What Happens To Your Body When You Have MRSA?
The advances in modern healthcare seem to know no bounds, and nowadays, medicine can work with almost mind-blowing efficiency. But the fact remains that there are still conditions that can elude easy treatment with medication, and some of them may be right under our noses –- quite literally, that is.
MRSA (methicillin-resistant staphylococcus aureus) is one of these, a strain of staph bacteria that can cause a pretty unpleasant infection, working its way into open sores and wounds (per Johns Hopkins Medicine). Not only does MRSA make them worse, but it also produces a host of other symptoms. MRSA is notable not just because it's challenging to treat with antibiotics (thanks to the bacteria's resistance to classic medication), but also because a lot of people carry it without even knowing. In fact, a third of people carry the bacteria that leads to an MRSA infection around in their noses every day, according to the Centers for Disease Control and Prevention (CDC).
While a lot of those people don't necessarily become infected by the bacteria that their skin's hosting, it's important to know what an MRSA infection looks like, and what changes occur to your body when they happen. Let's take a deep dive into the ways an MRSA infection affects a person.
How does MRSA spread?
MRSA is commonly spread via skin-to-skin contact or contact with objects contaminated with the bacteria (per the CDC). Although many people carry MRSA around with them without becoming ill, the infection starts when the bacteria come into contact with open skin or an abrasion. After that, it's able to work its way into the body. And the bad news is that MRSA can spread pretty easily.
While the bacteria may move from person to person within a community, it can be a particular problem in healthcare settings like hospitals (per Health and Social Care), as well as nursing homes. In these locations, individuals are usually more likely to be affected by MRSA thanks to the fact that they're already in poorer health, giving the bacteria more of an opportunity to take hold. MRSA may also be more likely to affect opioid users.
To avoid contracting MRSA, it's vital to follow basic hygiene measures. Make sure you're washing your hands and your body frequently and properly, use your own hygiene items, and tend to any wounds or abrasions immediately and thoroughly, keeping them covered.
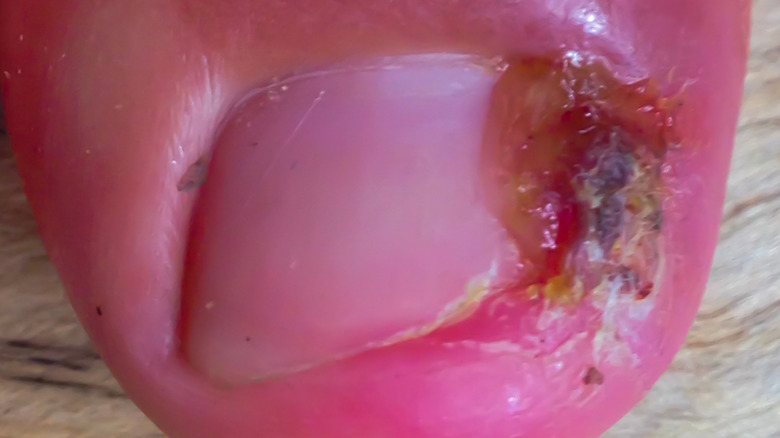
MRSA causes skin changes
While MRSA can live harmlessly on the skin, once it enters your body, it can start to produce symptoms relatively quickly. Most commonly, MRSA infections produce bumps on the skin, which are generally pretty painful, as the Mayo Clinic discusses. These bumps can often be mistaken for other things like insect bites or even pimples (per Healthline), and can often be especially warm, red, or swollen.
It may not stop there, though. These bumps may eventually open up, creating excruciating open sores, abscesses, or ulcers that can also be accompanied by other symptoms. If this happens to you, immediate treatment is essential, as the Michigan Department of Health and Human Services advises. Speak with your doctor about any potential medications you can take to treat the illness, and follow their hygiene guidance to the letter to avoid further spread. This usually includes cleaning the wound and the surrounding skin thoroughly, ensuring any bandages you've used are thrown away immediately, disinfecting any surfaces that you're in contact with, and washing your clothes and sheets properly using hot, soapy water.
You may get pus-filled growths
As MRSA gets under your skin and the infection begins to impact your body, painful red bumps can begin to appear, which are normally filled with pus (via Johns Hopkins Medicine). These bumps may be isolated, or may appear in a cluster or group.
This pus production is all part of your body's natural system of fighting infection, as Healthline explains. Your body responds to any foreign bodies coming into your system by releasing a flood of white blood cells to fight them off. These white blood cells die, along with some of the tissue where the infection's present. Pus is essentially dead matter.
Tackling these pus-filled bumps can be unpleasant, but it's also one of the ways that MRSA is treated (per Healthline). Your doctor will cut into the bump or growth and drain out the pus, which may then be used to determine which antibiotic should be used for your treatment (if you need them for recovery). Whatever you do, under no circumstances should you try and drain the pus yourself –- leave that to a healthcare professional.
MRSA can enter surgical wounds
MRSA can strike when you least expect it, and also when you're at your most vulnerable. And one of those times is after you've had surgery, as research published in Cochrane states. While for some surgeries, the possibility of developing MRSA in a surgical site is low, for others it may occur in up to a third of surgical procedures. Worse, treatment for post-surgery MRSA can be incredibly challenging due to its antibiotic resistance.
If you're concerned about contracting MRSA after surgery, it's wise to discuss any anxieties you have with your doctor, as they'll be able to advise you on how best to limit the risk of infection. They may suggest, for example, that you don't shave the location of the surgery, as this may raise the risk of infection (per bioMérieux Connection). Additionally, taking actions like limiting smoking post-surgery and avoiding too much physical contact with the surgical wound can help to keep the risk of infection at bay (per Johns Hopkins Medicine). Continue to communicate with your doctor post-surgery, and inform them of any changes to the surgical area (particularly redness) or if you develop a fever.
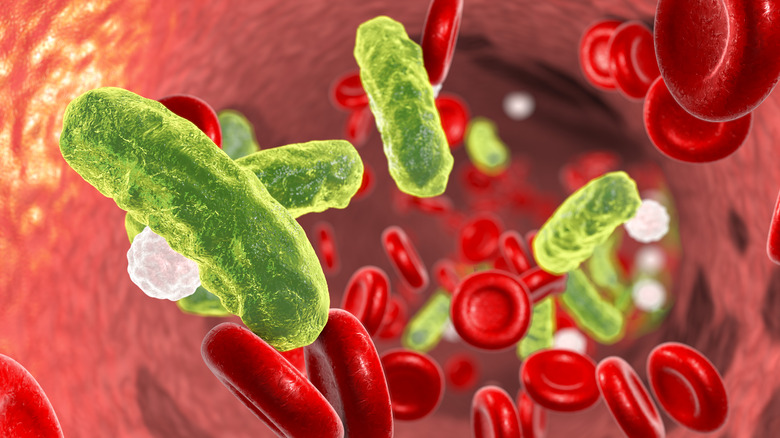
The infection may also make its way into your blood
While MRSA commonly affects the skin, it can also have a greater impact on your body as a whole. The bacteria that cause MRSA can go from the entry point on your body, usually an open wound, into your bloodstream, a condition known as bacteremia (via Healthline). When this occurs with an MRSA infection, the consequences can be incredibly dangerous, with sepsis and even death as possible outcomes (per the CDC).
That's why it's highly important to watch out for any symptoms of bacteremia and to act immediately if you see them. Changes in breathing and a quickening heart rate, as well as fever or getting shivers, are all signs. Individuals who develop bacteremia from MRSA will usually undergo a course of antibiotics, administered in a hospital setting via an IV drip, according to research published in Clinical Infectious Diseases. Vancomycin and daptomycin are two medications that may be used, which could be administered for up to six weeks if the bacteremia becomes complicated. For less severe cases of bacteremia, roughly two weeks of antibiotic treatment can be enough to get rid of the infection.
MRSA in the lungs can be incredibly dangerous
Once MRSA bacteria gets into your blood, it can travel from the point of infection to any part of your body. And one of the most dangerous places it can end up is in your lungs.
The abscesses full of pus that manifest on your skin in a classic MRSA infection can form in your lungs, according to Healthline. The MRSA bacteria can also cause a large accumulation of pus between tissues, specifically between your lung and the tissue that encloses it in your chest, a condition known as empyema (per Johns Hopkins Medicine). Both of these complications can lead to pneumonia, which can be very dangerous and can cause your lung tissue to die, per research published in the European Respiratory Journal.
Symptoms of lung-based MRSA can be adjacent to other respiratory conditions, with coughing and shortness of breath common (the latter sometimes caused by the pressure on the lungs from empyema). You may also have blood in your phlegm, as well as more generalized symptoms like a fever. For pneumonia stemming from MRSA, immediate and rigorous antibiotic or antibacterial treatment is required, with vancomycin and linezolid often used (per research published in Cureus).
In some instances, it can cause endocarditis
When MRSA enters your bloodstream, it's only a matter of time until it passes through your heart. And if the bacteria starts to infect this organ, it can cause inflammation of the tissue within the heart, a condition known as endocarditis (per the Mayo Clinic).
Endocarditis is an incredibly serious and potentially fatal condition. It can have a rapid onset and cause symptoms similar to other heart conditions, like an aching chest, muscle pain, or a heart murmur. Elsewhere, endocarditis can create symptoms that may be confused with other illnesses, with some signs (like shivering, night sweats, or feeling more tired) appearing more like the flu or a seasonal bug.
Endocarditis is especially serious for individuals who have pre-existing heart conditions, and if MRSA prompts it, it should be treated as soon as possible. The good news, however, is that the condition is rare in terms of being a result of MRSA, according to research published in Clinical Infectious Diseases. Endocarditis appears to be most common from MRSA when the infection occurs among individuals who use intravenous drugs. As with other MRSA infections that spread to organs, this form of endocarditis may be treated with vancomycin, as well as other antibiotic medications.
MRSA can also cause issues for your bones
MRSA may primarily affect the skin, but it's not just skin-deep. In fact, in certain circumstances, MRSA can work its way down to the deepest level of your body, impacting your bones and your joint health (per Medical News Today).
The MRSA infection often appears in your arm and leg bones. It can also affect your spine, resulting in an infection called osteomyelitis. This condition, which causes your bones to swell and become inflamed, can result in pain, mobility issues, stiffness, and a fever, and is usually treated through a course of antibiotics and, on occasion, surgery (per Johns Hopkins Medicine).
MRSA can also prompt septic arthritis (via Medical News Today). If this occurs, it's vital to act quickly. A form of arthritis caused by the bacteria making their way to your joints (usually your hips or knees, says Versus Arthritis), this is an excruciating condition with a rapid onset. It may also require surgery to tackle, often to drain out the infection from the joint. As with other MRSA infections, a high fever can be a symptom of septic arthritis, as well as severe joint pain, swelling around a joint, and difficulty bearing weight or operating the body parts it affects.
MRSA may also affect your eyes
MRSA can be a serious problem for a lot of areas around your body, and this includes your eyes. While MRSA that affected the eyes was once less common, the infection has grown in prevalence, states the University of California's David G. Hwang (via the American Academy of Ophthalmology). "Even four or so years ago, I would see only a handful of MRSA cases each year, and now I see such cases routinely every few weeks; it has moved from a theoretical concern to the actual," says Hwang.
MRSA infections in the eye can cause abscesses in the lid area as well as symptoms of conjunctivitis, but other symptoms can be more profound and could potentially lead to a loss of eyesight, according to research published in Transactions of the American Ophthalmological Society.
As with other MRSA infections, antibiotic resistance can be a significant hurdle in tackling the infection. Hwang states that cycling different antibiotics can be a helpful tool in the prevention of resistance and subsequent difficulty in treating eye-based MRSA. Vancomycin is said to be a particularly effective medication, especially in higher doses over a shorter space of time; however, it should only be used as an "agent of last resort" for severe infections.
MRSA may often be confused with other conditions
One of the biggest challenges around MRSA is diagnosing it in the first place. The infection can frequently look like other conditions, and this may make confirming that it is MRSA (and treating it urgently) quite tricky.
One condition that MRSA can often be confused with is impetigo, a different skin infection that, like MRSA, counts skin sores as one of its symptoms (per Johns Hopkins Medicine). Also caused by staph bacteria, impetigo is usually seen in younger children, and while it usually doesn't cause long-term issues or scarring, it can pass from person to person very easily, and so should be treated immediately (per the Mayo Clinic).
MRSA can also typically look like an insect or arachnid bite, with spider bites looking quite similar to MRSA lesions. While you're likely to know if a spider has indeed bitten you, if in doubt, consult with a healthcare professional immediately. Cellulitis, a skin infection that creates many of the symptoms of MRSA, can also often be prompted by the bacteria, but could also be the result of an entirely different strain of staph bacteria (per the CDC).
What to do if you have MRSA
Contracting MRSA can be a worrisome experience, and the most important thing to do is to not delay seeking treatment from a doctor. The good news is that while an MRSA infection can become more severe, the majority of the time, the condition will clear up without any long-term issues, per Johns Hopkins Medicine.
When you're being treated, antibiotics are your best friend. "Many MRSA infections can be treated with oral antibiotics, but some require intravenous medications, so make sure you and your doctor check the sensitivities found on laboratory testing," states Johns Hopkins Burn Center director and plastic and reconstructive surgeon Scott Hultman.
Your MRSA infection may also be treated using topical antibiotics, for which a prescription will be required (as these creams will often be way stronger than the kinds you can get yourself at the pharmacy). Post-treatment, your doctor may also want to assess your potential for infecting other people by carrying MRSA on your skin or in your nose. Luckily, if you are, Hultman states that there's no cause for concern — treatments are available to remove the bacteria from your skin.
When you have MRSA, your body may resist treatment
Given that the "R" in "MRSA" literally stands for "resistant" (per the Mayo Clinic), it's perhaps no surprise that this is a bacteria that can be tough to eradicate. In fact, the whole reason that MRSA exists in the first place — and is so difficult to treat with antibiotics — is because of the overuse of antibiotic medications by humans, leading to a greater adaptation of bacteria to avoid typical treatments. This can lead to difficulty in treating the condition, as MRSA strains can frequently adapt to evade antibiotics that previously worked.
Unfortunately, particularly robust strains of MRSA have a greater capacity to continue spreading through your body and cause more severe infections in your organs, blood, and bones. Given MRSA's adaptability, you must follow your doctor's instructions around antibiotics, especially if you're being advised to take them at home. Failing to complete a dose of antibiotics can be one of the worst things you can do, as this can give the MRSA bacteria a chance to adapt and cause more issues before it's eradicated from your system (via Johns Hopkins Medicine).
How you can stop MRSA from spreading
In an ideal world, no one would have to treat MRSA, as people wouldn't contract it in the first place. And while this is currently an unlikely prospect, there are certain steps that everyone can take to stop MRSA from spreading so rapidly.
If you don't currently have MRSA, the main thing to do is to make sure your personal hygiene is on point (per the CDC). Make sure you're washing your hands at regular intervals, only using personal hygiene items that haven't been used by anyone else, and tending to any cuts and abrasions quickly.
If you do have MRSA, though, then you should take your preventive measures up a notch. Seek instructions on how to handle any infected areas of skin from your doctor, and stay well away from others when changing dressings or cleaning wounds. Ensure that any items you come into contact with are clean, especially fabrics (which should be washed using high heat and dried using a tumble dryer). Finally, avoid skin-to-skin contact with others until your infection is completely healed, and adhere to your doctor's advice around medication strictly so that you'll make a full recovery.