Ringworm Explained: Causes, Symptoms, And Treatments
Microorganisms such as bacteria, fungi, and viruses are all around us. They can be on the surfaces you touch, the ground you walk on, and the food that you eat. They can even be on your skin or inside your body. Some of them are harmless, while others are harmful only to certain people. But there are also microorganisms that can cause harm to all of us.
Although fictional movies or TV series about infectious diseases such as "Outbreak," "Contagion," or "The Last of Us" are oftentimes exaggerated, they are more true to life than they seem. This concept is further supported by past pandemics that we have experienced including the Black Plague, Spanish Flu, SARS, and very recently, COVID-19. Some of the most worrisome infections that we face are caused by bacteria and viruses, but fungal infections can also be a threat to our health and should not be overlooked. Luckily, according to the Centers for Disease Control and Prevention (CDC), out of the millions of fungal species that exist in the world, only a few hundred of them are harmful to us. Some of them can cause relatively mild allergies, rashes, or skin infections, while others can cause life-threatening brain, blood, or lung infections.
What is ringworm?
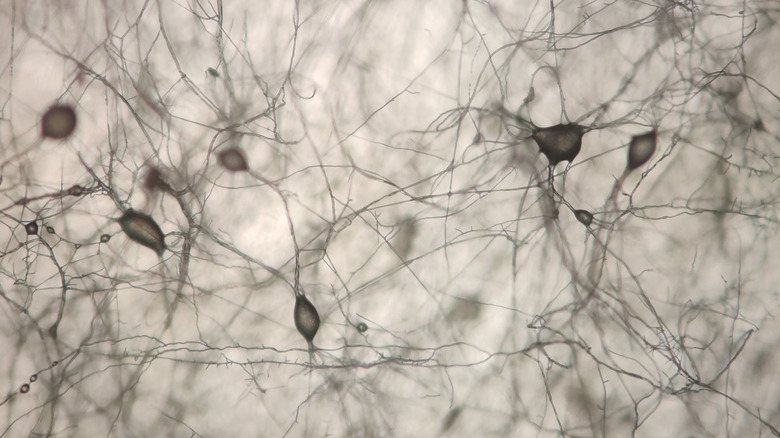
Contrary to its name, ringworm is not caused by worms. It is the common name used to describe tinea, a superficial skin infection caused by a group of fungi called dermatophytes (per Merck Manual). Dermatophytes are multicellular filamentous molds that look like fine, branching threads (via Microbiology Society). They use keratin found in your skin, hair, and nails to grow and survive. In humans, species of dermatophytes that can cause infection include Epidermophyton, Microsporum, and Trichophyton. Any one of these species can cause a ringworm infection (per Merck Manual).
According to Cleveland Clinic, you can acquire a ringworm infection through direct physical contact. Examples of scenarios where you can get infected include touching an infected person skin-to-skin, coming into contact with contaminated objects or surfaces (e.g., towels, bedding, used gym clothes, or even the floor), walking barefoot on contaminated soil, and petting infected animals such as cats or dogs.
Different types of ringworm
Ringworm infections are classified based on location. They are collectively known as dermatophyte, or tinea, infections. The American Family Physician lists them down as tinea capitis, barbae, faciei, corporis, cruris, manuum, pedis, and unguium.
Tinea capitis is the most common dermatophyte infection seen in children. It affects the scalp and hair shafts and is transmitted via contact with contaminated hats, hair brushes, pillowcases, and other similar objects. It is usually seen in children with poor hygiene and those who are exposed to overcrowded environments. Infected hair strands that fall off the head can carry the culprit fungi for more than a year. Moving down from the scalp to the face, tinea barbae affects the skin and hair where the beard and mustache grow, while tinea faciei affects all other non-bearded areas of the face. Tinea barbae is often seen in men, and in women with hirsutism — a condition that causes excess body hair to grow on areas that do not normally have hair. On the other hand, tinea faciei can sometimes be caused by a tinea capitis infection that spreads downwards (per Osmosis).
Tinea corporis is a dermatophyte infection of the neck, trunk, arms, and legs. Like tinea capitis, tinea corporis is also very common in children (via Tinea Corporis). When a dermatophyte infection is present in the groin area, it is called tinea cruris or, colloquially, "jock itch." It happens when the environment around the groin is hot and humid. A dermatophyte infection of the hands is called tinea manuum, infection of the feet is called tinea pedis (i.e., athlete's foot), and infection of the fingernails or toenails is called tinea unguium (per American Family Physician).
Difference between tinea versicolor and ringworm
Similar to the dermatophyte infections, tinea versicolor (aka pityriasis versicolor) is also caused by a fungus. Specifically, it is caused by Malassezia furfur, a club-shaped yeast that is distinct from the dermatophytes (via DermNet).
According to the University of Texas Health Services, tinea versicolor is commonly seen in those living in places with warm and humid weather. Scaly skin patches of different sizes can appear on the neck, upper back, and shoulders. It is a persistent infection that comes and goes and has a tendency to recur. They may appear lighter than normal skin during the summer (when normal skin tans from sun exposure), and appear darker during the winter (when tanning of the skin during summer progressively fades). Unlike dermatophyte infections, tinea versicolor is not contagious and is mostly a cosmetic issue.
The Mayo Clinic adds that Malassezia furfur is a normal part of healthy skin. It only causes tinea versicolor when it multiplies uncontrollably to greater numbers. This can occur in people with oily skin, those who are exposed to hot and humid weather, those who experience changes in their hormones, and people with compromised immune systems. If you have a history of tinea versicolor, your doctor may prescribe antifungal agents such as selenium sulfide (lotion or shampoo), ketoconazole (cream, gel, or shampoo), itraconazole (tablet, capsule, or oral solution), or fluconazole (tablet or oral solution) during the warm months of the year to prevent it from recurring.
Who is at risk of getting infected with ringworm?
Although ringworm is common in children, the Cleveland Clinic states that it can be seen in up to a quarter of the world's population at any given point in time. It is extremely common and can affect anyone regardless of their age, gender, race, or ethnicity. However, there are certain groups of people who are more prone to contracting it compared to others. Among these include people living in warm and humid places, people with weak immune systems (e.g., due to HIV, cancer, malnutrition) or autoimmune diseases (e.g., lupus, psoriasis, rheumatoid arthritis), athletes who participate in high-contact sports (e.g., wrestling), people who sweat a lot, people who use public locker rooms and showers, and people who work with or around animals that can get infected with ringworm (e.g., veterinarians). Healthline adds that wearing tight shoes or clothes, being obese or overweight, and having diabetes also increase your risk.
The latest data from the CDC shows that the average number of outpatient visits for ringworm between 2005 to 2014 was close to five million; and in 2014, 690 cases of ringworm resulted in hospitalizations.
Signs and symptoms of ringworm
Ringworm signs and symptoms may vary depending on the type. The American Academy of Dermatology Association (AAD) explains that generally, you may see flat, ring-shaped lesions on the skin — hence, the name "ringworm." They are usually red or pink on light skin and brown or gray on darker skin. They begin as round patches that can grow in size and spread across other areas of the body. Their borders are raised and covered with scales, and they can be extremely itchy. Eventually, the central part of the lesions will clear, causing them to appear like rings. This is particularly true for tinea corporis. Tinea capitis and tinea barbae will present like this as well, but they may also cause hair loss on the affected areas and develop sores with pus.
American Family Physician adds that people with tinea faciei may experience worsened symptoms with sun exposure. While they also develop red patches, the lesions usually do not have raised edges or scales, making them difficult to recognize. Jock itch can be seen in the upper inner thighs and can even spread to the buttocks and lower abdominal area, but the scrotum is often unaffected. Red, scaly patches that itch or sting appear on the affected areas, and can sometimes also develop vesicles and pus-filled lesions. Tinea manuum can appear as dry and thick skin on the palms, while athlete's foot can appear as an itchy or burning rash in between the toes, scaly and thickened skin on the soles and heels, or a red rash with vesicles and pus-filled lesions on the soles of the feet. Lastly, tinea unguium can cause toenails and fingernails to become brittle, discolored, and thickened (via the AAD).
Diagnosis of ringworm
Ringworm is often easily recognizable just by looking at its appearance, which means that your doctor will usually be able to tell if you have ringworm by asking you about your symptoms and examining your lesions visually. However, depending on your medical history and other symptoms you may have, your doctor may decide to do a confirmatory test to be sure.
Initially, if you have ringworm on one specific area in your body, your doctor will also examine the rest of your body to make sure that you do not have signs of infection elsewhere. This is important because ringworm infection is persistent and can easily spread, and if all sources of infection are not treated properly, it will never go away (per the AAD). If your doctor decides to order tests, the most common one is the potassium hydroxide (KOH) test, where a scraping of your skin or clipping of your nail is placed in a KOH solution (which destroys all cells except for fungal cells) and examined under a microscope. It is simple, fast, and can be done at the clinic (via Medical News Today).
According to the CDC, if no fungal cells are seen but your doctor is highly suspicious that it is a tinea infection, they may order other tests such as a fungal culture, stained laboratory examination specifically for tinea of the nails, polymerase chain reaction (PCR), or Wood's lamp exam, where ultraviolet light is used to look for the presence of dermatophytes.
Ringworm treatment options
Since it is a fungal infection, it only makes sense that ringworm can be treated using various oral and topical antifungal medications. WebMD states that there are readily available, over-the-counter (OTC) antifungal creams, lotions, or powders being sold at local pharmacies. Cleveland Clinic adds that if you have tinea capitis, antifungal ketoconazole shampoo such as Nizoral A-D may help control the infection.
Typically, you will want to use topical antifungals for at least two weeks. But if your lesions persist or your symptoms worsen, you may need to take oral medication, which can be prescribed by your doctor. Depending on the type of drug you were prescribed and how severe your infection is, you may need to take antifungals for as short as seven days to as long as 10 weeks (via WebMD).
Alarmingly, the CDC warns that over the past decade, there has been an increasing number of dermatophyte species that are resistant to the antifungals we have today — and this is probably due to overuse or misuse of antifungal drugs, and travel and migration of people who have antimicrobial-resistant dermatophytes.
At-home remedies for ringworm
If you have ringworm, there are several things you can do at home to help ease your symptoms and facilitate a faster recovery.
With or without infection, it is important to practice good hygiene. Keeping affected areas of your body clean helps control the infection and prevent it from spreading to other areas. Healthline recommends washing infected areas with water and antibacterial soap before applying anything on them. It is also equally important to dry your skin well to avoid creating a wet and humid environment that would allow dermatophytes to thrive. Applying cotton balls soaked in apple cider vinegar or tea tree oil three times a day may also help, as both of these substances are known to have antifungal properties. Coconut oil, oregano oil, and lemongrass oil also have antifungal properties. Warmed coconut oil can be applied onto the skin directly, and it can be used on the scalp as well. Oregano oil and lemongrass oil can also be used on the skin, but they are potent and need to be diluted with a carrier oil such as olive or coconut. Turmeric and powdered licorice also have antifungal properties, and can be combined with water to make a paste and applied on the skin.
Aloe vera is a commonly used gel that has antifungal, antibacterial, and antiviral properties (via Medical News Today). It also has a cooling effect when applied on the skin which helps reduce redness, swelling, and itchiness. Applying diluted grapefruit seed extract on affected areas may also help treat ringworm, and applying crushed garlic paste mixed with a carrier oil has been proven to effectively treat fungal infections.
How to protect yourself from ringworm
Because ringworm is a very common and highly contagious infection, it may be difficult to fully prevent yourself from ever getting it. In fact, According to Medical News Today, infectious spores from dermatophytes can survive for as long as 20 months, which means that coming into direct physical contact with contaminated objects within that time frame can lead to an infection.
Despite dermatophytes being persistent little creatures, there are certain things you can do to lower your chances of getting infected by them (per the CDC). These include wearing shoes that are not too tight and allow air movement around your feet; wearing clean underwear and socks daily; practicing good hygiene; keeping your skin dry; using flip flops in public areas like locker rooms and showers rather than going barefoot; keeping your nails short and clean; avoiding sharing clothes, sheets, towels, brushes, and other personal items with infected people; taking a shower immediately after engaging in contact sports; keeping all sports gear and uniforms clean; and washing your hands with soap and water after playing with pets. Make sure that your pets get seen and treated by their veterinarian if they have ringworm, wear gloves when interacting with them, disinfect all surfaces they come into contact with, and vacuum all areas of your home where your pet has been in, since their shed skin flakes and fur can also be a source of infection.
Ringworm and pregnancy
When it comes to being pregnant, you are no longer worried just for yourself, but also for your unborn child. Everything turns into a question mark, and you will often find yourself asking, "is this safe for my baby?"
Although getting ringworm while you are pregnant will not necessarily affect your baby, the Cleveland Clinic advises that you speak with your doctor first before taking or using any medications, especially if they are over-the-counter. This is because not all drugs are safe for use during pregnancy and can even cause harm to you or your baby. According to a 2017 article published in the Indian Dermatology Online Journal, topical antifungals like clotrimazole, terbinafine, ciclopirox, naftifine, and oxiconazole are relatively safe during pregnancy, while econazole, miconazole, ketoconazole, and selenium sulfide should be avoided. Additionally, oral fluconazole, itraconazole, and griseofulvin should also be avoided. If you are breastfeeding, DermNet states that all topical antifungals are relatively safe; but when it comes to oral antifungals, only oral fluconazole and ketoconazole are safe, while oral terbinafine and griseofulvin should not be used.
Ringworm and diabetes
People with diabetes are at an increased risk of getting infected by ringworm. According to Skin Manifestations of Diabetes Mellitus, around 30-70% of people with diabetes will have some form of skin condition or another; and a lot of times, the skin is the first to show evidence of disease. One in every five diabetics will acquire a skin infection, with tinea pedis being the most common dermatophyte infection seen. In healthy individuals, dermatophyte infections are usually easily managed, but in diabetics, it can lead to serious complications like secondary bacterial infections, fungemia (fungal infection of the blood), and sepsis if left untreated.
Ways to prevent contracting ringworm are the same for everyone, regardless of whether you have diabetes or not. But the American Diabetes Association adds that people with diabetes should pay closer attention to their blood sugar levels and ensure that they remain controlled. While extra moisture causes dermatophytes to grow and thrive, having extremely dry skin is also not good, as scratching can cause a break in the skin that allows existing infections to enter the bloodstream. During cold and drier months, moisturizing the skin is advisable, but applying lotion in between the toes should be avoided. The feet should also be regularly checked for cuts or sores, since these are common sources of infection, and diabetics who have neuropathy (nerve damage that impairs mobility and sensation) may be unable to feel injuries to their feet (per the Cleveland Clinic).
Ringworm versus eczema
Ringworm can be confused with other skin conditions. For example, eczema is a long-term inflammatory disease of the skin that causes red, itchy, dry, and scaly patches to form on several areas of the body (per the National Eczema Association). There are many different types of eczema, with nummular eczema being the one that resembles ringworm the most. According to WebMD, nummular (or discoid) eczema appears as coin-shaped lesions following trauma to the skin (e.g., burn, insect bite). In general, eczematous lesions commonly affect the face and scalp in infants; the elbows, back of the knees, neck, wrists, and ankles in children; and the face, behind the knees, wrists, hands, and feet in adults. Similar to ringworm, lesions may appear red in light-skinned individuals. But in people with darker skin, lesions may be lighter or darker than their normal skin tone.
Unlike ringworm, eczema is not contagious, and its underlying cause is unknown. Since eczema is not caused by a fungal infection and is mostly a permanent condition, treatment is focused on reducing symptoms and preventing recurrences. These include treating lesions with topical creams that reduce inflammation or regulate the immune system, taking antihistamines to help relieve itchiness, and taking antibiotics or antifungals only if an infection is present (via MedicineNet).
Ringworm versus psoriasis
Psoriasis is another skin condition that can resemble a ringworm infection. Similar to eczema, it is an immune-mediated inflammatory disease of the skin that can affect many different areas of the body. It is very common and affects more than 7.5 million American adults. Skin lesions can be seen as raised red plaques with scales, commonly seen on the elbows, knees, and scalp. Like ringworm, psoriatic lesions can itch, sting, or burn. They can also affect the nails and cause them to appear thick and pitted (per the National Psoriasis Foundation). Unlike ringworm but similar to eczema, psoriasis is a life-long condition and is not contagious, so treatment of the condition targets symptom management (via Healthline). Its underlying cause is unknown but it also tends to run in families. Unlike eczema, psoriasis can affect the groin area, a condition called inverse psoriasis, which can be mistaken as jock itch (per Medical News Today).
Ringworm versus seborrheic dermatitis
According to the Cleveland Clinic, seborrheic dermatitis is a common skin condition that causes red, itchy, and scaly patches to appear on the skin. It commonly appears on the scalp, but can also be seen on other areas of the body with high oil production such as the upper back, chest, face, behind the ears, and skin creases. It can easily be confused with ringworm because of the appearance and location of its lesions, but seborrheic dermatitis is not contagious and is a long-term condition that comes and goes. It is more commonly known as dandruff or cradle cap when it affects the scalp, and unlike tinea capitis, seborrheic dermatitis does not lead to hair loss. It is thought to be associated with the fungus Malassezia, which is not a dermatophyte, but is the same type of fungus that causes tinea versicolor.
Medical News Today states that unlike ringworm, seborrheic dermatitis can cause the skin to appear greasy with white or yellow crusting. Treatment of seborrheic dermatitis includes OTC dandruff shampoos, prescription medicated shampoos, topical antifungals, steroids, and drugs that control the immune system (via the Cleveland Clinic).