Nail Fungus: Causes, Symptoms, Treatments, And Prevention
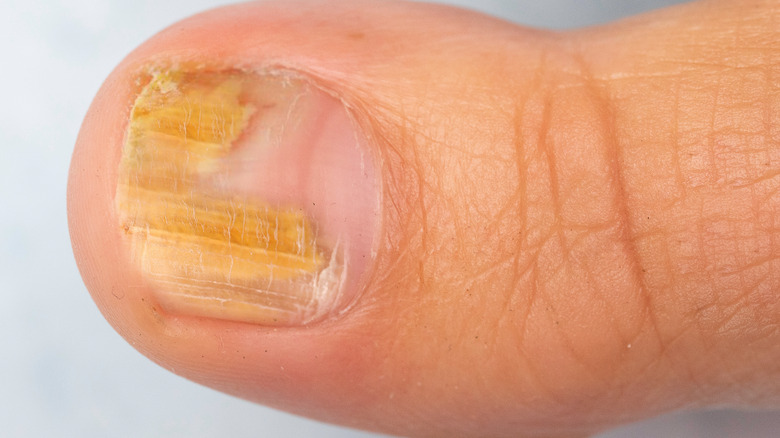
Nail fungus can occur under the tip of the fingernail, but appears more often in the toenail (via the Mayo Clinic). It can cause the nail to thicken or change color to white, yellow, or brown. Fungus-infected nails can also become brittle, crumbly, or ragged. The fungus can spread to other toenails as well as the foot, causing a fungal infection of the foot (athlete's foot). Toenails are often infected when exposed to warm and damp conditions (e.g., sweaty shoes, shower rooms, pools) where fungi flourish.
The medical term for nail fungus is onychomycosis, originating from the Greek words "onyx" and "mykes," which signify nail and fungus, respectively (via a 2020 review of studies published in Inflammation & Allergy Drug Targets). Onychomycosis is responsible for at least half of all nail diseases. Fungi known as dermatophytes cause the vast majority of nail fungus whereas non-dermatophyte molds or, rarely, yeasts (like Candida) account for the remainder. Complications of nail fungus include fungal (e.g., athlete's foot) and bacterial (e.g., cellulitis) infections of the skin.
In general, mild to moderate cases of nail fungus respond to topical over-the-counter antifungals, while oral antifungal medicines are recommended for more severe cases or infection in multiple nails. While some natural remedies (e.g., tee tree oil, natural coniferous resin) and OTC cough suppressant medications exhibit antifungal activity in laboratory experiments, evidence of efficacy from clinical trials is weak (via a 2016 clinical review published in the journal Cutis).
Prevalence of nail fungus
The prevalence of nail fungus in the global population is around 5.5%, and on the rise (per the review of studies published in a 2020 edition of Inflammation & Allergy Drug Targets). The increasing incidence may be due, in part, to increased longevity and more people living in urban areas.
Other contributing factors are the rising prevalence of obesity and greater use of closed-toe footwear (like tennis shoes and boots) that create a warm and sweaty environment for the toes. The prevalence of nail fungus significantly increases with age, occurring in only about 0.4% of children and up to 35% in the elderly (over 65 years old). While toenail fungus occurs more frequently in males, fungal infections of the fingernail — primarily caused by the yeast Candida albicans — is more prevalent in females. In North America and Europe, the prevalence of nail fungus in hospitalized patients is about twice as high as the prevalence in the general population.
Causes of nail fungus
Onychomycosis is caused by the invasion of the toenail or fingernail by fungi that multiply and proliferate, reports Healthline. Since fungi prefer the warm, moist conditions within shoes, toenails are infected more frequently than fingernails. These fungi are often living innocently on the body and, when predisposed, can not only infect the nails but the feet (athlete's foot), groin (jock itch), and skin (ringworm) as well. Nail fungus can be spread from person to person.
Nails are very susceptible to fungal infections because they are constantly exposed to a harsh environment that can often cause structural damage to the nail (via a 2012 review article in the Indian Journal of Dermatology, Venereology, and Leprology). Damage to the nail, in turn, increases the risk of fungal infections. Moreover, nails are shut off from the body's cell-mediated immunity, which protects the body against invading germs. Around 68% of fungal nail infections are caused by fungi called dermatophytes. The most common species of dermatophytes that infects over half of nail fungus cases is Trichophyton rubrum.
Far behind dermatophytes in prevalence are yeasts (11%) and non-dermatophyte molds (11%). Yeasts, primarily Candida albicans, usually infect previously damaged nails or nails of people who have immunodeficiency disorders. Aspergillus and Scopulariopsis are the most prevalent species of non-dermatophyte molds.
Risk factors for nail fungus
Certain risk factors increase the likelihood of developing nail fungus, reports MedlinePlus. In addition to the factors mentioned above, nail fungus can occur as a result of other nail issues. For example, the risk of a fungal nail infection is increased when nails are Injured, deformed, or diseased. Skin conditions such as prolonged moist skin or minor skin injuries can also encourage the growth of nail fungus.
Other factors that make people more prone to nail fungus include smoking, excessive sweating, exercise, fungal infections on other parts of the body, a history of nail fungus, and living with family members who have a fungal infection (via a 2020 review article in Inflammation & Allergy Drug Targets). A number of disorders also predispose a person to nail fungus, including diabetes mellitus, psoriasis, peripheral vascular disease, venous insufficiency, acquired immune deficiency syndrome (AIDS), Down syndrome, bunions, and a toenail abnormality called "asymmetric gait nail unit syndrome (AGNUS)." AGNUS is characterized by toenail changes that resemble nail fungus but without the fungus (via a 2014 study published in the journal Skinmed). The condition develops when uneven flat feet affect walking gait, resulting in toenail trauma from unbalanced shoe pressure.
Types of nail fungus
According to a review article published in a 2012 edition of the Indian Journal of Dermatology, Venereology, and Leprology, the most prevalent type of nail fungus is known as distal lateral subungual onychomycosis (DLSOM). Though this type of nail fungus can infect fingernails, it more often infects toenails. After it first attacks the keratin protein in the thick layer of skin under the free edge of the nail, the fungus then migrates to the nail plate where it causes inflammation, thickening, and separation of the nail from the nail bed.
Superficial white onychomycosis (SWOM) is a fairly rare variant in which the entire nail surface may be covered by white patches. It mainly occurs on toenails. Similar to SWOM, proximal white subungual onychomycosis (PWSOM) is also marked by white spots but occurs in both toenails and fingernails. This variant can spread systemically through the lymphatic system, primarily in people with a weakened immune system, like HIV-infected individuals.
Nail fungus caused by Candida yeasts predominantly affects the fingernails, per Healthline. The yeasts infect the cuticle (the layer of clear skin at the base of the nail), causing redness, swelling and inflammation. The nail may fall off entirely. Previous injury or infection of the nail, as well as frequent soaking in water, predispose nails to Candida infection.
Symptoms of nail fungus
Nail fungus features a variety of different changes to the nail. Initially, a portion of the nail may change to another color such as white, yellow, or brown. Eventually, the entire nail may change color if not treated. While some nails thicken, others thin and become soft, dry, and powdery. Sometimes the nail splits or crumbles or becomes unattached and lifts up from the nail bed. Debris may accumulate underneath the nail.
Some people with nail fungus may experience pain in the toes or fingertips. In others, the nail may reek of a foul odor. A type of itchy skin eruption called a dermatophytid reaction may occur some individuals. These dermatophytid reactions are allergic reactions to the fungus that appear on a part of the body distant from where the fungal (dermatophyte) infection occurs. These eruptions may manifest as small spots filled with fluid, usually on the hands or feet; red welts (hives); solid bumps; or pinkish red spots that look like targets. Once the nail fungus infection is cleared, the dermatophytid reaction disappears.
How is nail fungus diagnosed?
The diagnosis of nail fungus begins with a thorough medical history and physical examination (via Onychomycosis). The history should include previous treatments, hepatitis, skin conditions (e.g., psoriasis, jock itch, or ringworm), alcohol usage, and recreational activities.
A list of current medications is also important, in order to avoid possible interactions with oral antifungal drugs. Examination of the skin should feature the hands, feet, and scalp. While doctors can often make a diagnosis based solely on appearance (one or more thickened, discolored toenails), nearly half of cases of odd-looking toenails do not involve fungi. To confirm a diagnosis of toenail fungus, a type of hand-held microscope called a dermatoscope may be used to analyze a sample of nail debris. In addition, a scraping of nail debris may be cultured to determine the specific fungal species causing the infection. However, results of fungal cultures may take weeks since fungi grow slowly.
Another diagnostic test known as PCR (polymerase chain reaction) is 20% more efficient at detecting fungi species than fungal cultures per se. The PCR test can quickly and accurately identify a pathogen (e.g., fungus) by making billions of copies of its genetic material (DNA or RNA) from a small sample of the fungus (per MedlinePlus).
Medical treatment of nail fungus
Treating toenail fungus is challenging as it may take several months to completely snuff it out, reports the Cleveland Clinic. Even then, the fungus frequently turns up again. Many cases of toenail fungus are mild and without symptoms, thus not needing treatment. The most effective treatments are prescription oral antifungal medications that are taken daily for several months or longer, like Lamisil (terbinafine), Sporanox (itraconazole), and Diflucan (fluconazole).
Blood testing may be advised to monitor potential adverse effects such as liver toxicity and serious drug interactions. Various topical antifungals applied directly to the nail are preferred by people who wish to avoid taking drugs. However, topical medicines used as a complement to oral medications enhance the overall treatment outcome. For example, a medicated nail polish (ciclopirox, or Penlac) can be painted on the nails daily and then wiped off with alcohol after a week of accumulation (via the Mayo Clinic). The process is then repeated for up to a year. Prescription antifungal creams such as efinaconazole (Jublia) or tavaborole (Kerydin) may also be used, preferably after first thinning the nails to allow for better penetration to reach the fungus.
Another option is laser treatment whereby a device shines a high-tech laser beam into the toenail to kill the fungus. While FDA-approved to treat nail fungus, lasers are less effective than oral and topical medications. Nail debridement is also an option, particularly for cases that are resistant to treatment (via Medical News Today). Debridement may involve the periodic reduction of the thickness of the nails or non-surgical chemical nail removal.
Natural remedies for nail fungus
Traditional treatments for nail fungus take a long time, are not always effective, can be expensive and come with potential systemic adverse effects (via a clinical review in Cutis). Fortunately, several natural and over-the-counter remedies hold promise as viable and safe alternative therapies for nail fungus. For example, tee tree oil has a long history of medicinal use, including the treatment of fungal conditions like athlete's foot. Among various fungi, tee tree oil was effective at inhibiting the growth of Trichophyton rubrum, the most common cause of nail fungus. Topical OTC cough suppressants (particularly those containing camphor, menthol, thymol, and eucalyptus oil) have also been shown to have antifungal activity against T. rubrum. Thymol, in particular, works by damaging the cell membranes and inhibiting the germination of the fungi.
Another potential remedy for nail fungus is natural coniferous resin (NCR) extracted from the Norway spruce tree (Picea abies). NCR has been demonstrated via cell culture experiments to kill a wide variety of pathogens including the Trichophyton species of fungi and Candida albicans. Antifungal properties have also been attributed to an extract of the plant species Ageratina pichinchensis (used traditionally in Mexico as a remedy for skin fungus), as well as ozonized sunflower oil. Ozonized sunflower oil is made by reacting ozone gas with sunflower oil to form a gel.
Ultimately, while these natural and OTC remedies have efficacy, clinical human trials performed with these agents were too small, lacked adequate controls, and used different testing methods. Larger randomized clinical trials are essential to prove efficacy.
Complications of nail fungus
Nail fungus can spread to other nails and the skin, potentially leading to fungal skin conditions such as athlete's foot, jock itch, or ringworm (per a 2020 review article in Inflammation & Allergy Drug Targets). People with nail fungus also run a higher risk of cellulitis (skin infection), paronychia (infection of the skin around a nail), or other bacterial infections. This risk is particularly high in individuals who have weakened immune systems, including those with diabetes. In cases of severe nail fungus, daily activities and nail function may become challenging. Some people may even struggle with standing and walking.
Untreated nail fungus can cause pain and discomfort as well as paresthesia (numbness or a tingling sensation in the extremities). Nail deformities such as rounded or curved nails may also develop. Trimming nails and fitting into shoes may become difficult. Females, in particular, may have low self-esteem due to social embarrassment from disfigured nails. As a result, quality of life may be impacted. Other complications of nail fungus include a re-emergence of the infection, permanent loss of the infected nail, and systemic spreading of the infection into the bloodstream (via Healthline).
Liver damage is a potential complication of continuous antifungal drug therapy (via Onychomycosis). This can be minimized with an alternative approach known as pulsed systemic therapy. For example, a dosage of Lamisil can be taken every day for one week every nine weeks for three cycles, or pulses.
Prevention of nail fungus
Several measures can be taken to help prevent fungal nail infections (via the Cleveland Clinic). Risk of toenail infections can be minimized by wearing flip-flops, sandals, or other footwear instead of going barefoot in public swimming pools, showers, and changing rooms. Since fungi grow well in damp conditions, feet should be dried thoroughly after showering and kept dry. Shoes should not be too tight or too loose, especially around the toes.
Practicing good nail hygiene should also be a priority. Nails should be kept trimmed and cut straight across. This helps prevent germs form fungi from getting under your nails. Softening and moisturizing your nails before cutting them is recommended. Thus, the best time to cut your nails is after a shower or bath, or after soaking them in warm water. Aggressive clipping of your nails should be avoided, and trimmers should be disinfected before use.
Additional tips that minimize the risk of nail fungus infection include wearing shoes that "breathe" to allow air and moisture to escape from inside the shoe (per the Mayo Clinic). Old shoes that may be contaminated with fungi should be disinfected or thrown away. Wearing absorbent socks or changing socks daily is also advised. An antifungal foot powder applied to the nails can help discourage fungal infection while a nail hardener can strengthen nails and cuticles. Tools for pedicures or manicures should be sterilized, whether used at home or at a salon.
Prognosis
With prompt treatment that is continued for as long as prescribed, fungal nail infections usually have a good prognosis, notes the American Academy of Dermatology Associates. However, nail fungus can be a persistent foe. While treatment can get rid of the infection, it takes a long time for noticeable improvement in the appearance of the nail. Nails grow slowly — a new, healthy-looking toenail requires up to 18 months to grow out, whereas a fingernail can be replaced in half the time (4 to 6 months).
Overall, fungal infections of the fingernails have a significantly better prognosis than cases of toenail fungus (via Onychomycosis). Moreover, nails that have yellow streaks along the sides of the nail are more resistant to treatment. In any case, even with successful treatment, the fungal infection may return. Anywhere from 5% to 50 % of nail fungus infections reoccur. Thus, compliance with preventive strategies is important for reducing the risk of recurrence.