Atrial Fibrillation Explained: Causes, Symptoms, And Treatments
Atrial fibrillation (A-fib) is a common type of arrhythmia or abnormal heart rhythm that affects more than 2 million Americans (via Memorial Hermann). According to the American Heart Association, the heart is in charge of pumping blood to all aspects of the body. The heart's electrical system regulates the frequency of its beats and coordinates the work of its chambers. Arrhythmias can occur when electrical activity is disrupted. When A-fib occurs, the electrical signal normally produced by the sinoatrial node (SA node) begins elsewhere in the atria. As a result, the heart's upper chambers beat quickly and chaotically, causing fibrillation. Because A-fib affects everyone differently, symptoms can range from mild to severe.
Fortunately, numerous treatments are available, ranging from lifestyle changes to surgery. Even if your symptoms are mild or undetectable, it is critical to consult your healthcare provider because A-fib can lead to severe complications, one of which is a five-time increase in the risk of developing a stroke (via Get Smart About Afib). Understanding the risk factors, symptoms, and treatment options can help you manage this common heart condition.
Symptoms of atrial fibrillation
If you're new to A-fib, you might wonder what it feels like. The Centers for Disease Control and Prevention (CDC) mentions that A-fib symptoms vary in severity and presentation, so no two people will have the same feelings or symptoms. In some cases, if the heart rate is not beating rapidly, you may not experience symptoms.
Some symptoms, such as fatigue, shortness of breath, or chest pain, may be ambiguous or mimic other issues. During an A-fib episode, all these symptoms may occur individually or collectively. Additionally, feeling faint or having palpitations that feel like butterflies in the chest is not uncommon (via the Cleveland Clinic).
The American Heart Association (AHA) recommends speaking with your healthcare provider about what you and your family should know about this condition and how to respond to potentially life-threatening symptoms. Understanding the symptoms and disease process can help you live a longer, healthier life. Furthermore, if you live alone, a life-alert device could save your life if you experience worrying symptoms and need assistance.
Coronary artery disease and developing atrial fibrillation
Although coronary artery disease (CAD) and atrial fibrillation are heart conditions, they are vastly different. One condition can be diagnosed even if the other is not present. However, if both conditions coexist, treatment can be complex, and life expectancy may be shortened (via WebMD). According to the World Health Organization, coronary artery disease is the leading cause of death worldwide.
Furthermore, a study published in the American Journal of Physiology states that CAD is a risk factor for A-fib development. CAD is a structural disorder of the heart's blood vessels, as well as a condition in which the vessels narrow due to blockage. As a result, blood flow to the heart is reduced, damaging the electrical system over time and causing A-fib or other arrhythmias. Consequently, most patients have both CAD and A-fib. This is primarily due to shared risk factors such as diabetes, high blood pressure, obesity, stress, and sleep apnea.
High blood pressure can cause atrial fibrillation
When the heart beats, it generates pressure, pushing blood throughout the body and to all of its vital organs. According to the American Heart Association, blood pressure is measured by the heart pumping blood to the body, known as systolic pressure. When the heart is at rest, blood circulates from the body to the heart, known as diastolic pressure. When your blood pressure is checked at home or in a doctor's office, these two pressures combine to form a blood pressure reading. When you have high blood pressure, the blood flows through your vessels with more force than usual.
A study published in the European Journal of Preventive Cardiology concluded that high blood pressure is one of the most common cardiovascular risk factors for developing A-fib. The study also found that maintaining normal blood pressure is a valuable strategy for preventing A-fib and reducing complications caused by cardiovascular diseases.
Furthermore, Kardia states that high blood pressure erodes the artery walls over time. As a result, the heart muscle works harder, becoming stiffer and thicker, which can cause electrical activity to malfunction. And so, A-fib becomes a complication exacerbated by this scenario.
Finally, you must consult your doctor about high blood pressure treatments before it becomes a chronic issue. If detected early on, there may be lifestyle changes that can be implemented to reduce your risk of long-term illness.
Illicit drugs, alcohol abuse, and stimulants can cause atrial fibrillation
People who abuse methamphetamines, cocaine, marijuana, and opiates have an alarmingly high rate of A-fib, according to the American Heart Association (AHA). Chronic drug use increases the risk of developing A-fib up to 86%, with methamphetamines posing the most significant threat. Additionally, Dr. Muhammad Afzal, cardiac electrophysiologist at The Ohio State University Wexner Medical Center in Columbus, reported to Healthline that illicit drugs could alter the autonomic nervous system responsible for controlling the heartbeat. This is one of the main reasons these drugs cause A-fib.
Furthermore, a published study reveals that the particulate matter in marijuana, like cigarette smoke, may increase the risk of developing this arrhythmia. Even though the risk may be lower than other drugs, it is something to be aware of, and further studies are needed.
Aside from illicit drug abuse, the University of California, San Francisco, reported to the AHA that alcohol abuse increases the likelihood of developing A-fib and increases emergency room visits for people with A-fib who abuse alcohol.
Harvard Health also found binge drinking to be an instigator of new-onset A-fib. So much so that it has earned the moniker "holiday heart" because people tend to drink more during the holiday season, resulting in more doctor visits.
Certain cold medicines can cause a flare-up of atrial fibrillation symptoms
Cold and flu medications sold over the counter can aggravate the symptoms of atrial fibrillation. According to the Mayo Clinic, it is critical to be aware of decongestants' ability to raise blood pressure.
If you already have high blood pressure, this can be even more concerning because high blood pressure can aggravate atrial fibrillation and may reduce the effectiveness of any heart medication you may be taking to treat the arrhythmia (via Heart Rhythm Consultants).
Additionally, WebMD mentions that many cold and allergy medications, such as pseudoephedrine, contain a stimulant that increases heart rate. This can be a severe side effect if you have A-fib. Most over-the-counter medications with a "D" after the drug name should be avoided unless you consult your healthcare provider before taking them for symptom relief.
Finally, A-fib patients should carefully read the labels of any over-the-counter cold medicine. Most will include a warning for patients with heart disease. Your healthcare provider can recommend the best medication for your symptoms, ensuring that there are limited side effects and no interactions with your heart medications (via the Mayo Clinic).
Congenital heart defects can increase the risk of developing atrial fibrillation
Patients with congenital heart disease are living longer lives thanks to medical advances. However, medical advances and increased life expectancy bring comorbidities that must be managed, as patients with structural or functional abnormalities are more prone to abnormal heart rhythms, according to the American Heart Association (AHA).
According to a study published in the Journal of Atrial Fibrillation, congenital heart defects affect about nine out of every 1,000 births, with more than 90% of patients surviving into adulthood. These advancements are exciting and provide hope to families with members affected by congenital anomalies. Many congenital heart patients, however, will develop atrial fibrillation at some point in their lives due to surgical interventions, scar tissue formation, or other long-term effects of surgery. The type of congenital defect primarily determines the severity and extent of A-fib development.
Furthermore, another study found that 25% of adult hospital admissions with a history of congenital heart disease were for heart arrhythmia management. A-fib arrhythmias were diagnosed in 86% of this population.
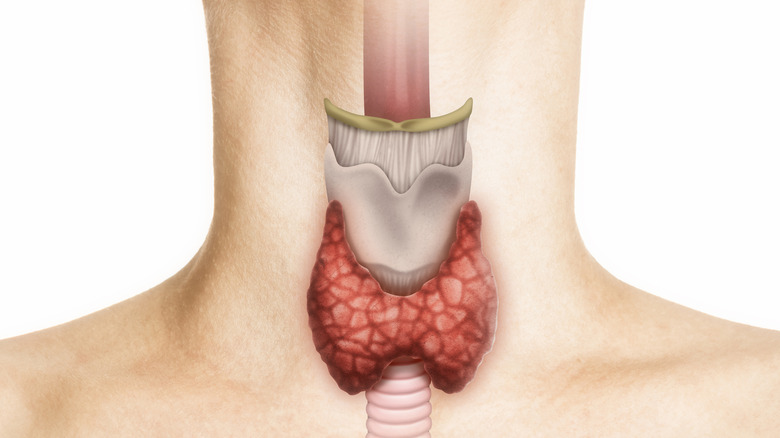
Thyroid disease and atrial fibrillation
When functioning normally, the thyroid gland produces hormones. Most do not notice this gland when all is working correctly (via WebMD). On the contrary, if your thyroid goes into overdrive and produces too many hormones, many bodily functions, including your heart rate, accelerate. If left undiagnosed and untreated, rapid heart rates and arrhythmias such as atrial fibrillation can develop, potentially reducing life expectancy and quality of life. According to a study published in the Journal of the American Medical Association, thyroid disease, particularly hyperthyroid or overactive thyroid disease, has been linked to worsening the health of those with pre-existing heart disease.
It is also worth noting that this study found that up to 60% of hyperthyroid patients developed atrial fibrillation. The American Thyroid Association also notes that when there is an increase in thyroid hormone, the heart rate increases, and palpitations can occur, leading to arrhythmias, including a-fib. Therefore, it is crucial if you have A-fib or heart disease and develop a thyroid condition, you discuss a treatment plan with your healthcare provider.
Rheumatic fever can cause atrial fibrillation years after illness
Rheumatic fever is a complicated disease that can arise from an untreated strep infection, such as strep throat or scarlet fever. This infection is caused by the bacterium group A streptococcus, according to the Centers for Disease Control and Prevention (CDC). Rheumatic fever does not appear immediately; it can take up to five weeks after infection to exhibit symptoms of rheumatic fever. Because of access to health care, rheumatic fever is uncommon in developed countries.
According to Heart and Stroke, heart disease is a complication that can occur after a bout of rheumatic fever. Surprisingly, heart disease may not appear for many years after rheumatic fever. Because rheumatic fever causes inflammation of connective tissue in the body, the heart can be damaged, causing various problems, one of which is atrial fibrillation. When the heart valves are affected by this disease, atrial fibrillation can occur as the valves become more damaged over time. The best way to avoid complications is to see your doctor whenever you suspect an infection is present or is not improving, so that appropriate treatment can be started right away.
Diabetes increases the likelihood of developing atrial fibrillation and can exacerbate symptoms
Diabetes is a chronic condition where the blood sugar level in the body is higher than average. According to the Centers for Disease Control and Prevention (CDC), 37.3 million people in the United States have diabetes. Without proper blood sugar control and lifestyle changes, over time, diabetes can cause significant health conditions that affect many body organs, including the heart.
Furthermore, WebMD mentions people with type 2 diabetes are 40% more likely to develop atrial fibrillation. This is thought to be because diabetes has risk factors similar to heart disease risk factors, such as A-fib. Elevated BMI, which includes obesity, high cholesterol, and hypertension, are examples of these risk factors. Furthermore, uncontrolled diabetes can cause inflammation in the blood vessel lining, which is thought to affect the electrical activity in the heart, resulting in A-fib.
Finally, diabetes can aggravate A-fib if you already have it and make you more symptomatic than someone with atrial fibrillation alone (via Healthgrades).
Atrial fibrillation increases your risk of developing a stroke
When you have atrial fibrillation, your heart does not beat in a rhythmic pattern. Consequently, blood normally pushed through the heart can accumulate in the lower chambers and form clots when this occurs. As a result, when blood clots make their way out of the heart and into the vascular system, they have a high risk of forming in various blood vessels throughout the body, including the brain and lungs (via WebMD).
According to the National Institute of Neurological Disorders and Stroke, one serious complication happens when the blood clot travels to the arteries in the brain and blocks blood flow to a portion of the brain. A stroke is imminent in this situation. People with atrial fibrillation are at four to six times increased risk of developing a stroke during their lifetime. The risk of development increases with age. Even though that may be a scary statistic, treatment with blood thinners can decrease your chances of stroke by up to half.
Chronic snoring can cause atrial fibrillation
You may have a friend or loved one who snores frequently, but did you know that snoring can be a sign of something more serious, such as sleep apnea? The American Academy of Sleep Medicine estimates that 25 million Americans are affected by sleep apnea. Furthermore, it is estimated that more than half of patients with atrial fibrillation also have sleep apnea. To add to these astounding statistics, sleep apnea patients have a four-time higher risk of developing A-fib (via WebMD). If left untreated, sleep apnea can develop ailments such as high blood pressure and diabetes. These comorbidities raise the risk of developing A-fib.
Similarly, because sleep apnea causes breathing to fluctuate from decreased to paused, the risks for A-fib and other arrhythmias are increased due to the decrease in oxygenation during this time. Additionally, the Heart Rhythm Society mentions the stress the heart goes through during sleep apnea episodes can produce chemical changes when the lack of oxygen initiates the startle reflex, according to WebMD. The stress can contribute to arrhythmias, specifically, A-fib.
You are more likely to develop atrial fibrillation if you smoke
According to a European Society of Cardiology study, the more you smoke, the more likely you are to develop A-fib. The study found that for every 10 cigarettes smoked per day, there was a 14% increased risk of developing A-fib, with the risk increasing as the number of cigarettes smoked increased. Furthermore, smokers have a 32% higher risk of developing A-fib than nonsmokers. Fortunately, the study also reveals that the likelihood of developing this arrhythmia decreases as one quits smoking. However, it is unclear if the risk reduces completely, like a nonsmoker.
Additionally, smoking has a toxic effect on the heart, which can cause atria stiffening. When this occurs, the electrical activity is disrupted, increasing the likelihood of A-fib (via FixAFib).
If you want to quit smoking, you are not alone. There are numerous health benefits to quitting and multiple health risks if you choose not to quit. The Centers for Disease Control and Prevention (CDC) provides online smoking cessation materials and a toll-free number 1-800-784-8669 for support, which the National Cancer Institute provides.
Atrial fibrillation can be treated in a variety of ways
Following your healthcare provider's treatment plan is critical if you have been diagnosed with A-fib. The Mayo Clinic explains that the goal of treatment is to keep your heart rate under control, prevent blood clots from causing severe health problems, and stabilize your heart rhythm. Additionally, there are numerous treatment options available to control this arrhythmia. Because the cause of A-fib can be due to different disease processes, not all treatment options will work for all patients.
According to the American Heart Association, medication therapy aims to prevent blood clot formation by prescribing blood thinners. Additionally, if your heart rate is elevated, your doctor may prescribe medications to control the rate. After the heart rate is controlled, you may be prescribed medication to regulate the abnormal heart rhythm.
Additionally, Johns Hopkins Medicine suggests cardioversion if you have new-onset atrial fibrillation or have severe symptoms. Cardioversion is a minor sedation procedure in which your heart is shocked back into normal rhythm. Your doctor will review the procedure's advantages and disadvantages before suggesting this option.
Finally, WebMD suggests that catheter ablation be considered. In fact, a recent study published in the New England Journal of Medicine found that, when given as a first treatment, catheter ablation was more effective than medication at reducing the incidence of irregular heartbeat episodes.