal tract (via the Mayo Clinic). While it can affect the whole intestine, it most frequently impacts the last part of the small intestine, called the ileum, according to a 2020 review published in Biology Direct. The review also explains that while this is a chronic condition, people with Crohn's disease can have periods of flares that alternate with periods of remission — meaning that their symptoms come and go. In addition, according to the Mayo Clinic, symptoms of Crohn's disease vary from one person to another, ranging in both severity and in the time it takes for symptoms to develop.
The cause of the disease is still unknown, but Crohn's is believed to be an autoimmune condition in which the body's immune system malfunctions and attacks its own digestive tract (via Johns Hopkins Medicine). Nevertheless, there also seems to be an important hereditary factor, seeing that the condition is commonly present in members of the same family. There is currently no cure for this disease, but people can achieve long-term remission with therapy and medication, the Mayo Clinic says. While Crohn's disease is an intestinal condition, you may also experience some non-intestinal symptoms that can be just as problematic. This article reviews some common signs and side effects that Crohn's disease can have all over your body.
Fatigue
Feeling tired or fatigued is quite common for people with Crohn's disease, who report memory lapses, poor concentration, and generally low energy (via Healthline). Naturally, these symptoms can affect someone's productivity at work or school, reduce quality of life, and negatively impact their relationships.
Per a 2019 study published in the journal Inflammatory Intestinal Diseases, while fatigue is more common in people with active Crohn's disease symptoms — showing up in 80–83% of the study's participants — it remained present in 39–44% of those who were in remission. According to the study, fatigue can be felt mentally or physically (or both) and is often attributed to factors such as disease severity and duration, age, gender, and psychological or lifestyle factors. According to the Mayo Clinic, fatigue in people with Crohn's disease can be hard to treat due to its multiple potential causes. However, your doctor may help you manage it by switching up your medication, making sure you don't have vitamin or mineral deficiencies (in which case they could suggest supplementation), and recommending psychological therapy. Furthermore, following a healthy diet, staying physically active, getting enough sleep, and staying well hydrated may help as additional strategies to combat fatigue.
Mouth sores
Mouth sores are present in up to 50% of people with Crohn's disease — and they're even more frequent in children, according to a 2021 review published in Gastroenterology. Medical News Today describes such sores as being small, round- or oval-shaped, and yellow or gray in color with a red border.
According to a review published in the World Journal of Gastroenterology, mouth sores and other oral wounds can happen in people with Crohn's disease and other IBDs even when intestinal symptoms haven't shown up. In fact, they may appear years before intestinal symptoms appear, and in up to 60% of cases they are the primary initial sign of Crohn's. For this reason, the review explains that recognizing patterns in the appearance of mouth sores can help doctors to offer a timely diagnosis and monitor the disease's activity. This type of sore can be painful, impair oral function, and lead to nutritional disorders due to the elimination of triggering foods, or just because eating becomes uncomfortable and unpleasant. Moreover, the review states that since some may appear on the outer side of your mouth, they can also lead to mental health problems. Mouth sores are commonly treated with topical steroid creams or medicated mouthwashes (via Gastroenterology).
Anemia
Anemia is a blood condition characterized by a low red blood cell count or, more specifically, a low count of hemoglobin — the protein in charge of carrying oxygen to your organs and tissues (via WebMD). Per a study published in Expert Review of Gastroenterology and Hepatology, anemia is one of the most common non-intestinal complications in Inflammatory Bowel Diseases (IBD) such as Crohn's disease.
According to a review published in Nutrients, the European Crohn's and Colitis Organisation (ECCO) guidelines categorize anemia in IBD patients as iron deficiency anemia (IDA), anemia of chronic disease (ACD), B12 deficiency-associated anemia, and drug-induced anemia. IDA is potentially caused by iron loss from bleeding or impaired iron absorption or intake. In contrast, ACD can occur due to abnormalities in iron transport, inhibition of red blood cell production, or due to iron being trapped in white blood cells. Lastly, B12 deficiency anemia is primarily caused due to nutrient malabsorption. While an exact origin can be challenging to determine due to the multiple potential causes, the review reports that IDA may account for up to 90% of anemia cases in those with an IBD.
Due to iron's role in oxygen transport, people with anemia might present chronic fatigue, headaches, dizziness, fainting, and pale skin, nails, and conjunctiva (the pink membrane that covers the inside of your eyelids). In severe cases, anemia could lead to heart and thyroid problems, impaired mental performance, and increased risk of infection. In short, it may deteriorate your overall health. The good news is that you can easily treat anemia with oral iron supplementation or intravenous (IV) iron (via Expert Review of Gastroenterology and Hepatology).
Depression and anxiety
Crohn's disease has been linked to higher rates of depression and anxiety, which is why treating its emotional symptoms is just as important as treating the physical ones (per the Crohn's & Colitis Foundation). Depression is a mood disorder characterized by feelings of sadness, exhaustion, hopelessness, helplessness, and worthlessness. In contrast, anxiety shows up through feelings of worry, panic, and nervousness.
Though emotions like anxiety or stress don't cause Crohn's disease, they can contribute to flares. In turn, the fear of flare-ups tends to feed said stress and anxiety, leading to a spiraling harmful cycle. Similarly, when the disease flares up or becomes active, people may feel like they've lost control of both the illness and their bodies, which might lead to depression (via Healthline).
Some tips for managing Crohn's-related depression at home include remembering that the disease does not define you, that flare-ups are followed by periods of remission, and finding something to look forward to. As for at-home anxiety management, the Crohn's & Colitis Foundation (CCF) recommends practicing relaxation and breathing exercises, creating a support network, and keeping a routine filled with activities or hobbies you enjoy. Seeking professional help is also recommended in both cases.
Bowel obstructions
Bowel obstructions are a common complication of Crohn's disease. Being an inflammatory condition, Crohn's leads to prolonged swelling of the intestinal walls, which narrows down the intestinal canal where food or stool would have to pass through — a complication called a stricture (via Medical News Today). Strictures can happen one of two ways with Crohn's. When they're caused by inflammation, they are inflammatory strictures. Fibrotic strictures occur when the narrowing happens due to the buildup of intestinal scar tissue — this can happen as a result of long-term inflammation.
Per a 2015 review published in Intestinal Research, up to 50% of people with Crohn's disease will develop strictures within 20 years after diagnosis. These could happen in either the small or large intestine. Most of them will need at least one surgery during their lifetime to fix them — especially in the case of fibrotic strictures, which don't respond to anti-inflammatory therapy like inflammatory strictures. The review lists genes, age, use of steroid treatment, history of smoking, and ulcers in the small bowel as potential risk factors for developing strictures. Some signs that you might be developing intestinal strictures include mild to intense abdominal pain and bloating, reduced appetite and energy, excess gas, constipation, and vomiting (per Medical News Today).
Diarrhea or constipation
Diarrhea and constipation stand at the opposite end of the bowel movement-disease spectrum, and both can make their way into the lives of people with Crohn's disease. Diarrhea is a frequent symptom of the disease (via WebMD). Aside from the typical loose stools, you might also experience bloody stools, abdominal cramps, sudden urges to poop, and even weight, vitamin, and mineral loss. Per a study published in the Journal of Crohn's and Colitis, the most common causes of Crohn's-related diarrhea include water and electrolyte imbalances and increased concentrations of bile acids, both caused by intestinal malabsorption.
On the other hand, constipation happens when you have difficulty passing stools (per Healthline). While Crohn's disease's complications such as bowel obstructions or strictures might be a potential cause, constipation is more often related to Crohn's-related lifestyle factors, such as following a low-fiber diet to avoid irritation or not exercising or drinking enough liquids, as well as the need to take multiple medications.
Treatment for Crohn's-related diarrhea and constipation also requires opposite techniques. According to WebMD, some tips for managing diarrhea include avoiding high-fiber grains, fruits, and vegetables or following a low-FODMAP diet, managing stress, and taking probiotics. In contrast, to combat constipation, Medical News Today recommends adding more fiber to your diet, drinking more fluids such as water, soups, and fruit and vegetable juices without added sugars, exercising more, and implementing bowel training, which consists of trying to set a bowel movement schedule.
Ulcers
According to the Centers for Disease Control and Prevention (CDC), an ulcer is an open sore in the lining of the stomach or small intestine, a condition affecting up to 25 million Americans. However, in people with Crohn's disease, ulcers can appear pretty much anywhere in the gastrointestinal tract, from the mouth all the way to the anus, including the esophagus, stomach, appendix, and small or large bowels (via Healthline).
Crohn's-related ulcers can often lead to other common complications of the disease, such as anemia from constant low-grade blood loss; bleeding, which may happen if an ulcer reaches a large blood vessel; and fistulas, areas where a ulcers have created holes through the intestinal walls. Depending on the severity and location of the ulcers, treatment may include topical medication, antibiotics, immunosuppressants or drugs that calm your immune system, or surgery. Lifestyle management can also help reduce the frequency and duration of some ulcers.
Anal fistulas
According to a 2019 study published in the journal Clinics in Colon and Rectal Surgery, anal fistulas are a common problem affecting up to 43% of people with Crohn's disease. Moreover, in up to 45% of the cases, they may appear almost five years before the intestinal symptoms. A fistula is defined as an abnormal passage formed in an organ, such as like the bowel (via CCF). This passage can lead to another organ, or can totally penetrate body surface. In the case of anal fistulas, the opening appears in area surrounding the anus.
The study explains that anal fistulas are painful and may lead to fecal incontinence, scarring, anxiety or depression, and a decreased quality of life. In addition, those who develop anal fistulas are more likely to experience other non-intestinal complications, such as arthritis or skin issues. Anal fistulas must be treated right away to prevent infections (per CCF). While some may heal with medication such as antibiotics, severe fistulas may require a surgery called fistulotomy.
Vitamin D deficiency
Vitamin D is a fat-soluble vitamin needed for bone, muscle, nerve, and immune health, according to the National Institutes of Health (NIH). Additionally, research suggests it plays a critical role in inflammation and gut health. According to a 2019 review published in Nutrients, vitamin D helps keep your bowel lining in good shape. However, its deficiency is very common in people with inflammatory bowel diseases (IBD), especially those with Crohn's disease.
As a matter of fact, per a 2016 study published in the World Journal of Gastroenterology, vitamin D is inversely related to inflammatory conditions like Crohn's disease. This means that the lower the vitamin levels, the higher the risk of developing the disease. In addition, the study determined that its deficiency can even worsen the disease's progression, leading to an increase in the number and severity of its flares. Nevertheless, researchers still haven't figured out whether the deficiency is a cause or consequence of the disease.
Multiple factors may lead to vitamin D deficiency in people with Crohn's disease, including limited intake of vitamin D-rich foods, impaired nutrient absorption, and lack of sun exposure due to medicinal therapy (via Nutrients). However, supplementing with the vitamin may bring numerous benefits, such as reduced inflammatory markers, lower risk of anemia, improved response to anti-inflammatory treatments, and a reduced risk of surgery.
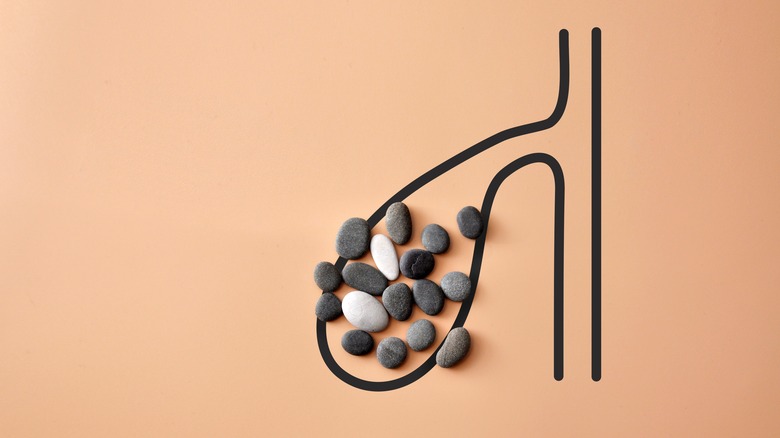
Gallstones
Your gallbladder is a small organ that stores bile produced by your liver to use it to digest dietary fats. However, when bile accumulates, it can form one large or multiple small stones known as gallstones (via Medical News Today). According to a 2022 review published in the journal Cureus, people with Crohn's disease have a 14% increased risk of developing gallstones compared to the regular population. The primary reason for this is that intestinal inflammation interrupts the mechanism of bile excretion from the gallbladder and the process of reabsorption in the small intestine. However, a 2017 study published in the journal PLoS One states that high bilirubin levels and long periods of fasting (which are common in people with Crohn's disease) can also be potential causes.
Per another study published in Hepatology, additional risk factors for gallstone formation include age, disease duration, more than three high-dose steroid treatments, more than three hospitalizations, long hospitalization times, and a specific intestinal surgery called an ileostomy. Common gallstone symptoms often include bloating, nausea, abdominal pain after meals, fever, and vomiting (per Healthline). Their treatment mainly depends on the severity of the symptoms, but it usually requires surgically removing your gallbladder.
Kidney stones
Your kidneys are the organs in charge of filtering your blood to eliminate waste through urine. Though it's rare for them to suffer serious damage due to inflammatory bowel diseases, someone with Crohn's might experience less severe complications (per the CCF). Kidney stones are the most common kidney complication in people with Crohn's disease. These happen because inflammation in the small intestine impairs fat absorption, leading to the buildup of a compound called oxalate — in turn, this oxalate can crystalize and form oxalate stones.
Per a 2017 study published in the journal PLoS One, other risk factors for kidney stones in people with Crohn's disease include low urine acidity, reduced urine volume due to diarrhea, low magnesium absorption (since magnesium can help prevent the formation of oxalate stones), intestinal surgery, being assigned male at birth, and reduced physical activity. Symptoms of kidney stones include sharp pain, bloody urine, nausea, and vomiting (via CCF). While small stones may pass spontaneously or by themselves, larger stones may require a surgical intervention.
Joint pain
Joint issues can manifest in people with Crohn's disease in two different ways, either through joint pain (called arthralgia) or joint inflammation (called arthritis). Joint problems affect up to 46% of people with intestinal bowel disease (IBD), per a 2021 review published in the journal Gastroenterology. Interestingly, the study states that while joint problems typically affect older people, the prevalence of arthritis in Crohn's disease actually decreases with age, meaning that it is more common in younger people. For example, the review notes that joint inflammation was present in nearly 25% of people in the 20– to 30-year age group, compared to just 2% of those in the 50– to 60-year age group.
According to the CCF, there are different types of arthritis in Crohn's disease that affect different parts of the body, including large joints of arms and legs like elbows, wrists, knees, and ankles, smaller joints in your lower back. In rare cases, it can affect areas such as the eyes, lungs, and heart valves. Unlike regular cases of arthritis, Crohn's-related joint pain and inflammation are usually treated by managing inflammation in the colon or large bowel. Additionally, your doctor may prescribe physical therapy, rest, or recommend applying heat to the affected area.
Eye problems
Among people with inflammatory bowel diseases, those with Crohn's disease are more prone to having eye problems than people with ulcerative colitis, according to a 2021 review published in the journal Gastroenterology. In fact, per the review, the eye is the third major non-intestinal organ affected by the disease, with up to 7% of people presenting ocular manifestations — with a higher rate among children than adults. In addition, those who present with eye problems are more likely to show skin and joint manifestations as well.
The three most common eye issues associated with Crohn's are scleritis (inflammation of the tissue covering the eye), episcleritis (inflammation of the eye's surrounding tissue), and uveitis (inflammation in the middle layer of the eye). Symptoms of each may include eye redness, sensitivity to light, blurry vision, pain around the eye, and watery eyes, according to Medical News Today. The site also lists dry eye and keratopathy — a disease of the cornea — as additional potential ocular problems. Treatment for eye complications depends on the manifestation. While some may improve by controlling their Crohn's disease, others may need anti-inflammatory medication.
Skin problems
According to a 2021 review published in the journal Gastroenterology, skin problems have been reported in roughly 5–15% of people with Crohn's disease, and while there are over 10 different disorders, red bumps and blisters are the most common ones. Per the CCF, red bumps typically appear on the shins and ankles when the disease flares up, and they're more common in people assigned female at birth. Similarly, blisters also develop in the shins and ankles, though they may also appear on the arms. While they may start small, Crohn's-related blisters can join together and form large and deep ulcers in the skin.
Other potential skin complications that might develop in people with Crohn's disease are sores, tears, acne, psoriasis, rashes, skin tags, purpura, and skin color loss (via Healthline). According to the CCF, while skin issues are primarily a direct manifestation of the disease, in some cases they might be caused by medications used as treatment. Therefore, even if controlling the disease may lead to improvement, treatment of these skin conditions may vary depending on the cause.
Low bone density
Bone density or bone mass is a measure that tells you how strong your bones are according to the amount of bone tissue present in your skeleton (via Livestrong). According to the CCF, around 30–60% of people with Crohn's disease have lower bone density than the general population. Low bone density or bone loss can lead to osteoporosis (a condition that increases the risk of bone fracture) or osteomalacia (a condition that leads to soft bones), and it is more common in people assigned female at birth.
Per a 2021 review published in the journal Cureus, multiple causes or risk factors can lead to bone loss in Crohn's disease, including inflammation, long-term use of steroid medication, and malnutrition due to impaired absorption of key nutrients for bone health — namely vitamins K, D, B12, and calcium, which are essential for bone metabolism. Therefore, the CCF lists taking vitamin and mineral supplements, talking to your doctor about reducing your steroid use, staying physically active, limiting alcohol consumption, and quitting smoking as potential preventive measures to reduce the risk of bone diseases.
Menstrual irregularities
Crohn's disease may add one more complication to people assigned female at birth by messing with their menstrual cycle. According to Healthline, inflammation caused by the disease may interfere with the levels of certain hormones involved in period symptoms. In addition, taking steroid medication and being underweight (both of which are common in people with Crohn's disease) are other known risk factors for menstrual irregularities, which may delay your first period or make your cycle erratic and hard to track.
In fact, per a 2015 study published in the journal Inflammatory Bowel Diseases, 25% of the participants had a change in their cycle regularity the year before being diagnosed with Crohn's disease. Similarly, 21% experienced changes in their cycle length, and 40% had heavier flows and increased menstrual pain. According to Healthline, a common way to manage said irregularities is by taking birth control pills. Those with Crohn's may want to avoid treating period symptoms with standard over-the-counter medications like ibuprofen and aspirin, as these common NSAIDs may trigger a flare.