Breast Cancer: A Comprehensive Guide
Statistics show that breast cancer is the most common type of cancer worldwide (per Breastcancer.org), making up about 12.5% of new cancer diagnoses across the globe each year. In the United States, roughly 30% of new cancer cases each year are breast cancer cases. The good news is that deaths from breast cancer have declined in recent years, most likely because of early detection and improved treatments.
Breast cancer affects both men and women of every ethnic background and at any stage of life. People with a family history of breast cancer may be at higher risk than others, but many people with no family history go on to develop breast cancer. By understanding factors that may put you at risk — including your genetics and lifestyle, as well as what symptoms you should look for and the types of screening options available to you — you can take steps to reduce your risk of breast cancer and detect it at an earlier stage.
Breast cancer defined
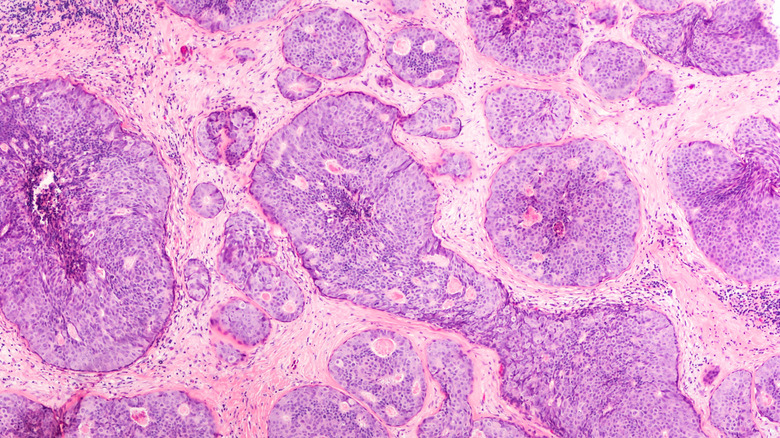
Breast cancer occurs when the cells of certain tissues in the breast increase in size uncontrollably, according to the Centers for Disease Control and Prevention (CDC). Most breast cancers start in either the lobules, which produce breastmilk, or the ducts, which carry milk to the nipple. Breast cancer that begins in the lobules and spreads to other parts of the breast is called invasive lobular carcinoma. Meanwhile, cancer that begins in the ducts and spreads to other breast tissues is called invasive ductal carcinoma. Both can metastasize or spread to other areas to the body.
Some patients develop a condition known as ductal carcinoma in situ (DCIS), which is an early form of cancer. According to Johns Hopkins Medicine, this condition is characterized by cancerous cells in the lining of the milk ducts that do not spread to nearby tissues. Because DCIS does not spread, it responds well to treatment. Patients who choose a lumpectomy (which surgically removes the cancer while preserving the breast) along with radiation have recurrence rates of 5 to 15%. As for patients who choose a mastectomy (surgical removal of the whole breast), recurrence rates are reportedly at a mere 2%.
History of breast cancer
Breast cancer is nothing new. Written accounts of breast cancer date as far back as roughly 3,000 B.C., said to be from the Egyptian physician-architect Imhotep (per a 2014 review in Sultan Qaboos University Medical Journal). In 400 B.C., the Greek physician Hippocrates described the stages of breast cancer. Records show that doctors understood how to surgically remove tumors of the breast in the first century A.D. Over the next several centuries, surgeons across Europe attempted various surgical approaches to remove breast cancer and speculated on its cause.
It was not until the 19th century that German physicians demonstrated that living cells caused breast cancer, and that these cells could spread from the breast through the lymph nodes. In 1894, William S. Halstead, a surgeon at Johns Hopkins, developed radical mastectomy, which become the gold standard for treatment. This procedure removed the entire breast as well as the pectoralis major, a large muscle that lies under the breast. He also demonstrated the importance of removing the tumor intact so as to prevent the spread of cancer cells to nearby tissues. In the late 19th and early 20th centuries, advances led to the use of radiation and chemotherapy to target cancer cells as well as modified radical mastectomy, which left the pectoralis muscle intact.
Since the late 1980's, breast cancer treatments have focused on completely removing breast cancer tissue while preserving as much healthy breast tissue as possible. Patients also have many options for breast reconstruction.
Prevalence of breast cancer in the U.S.A. and worldwide
According to the American Cancer Society, breast cancer is the most common cancer among American women. Worldwide, it is the most common cancer, and is the fifth leading cause of cancer deaths (per a 2021 study in the journal Cancer Communications). Per global estimates from 2020, there are about 2.3 million cases of breast cancer, as well as 685,000 deaths. Breast cancer rates vary from country to country. The incidence and mortality rate of breast cancer is declining in the United States, but increasing in South Korea and China.
The impact of breast cancer is not the same in every country. In general, highly developed countries like the United States, Australia, and the United Kingdom have higher rates of breast cancer than less developed countries such as Costa Rica, Mexico, and Iran. Breast cancer statistics also differ across racial and ethnic groups. Recent data from the CDC shows that the incidence of breast cancer increased among women of non-Hispanic Asian or Pacific Island descent, but decreased among non-Hispanic white women. According to the National Cancer Institute, Black women in the United States are more likely than white women to die of breast cancer, even though they have similar rates of the disease.
Symptoms of breast cancer
Early detection of breast cancer leads to earlier treatment, which can translate to better clinical outcomes. Women should be aware of the symptoms of breast cancer so they can seek prompt medical attention as soon as they develop any.
According to the Mayo Clinic, some of the symptoms of breast cancer affect the breast tissue, while others appear in the skin. Any changes in the size, shape, or appearance of the breast may indicate breast cancer, as can any lumps or thickening of the breast tissue. A newly inverted nipple is also cause for concern. Changes to the skin of the breast (such as dimpling, pitting like the skin of an orange, or redness) are additional symptoms of breast cancer. Lastly, scaling, peeling, crusting, or flaking of the skin of the breast or around the nipple can also be signs of breast cancer.
You may notice changes when you get dressed or conduct a monthly manual exam of your breasts, or your partner may notice these changes. Make an appointment if you develop any of these symptoms or if you have any other concerns about your breast health.
Breast cancer causes and risk factors
Researchers continue to investigate the biology behind breast cancer. According to the American Cancer Society, breast cells become cancerous because of mutations, or changes in the genes of breast cells. Sometimes, these mutations are passed down within a family, but inherited changes only account for about 10% of breast cancer cases. Most people simply develop mutations as part of the normal aging process.
There are a few known inherited mutations that greatly increase the risk of breast cancer. Men and women alike inherit two copies of every gene: one from their mother and one from their father. That means that everyone has two copies of genes known as BRCA1 and BRCA2, but some people have a copy with a mutation. Women who inherit a mutated copy of BRCA1 or BRCA2 have a much higher risk of developing breast cancer (per the CDC). Women with a family history of breast cancer may wish to seek genetic testing to see if they carry a mutation. If so, they may choose increased monitoring to detect cancer early or preventative surgeries to reduce their risk.
Researchers are also working to identify other risk factors for breast cancer. Per the World Health Organization (WHO), female gender and age are the biggest risk factors. Other risk factors are hormonal, such as the age of onset of menstruation and the age at first pregnancy. Other factors relate to lifestyle choices, such as obesity, alcohol consumption, and tobacco exposure.
Diagnosing breast cancer
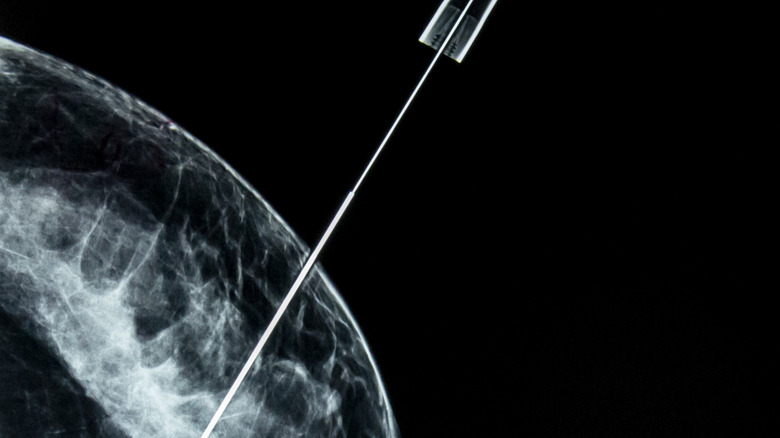
Doctors encourage women to conduct a monthly manual breast self-exam, and they will also perform one at your annual checkup. With this exam, you or your doctor are looking for lumps or anything unusual in your breast tissue and in the lymph nodes in your armpit (per the Mayo Clinic). Doctors also recommend getting an annual mammogram, which is an X-ray image of the breast, to screen for breast cancer.
Mammograms and manual exams are good screening tools, but are not used to diagnose breast cancer. If these exams detect anything unusual, your doctor will recommend further testing. These tests may include a diagnostic mammogram, an ultrasound, or magnetic resonance image (MRI) of your breast. All three tests produce detailed images of your breast tissue. A diagnostic mammogram uses X-rays, an ultrasound uses sound waves, and an MRI uses a magnet and radio waves. One advantage of an ultrasound is that it can show whether a lump in your breast is solid or simply a fluid-filled cyst.
The only way to truly diagnose breast cancer is with a biopsy of the suspicious tissue. If your diagnostic mammogram, ultrasound, or MRI suggests cancer, your doctor will use a needle to extract tissue from the site. Experts will analyze the sample to determine if it is cancerous. If so, they will determine the type of cells that are cancerous, how aggressive they are, and if they have any special characteristics, such as hormone receptors, that can affect your treatment.
Breast cancer treatments
There are many treatment options available to breast cancer patients, and according to Yale Medicine, the best approach is not one-size-fits-all. Treatment for each patient should be based on the type of cancer, which refers to characteristics of the cancer cells, as well as the stage, which refers to how far it has spread in the body.
Some breast cancer cells have receptors for the hormones estrogen and progesterone. These cancers are called hormone receptor (HR)-positive. Other breast cancers have receptors for human epidermal growth factor, and are called HER2-postive. Cancer cells with none of these receptors are known as triple-negative. Patients with HR-positive breast cancers respond well to hormone therapy alone, and may not need chemotherapy. Patients with HER2-positive breast cancers often respond well to a limited course of chemotherapy, while patients with triple-negative breast cancer typically require intense chemotherapy.
Other treatment options include surgery and radiation. According to the American Cancer Society, most patients with breast cancer require some type of surgery. Surgical options include lumpectomy (which removes the cancerous tissue and some tissue around it), mastectomy (which removes the whole breast, as well as some nearby tissue), and the removal of lymph nodes. Your team will help you determine which option makes the most sense for you.
Per the Mayo Clinic, some patients need radiation therapy after surgery to destroy any lingering cancer cells, reduce the risk of recurrence, or treat cancer that has spread to other parts of the body.
Ongoing research and treatment efforts
Decades of research into detection and treatment of breast cancer have made great strides in clinical outcomes and survivorship. According to the WHO, the five-year survival rate for breast cancer patients in high-income countries has surpassed 90%. While this news is certainly encouraging to newly diagnosed patients in these countries, it is less exciting for patients elsewhere. Survival rates are as low as 40% in middle- and low-income countries. These statistics highlight the need for continued research into new treatments, as well as the need for expanded access to screenings and treatments worldwide.
To increase access to care, the WHO has established the Global Breast Cancer Initiative, which is based on three pillars: health promotion and early detection, timely diagnosis, and comprehensive breast cancer management (per a 2021 review in The Lancet Oncology). The goal of this initiative is to reduce breast cancer mortality by 2.5% each year, potentially saving 2.5 million lives over the course of two decades.
Other organizations are working on new treatments. For example, the Vera Bradley Foundation for Breast Cancer funded research into minimizing the side effects of chemotherapy. One class of chemotherapy drugs used to treat breast cancer (anthracyclines) also cause severe and "often irreversible" heart damage. Recent findings identified a genetic variant that may put patients at greater risk for heart damage. The same research discovered that a drug already used to prevent allergic reactions and nausea may minimize the negative effect of anthracycline on the heart.
Breast cancer in men
When people think of breast cancer, they tend to think of women, but men can develop breast cancer, too. According to the CDC, just 1% of breast cancer cases affect men. While men do not undergo routine screenings like women do, they should keep an eye out for symptoms of breast cancer. Many of these symptoms are the same as symptoms women look for, such as a breast lump, swelling, or red, flaky, or dimpled breast skin. Other symptoms include nipple discharge and pain in the nipple area.
Major campaigns have led to greater breast cancer awareness for women, but awareness of breast cancer in men is much more limited. For many men, breast cancer is simply not on their radar. They do not know about the symptoms and they never think to look for them. As a result, men tend to be diagnosed with breast cancer when it is at a more advanced — and less treatable — stage (per Yale Medicine).
Men should be aware of factors that put them at greater risk of breast cancer. Age, family history, and known mutations like the BRCA mutations increase the risk, as do liver disease, Klinefelter syndrome, and having one or more undescended testicles. Other risk factors include previous radiation treatment to the chest, estrogen treatment for prostate cancer, obesity, enlarged breasts, alcohol consumption, and lack of exercise.
Breast cancer prevention
Some people have a greater risk of breast cancer from birth based on their family history and underlying genetic factors. But just because you are at greater risk does not mean you will definitely develop breast cancer. You can take steps to prevent breast cancer and detect it early when it is most treatable.
You can lower your risk by maintaining a healthy weight, staying physically active, and avoiding alcohol or drinking in moderation (per the CDC). Breastfeeding your children also reduces your risk of cancer. Certain hormonal drugs, including hormone replacement therapy and oral birth control pills, may increase your risk, so talk to your doctor about the pros and cons before starting these medications.
If you are already at high risk of breast cancer, you may choose to use medication to reduce your risk (per the American Cancer Society). Drugs like tamoxifen, raloxifene, anastrozole, and exemestane can reduce your risk, but may also cause side effects. Women with a high risk based on family history or positive results for a BRCA mutation may choose a preventative mastectomy (per the Mayo Clinic). Your doctor can help you determine if any of these options make sense for you.
If you have already been diagnosed with breast cancer, your diet may help you survive. New research indicates that breast cancer survivors who ate the largest amounts of cruciferous vegetables (e.g., broccoli, cauliflower, Brussel sprouts, and cabbage) had a lower risk of dying, per Science Daily.
Looking forward: newest findings
New technologies and their applications are advancing breast cancer treatment, promising news for patients everywhere. A 2022 study published in the journal Advanced Functional Materials demonstrated the potential for 3D bioprinted tumor models to test cancer treatments. Bioprinting is like a biological version of 3D printing. Instead of using layers of plastic to create a three-dimensional model, bioprinting uses layers of cells to create a three-dimensional model of a tumor. Researchers used this technique to create a breast tumor model, then treated it with the chemotherapy drug doxorubicin as well as an immunotherapy treatment. This modeling approach may give researchers another way to test new drugs. It may also pave the way for personalized medicine, as researchers could model a patient's specific tumor, then test treatments to see what works best.
Other research focuses on inhibiting breast cancer metastasis, which is the spread of cancer beyond the breast tissue. Roughly 90% of breast cancer deaths are due to metastasis (per News Medical Life Sciences), so preventing metastasis is critical in increasing survivorship. Israeli researchers found that breast cancer cells rely on invadopodia, foot-like projections, to "degrade underlying tissue, enter the bloodstream and [metastasize]." Breast cancer cells need two proteins, Pyk2 and cortactin, to form invadopodia. Blocking these proteins largely blocks metastasis, suggesting a potential target for drug treatments. Developments like this have led to improved breast cancer outcomes: Breast cancer survivorship has doubled since 2007 (via Science Daily).