What Really Happens To Your Body If You Get Sun Poisoning
The term "sun poisoning" gets thrown around a lot during summer, but mostly by laypeople, according to family medicine doctor Matthew Goldman, MD (via Cleveland Clinic). That's because it's not actually a formal medical diagnosis. Rather, it's the general term that is understood to refer to any number of clinically diagnosed medical conditions caused by sun overexposure in people who are sensitive to it. As dermatologist Dr. Joshua Zeichner explains, "Sun poisoning is a reaction to a severe sunburn that affects your entire body" (via Allure). Along these lines, some liken sun poisoning to an allergic reaction to the sun's UV rays in those who are sensitive to the sun's UV rays, per Curist.
If all of this sounds a bit abstruse, it's only because sun poisoning does not have one single scientific term or diagnosis associated with it. To wit, if you were to search for "sun poisoning" in the Google Scholar database for any clinical studies on the topic of "sun poisoning," you would come up empty. In fact, the University of Pittsburgh Medical Center defines sun poisoning as, simply, "an extreme sunburn." So do WebMD and Healthline. The Mayo Clinic doesn't even refer to sun poisoning, except to say it's a term sometimes used to refer to a rash caused by sun exposure. We'll be discussing that below, along with the other things that happen to your body which are associated with sun poisoning.
What exactly is sun poisoning?
Sun poisoning does not occur without direct skin exposure to the sun or without sunburn, per GoodRX. Sunburn is defined as "inflamed, painful skin" that occurs in response to sun exposure (via Mayo Clinic). So if your skin has not been exposed to the sun, or if it has but you don't have a sunburn, then you can't have sun poisoning. On the other hand, if you do have a sunburn, it still does not necessarily rise to the level of sun poisoning — regardless of the various health risks you may be taking when you spend too much time in the sun without appropriate skin protection, per the Skin Cancer Foundation.
For a sunburn to be considered sun poisoning, the burn must be "severe," per GoodRX. That could mean blisters on sunburned skin, though you don't have to blister to have sun poisoning. Likewise, you may develop a fever and/or related symptoms, but you don't have to register a fever to have sun poisoning. Moreover, there's no minimum amount of sun exposure that is required before sun poisoning can set in. Sun poisoning can present even after just a few minutes of sun exposure, depending on your sensitivity to the sun's UV rays. Ultimately, sun poisoning may be diagnosed if, in addition to a sunburn, you develop any of the conditions discussed below.
You may develop a prickly rash or hives
A sunburn is not a rash, but a literal burn to the skin, as the name implies (per University of Pittsburgh Medical Center). Unlike most burns, however, sunburn is not caused by heat, but by ultraviolet radiation (UV rays), according to dermatologist Dr. Saira George (via MD Anderson). For that reason, it's possible to develop sun poisoning even in cold weather, as long as you have developed a sunburn on exposed skin. In some people, however, a sunburn may present along with a rash (via the Mayo Clinic).
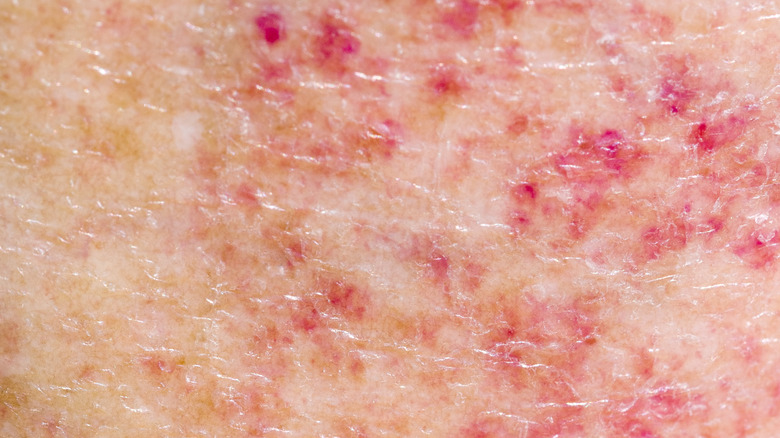
If, in connection with a sunburn, you notice "tiny inflamed bumps or slightly raised patches of the skin," your doctor may give you a diagnosis of "polymorphous light eruption" (PLE), defined as a "rash caused by sun exposure in people who have developed sensitivity to sunlight." PLE is distinct from heat rash, in which perspiration clogs the pores, and which is related to heat (as opposed to UV rays). The Mayo Clinic considers PLE to be synonymous with sun poisoning. So does the Health Department in Campbell County, Wyoming.
However, PLE is just one way sun poisoning may present. Just because your skin doesn't react with PLE to sun exposure, doesn't rule out sun poisoning. On the other hand, a literal sun "allergy" may cause hives in people with a condition known as solar urticaria (per WebMD), but that's not a symptom of sun poisoning.
Your sunburn may sprout blisters a few hours after sun exposure
Although overexposure to the sun isn't a healthy practice, a sunburn in and of itself does not rise to the level of sun poisoning (which itself only rarely rises to the level of alarm that the word "poisoning" might simply). There is one notable exception, however, and that is when your sunburn is more than just a first-degree burn. A first-degree sunburn, like any first-degree burn, comprises damage only to epidermis, the top layer of the skin (per Cleveland Clinic). A first-degree sunburn can be red, moderately painful, and hot to the touch, but while it may correspond to long-term sun damage (per Mayo Clinic), it's not associated with sun poisoning without other symptoms.
The same cannot be said for second-degree sunburns and beyond. A second-degree sunburn is one that reaches the dermis or inner layer of the skin. You'll be able to recognize it as a layperson because it will blister within several hours after sun exposure, per University of California – Davis. While a blistering sunburn is a sunburn, the severity suggests sun poisoning. On rare occasions, a sunburn may affect deeper layers of the skin. When a sunburn is deep enough to damage the skin's nerve endings, it is treated as a third-degree burn. This is very serious, and necessitates immediate medical attention.
Other skin symptoms may be present along with redness, rash, and/or blisters
In addition to the redness and/or blistering of a sunburn, sun poisoning may also involve swelling of the affected skin, hyperpigmentation, and/or severe pain. Even a mild sunburn can feel painful to the touch, but a sunburn that rises to the level of sun poisoning may also involve significant swelling of the reddened or blistered skin and visible swelling. According to Medical News Today, you may even see eczema-like lesions and/or a darkening of the skin that goes beyond simple redness. That said, lesions and hyperpigmentation are more commonly associated with an actual allergy to the sun (as opposed to the metaphorical sun "allergy" that sun poisoning may be said to comprise by both laypeople and medical professionals), per Cleveland Clinic.
Sun allergies include solar urticaria, which WebMD describes as hives that develop in response yo sun exposure, and actinic prurigo, which looks like raised nodules on the skin but will appear on areas of the skin that were not actually exposed to the sun. Actinic prurigo is also known as hydroa aestivale and Hutchinson's summer prurigo (via Cleveland Clinic), and is observed primarily in people of Latin or Native American descent with darker skin tones. Neither solar urticaria nor actinic prurigo is synonymous with sun poisoning, but the presence of either should be a clue of a genetic sun sensitivity which may predispose one to sun poisoning.
You may develop flu symptoms
Sun poisoning doesn't really refer to being poisoned by the sun. It's more of a loosely defined collection of symptoms suggesting that the affected person has spent more time in the sun than their body can handle without developing an inflammatory reaction, per New York City dermatologist Joshua Zeichner (via Allure). Sunburn is an inflammatory reaction to the sun's UV rays, but when a sunburn is severe enough, with or without pain or blistering, it can set off an inflammatory reaction throughout the entire body.
As dermatologist Shari Marchbein put it, "dermatologists don't use [the term sun poisoning] because it's not a real entity." Rather, sun poisoning is a simply a severe sunburn that may be "accompanied by systemic symptoms," including chills. Where there are chills, there is often a fever. Where there is fever, there are often body aches, headaches, dizziness, and nausea, per FastMed. You may also feel exhausted, vomit, and/or faint. Thus, despite sun poisoning not being an "entity," the symptoms can still be serious enough to merit immediate medical attention.
Confusion after sun exposure may indicate a more serious and chronic condition
To say that some people are more susceptible to sun poisoning is something of an understatement, according to dermatologist Jonathan Rees, who authored a 2004 academic paper on the genetics of sun sensitivity in the American Journal of Human Genetics. As Dr. Rees points out, "humans vary [more than] 100-fold in their sensitivity to the harmful effects of ultraviolet radiation." One of the most significant factors affecting one's sun sensitivity is skin pigmentation, with darker skin being associated with less sun sensitivity, in general. However, other factors also come into play, including hair color, with red hair being associated with extreme sun sensitivity. There are also "less-well characterized differences in skin inflammation and repair processes."
In this regard, Rees wasn't talking specifically about illnesses and conditions that might exacerbate skin inflammation, but rather variations within a sub-clinical range. However, a 2001 case study published in Rheumatology suggests that people with the autoimmune condition lupus might be more predisposed to at least one of the symptoms of sun poisoning. In that case study, a 37-year-old man presented with mental confusion after playing football in the sun. When the man was subsequently diagnosed with lupus, a condition known to be exacerbated by "direct, prolonged exposure" to the sun's UV rays, his medical team concluded that any confusion after sun exposure is worth investigating as possibly indicative of something more than mere sun poisoning.
Certain conditions can predispose you to sun poisoning
As noted above, sun exposure can exacerbate lupus symptoms (per a case study in Rheumatology). "Several effects of ultraviolet radiation at the molecular and cellular levels have been proposed to explain this," the study authors noted. The converse is true as well: People with lupus are more likely to develop sun poisoning than the general population (via Healthline).
Another condition associated with a higher risk of sun poisoning is xeroderma pigmentosum (XP), per Mt. Sinai. XP is a rare genetic condition that is characterized by extreme sensitivity to UV rays. It typically affects the skin and the eyes, but the nervous system may also be involved. Most adults who have XP have been dealing with it for as long as they can remember, with symptoms usually beginning by age two, often in the form of a severe sunburn from mere moments of sun exposure. Having XP means that any sun exposure at all is too much, including sun coming in through windows. Even fluorescent lightbulbs can damage the skin of people with XP.
Two other conditions are associated with a higher risk of sun poisoning: dermatomyositis and certain porphyrias. The former is a rare inflammatory condition characterized by weakness and what Mayo Clinic refers to as a "distinctive skin rash." The latter refers to several metabolic disorders that can cause photosensitivity (per Mayo Clinic).
Sun poisoning versus sunstroke
Sunstroke is another not-quite-medical term that often gets conflated with sun poisoning, along with sun allergy, sun rash, heat rash, heat stroke, and heat exhaustion. We've already covered sun allergy, sun rash, and heat rash, as well as the difference between a mere sunburn and what we think of as sun poisoning. What we've not yet covered is sunstroke, which is really the same thing as heat stroke, which is actually a severe case of heat exhaustion, per HCA Midwest Health.
HCAMH is yet another credible source of health information that does not acknowledge the existence of "sun poisoning," choosing instead to characterize a severe sunburn as just that. It apparently takes a similar position with regard to sunstroke. It recognizes that the word "sunstroke" is in common lay usage, but does not address sunstroke as an actual medical condition, choosing instead to characterize it as a serious condition caused by overheating without regard to the sun's rays.
In heat stroke, which has nothing to do with an actual stroke, the body becomes "so overheated that it is no longer able to cool itself," and that includes sweating. Heat stroke, which could occur contemporaneously with sun poisoning but is not related to the sun's UV rays, is a far more emergent scenario than most cases of sun poisoning. "If left untreated, it can lead to seizures, unconsciousness, and organ failure," according to HCAMH.
Certain medications can predispose you to sun poisoning
Sun poisoning, to the extent it's defined at all by medical professionals, is the result of overexposure to the sun in people who are sensitive to sun overexposure, per WebMD. But the notion of overexposure is relative, its threshold being lower for those who are more sensitive to the sun. And sun sensitivity is not necessarily a constant throughout life. As noted above, some medical conditions and certain medications can increase sun sensitivity. In fact, the FDA lists at least a dozen general categories of medications that can cause what it refers to as photosensitivity, each of which includes a number of specific formulations.
These include antibiotics (including cipro, tetracycline, and doxycycline), antihistimines (including loratadine, the active ingredient in Claritin, and cetirizine, the active ingredient in Zyrtec), cholesterol-lowering statin drugs, diuretics, NSAIDs, oral contraceptives, hormone replacement therapies, various tranquilizers, and several drugs used in the treatment of type 2 diabetes (including glipizide and glyburide). In addition, alpha-hydroxy acids found in some cosmetics can increase sun sensitivity.
Not everyone who takes these medications will experience increased sun sensitivity, but if you are taking any of these, you can err on the side of caution by wearing sunscreen and staying out of the sun between the hours of 10 a.m. and 2 p.m.
Sun poisoning can predispose you to skin cancer
If you never get a sunburn, you can never get sun poisoning. But even in the absence of a sunburn, any exposure to the sun increases your lifetime risk of skin cancer, according to Skin Cancer Foundation. Sun poisoning, which is defined by many as a severe sunburn, exacerbates that risk still further. To wit, "even one blistering sunburn in childhood or adolescence more than doubles your chances of developing melanoma later in life." So too does having five or more sunburns over the course of your life, regardless of severity.
Melanoma is the least common — and most deadly — form of skin cancer. But there is no "good" form of cancer, let alone skin cancer, and every bout of sun poisoning increases your risk of all forms of skin cancer, according to the authors of a 2016 study on relationship between severe sunburn and the risk of the three most common skin cancers (melanoma, squamous cell carcinoma, and basal cell carcinoma) published in the American Journal of Epidemiology. That said, whereas melanoma is more closely associated with severe sunburns (i.e., sun poisoning), squamous cell and basal cell carcinomas are "more closely associated with a pattern of continuously high sun exposure."
How sun poisoning should be treated
At the first sign of a sunburn, you should get out of the sun and start hydrating, if you have not already done so, according to the American Academy of Dermatology. Your next step is to "assess the damage," according to Health. If your sunburn develops blisters, that calls for a check-in with your healthcare provider in the interest of preventing infection and scarring, according to Connecticut dermatologist Dr. Deanna Mraz Robinson (via Allure). If you notice a rash, you'll want to bring that up with your healthcare provider as well. The same is true for any other symptoms that might bring your sunburn into possible sun poisoning territory.
To help you feel better, you'll want to do what you can to lower the temperature of your burned skin (per Health), including cool showers and cool compresses. You can also take an over-the-counter anti-inflammatory such as ibuprofen, and you definitely should if you develop a fever. Aloe vera gel may help cool your skin, according to Dr. Mary L. Stevenson, a New York City dermatologist. Just as drinking milk can help make spicy food more bearable, cold milk compresses can do the same for skin.
New York City dermatologist Dr. Julie Karen recommends avoiding the sun for at least a few days after sun poisoning. It's also worth keeping in mind that once you've had sun poisoning, you are now on notice that you are susceptible to it.
How to prevent sun poisoning in the first place
Literally no one is immune to sun poisoning. Just ask 21-year old Hannah Moussa, who was profiled by several tabloids, including the New York Post and The Sun, in June 2022 after she fell asleep while sunbathing and woke up "looking like a tomato" and feeling "like her face was going to explode." Not only was it the first time that the swarthy young woman had ever dealt with sun poisoning, it was also the first time she had ever even had a sunburn. Among other symptoms, Moussa experienced blisters, PLE rash, swelling, headaches, and vomiting.
Fortunately, for most people, sun poisoning is relatively easy to prevent. Just don't get a sunburn in the first place. To help avoid sunburn, stay out of the sun during the peak sunburn hours of 10 a.m. to 2 p.m. When you're going to be exposed to the sun at all, even on overcast days, always wear a broad spectrum sunscreen with an SPF of at least 30. Apply it 15 to 30 minutes before sun exposure, and reapply every two hours or immediately after bathing. And to the extent possible, wear protective garb such as sunglasses, hats, and clothing with built-in UV protection, per Cleveland Clinic. Lastly, take a lesson from Miss Moussa: don't fall asleep while sunbathing.