What Is Ablation Surgery?
Ablation surgery is a minimally invasive medical procedure in which a specific area of abnormal tissue is destroyed in order to treat a variety of conditions (via the Mayo Clinic). Minimally invasive surgeries tend to use smaller incisions and specialized instruments to perform a procedure. The goal is to minimize the trauma to the body and reduce the recovery time for the patient (via Healthline). This is also achieved by using specialized instruments, such as laparoscopes or robotic devices, to perform the surgery, per the Mayo Clinic. Traditional or general surgery, on the other hand, involves making a larger incision in the body. The procedure may be more invasive and result in larger scars, according to Beaumont Health.
If you're undergoing surgery, it is important to discuss your options with a healthcare team. The potential benefits and risks of ablation surgery should be carefully considered before deciding whether it is an appropriate treatment.
Types of ablation surgery
There are several different types of ablation surgery, each of which uses different methods to destroy targeted tissue. Radiofrequency ablation (RFA) is a type of ablation surgery that uses high-frequency radio waves to heat and destroy abnormal tissue, per the Cleveland Clinic. RFA is commonly used to treat chronic pain like sacroiliac joint pain, as well as to destroy cancerous tumors and abnormal cells in the heart that cause arrhythmias. Laser and microwave ablation are two other types of ablation surgery that use heat to destroy abnormal tissue in lesions, according to a 2015 article published in the journal Hepatoma Research.
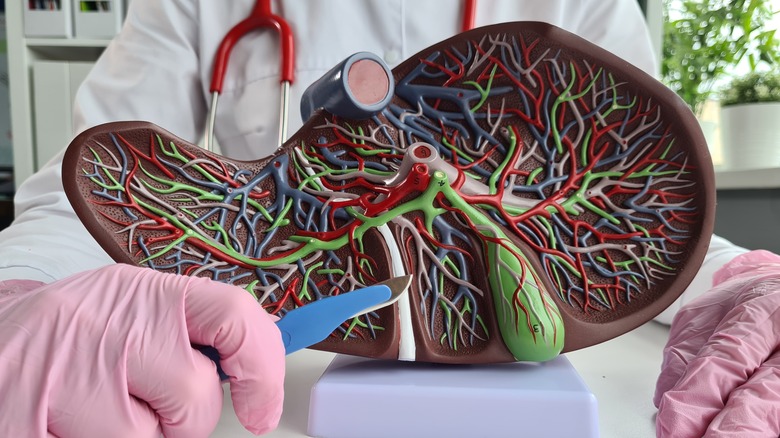
While some surgery types use heat to destroy abnormal tissue, some others, like cryotherapy, also known as cryoablation, use extreme cold, according to MedStar Health. Cryotherapy is commonly used to treat cancerous tumors in the prostate, liver, and kidney. It can also destroy abnormal cells in the heart that cause arrhythmias, per the Cleveland Clinic.
Other common types of ablation surgery include high-intensity focused ultrasound (HIFU) and percutaneous ethanol ablation (PEI). HIFU is a type of ablation surgery that uses high-frequency ultrasound waves to heat and destroy abnormal tissue in the bones and various organs including the kidney and liver, per the Cleveland Clinic. PEI, on the other hand, is a type of ablation surgery that involves injecting ethanol (alcohol) into abnormal tissue. PEI is commonly used to manage thyroid nodules, per a 2014 study published in the Indian Journal of Endocrinology and Metabolism.
Why do people need ablation surgery?
According to a 2014 article published in the journal Techniques in Vascular and Interventional Radiology, ablation surgery is used for destroying tumors that are malignant and benign (non-cancerous) or those that are at risk of becoming cancerous. This includes cancerous tumors in the bones as well as various organs like the liver, kidney, and lungs. In some cases, ablation surgery may be used as an alternative to traditional surgery or as a way to reduce the size of a tumor before surgery, per the source.
Ablation surgery is also used to treat abnormal heart rhythms (arrhythmias) by destroying abnormal scars in the heart that cause the arrhythmia, per the Mayo Clinic. This type of ablation surgery is known as cardiac ablation and is often used to treat atrial fibrillation, a common type of arrhythmia, per the clinic.
Radiofrequency ablation may be used to treat uterine fibroids, which are benign (non-cancerous) tumors that grow in the uterus, says the Cleveland Clinic. Uterine fibroids can cause heavy periods, abdominal pain, and other symptoms.
Other conditions ablation surgery may be used to treat include varicose veins and chronic pain. According to Johns Hopkins Medicine, varicose veins are swollen and twisted veins that are visible just under the surface of the skin, which can cause pain and discomfort and may also increase the risk of developing blood clots. Endovenous thermal ablation uses radiofrequency waves to deactivate the veins, says the Cleveland Clinic. To eliminate chronic pain, ablation therapy destroys the nerve fibers that transmit pain signals, explains Alberta Health Services.
How is ablation surgery performed?
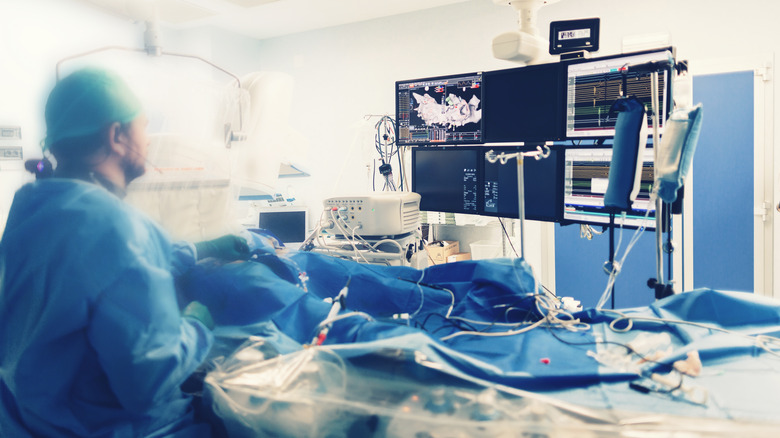
Before the surgical procedure, the healthcare team will carefully plan the ablation therapy and the patient will be given instructions on how to prepare. This may include fasting for a period of time beforehand and avoiding certain medications, says the Cleveland Clinic. Ablation therapy is typically performed with the patient under local or general anesthesia, depending on the type of procedure and the patient's preference. Depending on the location and type of tissue being treated, the surgeon may make a small incision in the skin using a needle and may use a probe or catheter to reach the tissue through the bloodstream. Once the healthcare team has accessed the target tissue, they will use one of several methods to destroy it. These methods may include radiofrequency energy, extreme cold (cryotherapy), laser energy, or microwaves.
During the procedure, the healthcare team will closely monitor the patient's vital signs and the progress of the ablation therapy. They may also use imaging tests (such as ultrasound or X-ray) to guide the procedure and ensure that the entire area of abnormal tissue has been adequately treated, per a 2018 study published in the journal Thoracic Cancer. After the procedure, the patient may experience discomfort at the site of the incision or where the ablation device was inserted and will be given pain medication as needed, says the Cleveland Clinic.
Benefits of ablation surgery
Being minimally invasive, ablation surgery has many benefits. As mentioned earlier, many types of ablation therapy are non-invasive, meaning they do not require general open surgery. This can reduce the risk of complications (via Healthline). Ablation surgery is also a highly targeted treatment, meaning it uses precision to destroy abnormal tissue, leaving healthy tissue intact. The surgery is also effective in treating various conditions, including cancerous tumors, arrhythmias (irregular heartbeats), and uterine fibroids, says Healthline.
Many types of ablation surgery have a quick recovery period, allowing patients to return to their normal activities soon after treatment, says the Cleveland Clinic. For some patients, ablation therapy may be a good alternative to more invasive types of surgery, especially for those who are not candidates for these surgeries due to age or other medical conditions. Ultimately, the decision about which type of surgery to use will depend on the specific needs of the patient and the expertise of the surgeon.
Risks of ablation surgery
While ablation surgery is generally a safe and effective treatment option, there are potential risks and complications that patients should be aware of. The surgery may cause bleeding at the site of the incision or where the ablation device was inserted, according to a 2017 article published in the journal Expert Opinion on Drug Safety. As with all surgeries, there's also a risk of infection after ablation therapy, especially if the procedure was performed through an incision in the skin, says Johns Hopkins Medicine. Symptoms of infection may include fever, swelling, and pain at the procedure site, says the source. Also, after the surgery, there might be pain or discomfort at the site of the procedure, which may be managed with pain medication, explains the Cleveland Clinic. And since the surgery is typically performed with the patient under local or general anesthesia, this carries its own set of potential risks and complications. These may include allergic reactions to the anesthesia, difficulty breathing, and nausea and vomiting, according to Healthline.
It is important to discuss the potential risks and benefits of ablation therapy with a healthcare provider before deciding whether it is an appropriate treatment option. It's also vital to carefully follow the surgeon's instructions for preparing for the procedure and caring for the treated area after the surgery. This can help minimize the risk of complications.