Should You Get A PCR COVID-19 Test Or A Rapid Test?
The Food and Drug Administration recommends getting tested for COVID-19 if you have been experiencing symptoms, have come into close contact with a person who has COVID-19, or have been in a high-risk situation where social distancing was not possible. Additionally, you should get tested if you were "asked or referred to get tested by your health care provider, or local or state health department," the FDA advises.
There are two types of COVID-19 tests you can receive: PCR test and rapid antigen, according to Harvard Health. Both tests are used to diagnose an active infection and can involve using a nasal or throat swab, or saliva collection. However, they differ from there. Using reverse transcriptase polymerase chain reaction, or RT-PCR, a PCR test can detect the genetic material of COVID-19. Once your sample arrives at a lab, "coronavirus RNA (if present) is extracted from the sample and converted into DNA. The DNA is then amplified, meaning that many copies of the viral DNA are made, in order to produce a measurable result," explained Harvard Health. PCR tests are remarkably accurate, but it can take several days to get a result.
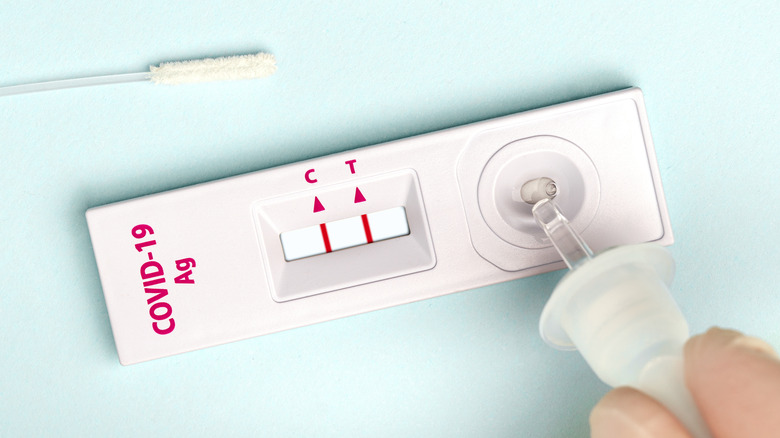
Antigen tests, also called rapid diagnostic tests, can deliver a result in less than an hour and work by detecting "specific proteins on the surface of the coronavirus," Harvard health detailed. Although false positives are rare, false negatives are more common with antigen tests. If you get a negative result, you may have to take another test or a PCR test instead to determine if that first result was accurate.
Which one should you choose?
Not sure which test to take? Both tests have their place.
A PCR test can detect COVID-19 earlier than an antigen test (via CNN Health). If you've been exposed or think you've been exposed to COVID-19, it's better to know early on if you have contacted the virus. This way, you'll be able to start treatment earlier if needed and will be better able to protect others, epidemiologist Emily Somers told CNN. "Up to two days before symptoms, or the one day or two days after symptoms (begin) people can have the highest risk of infecting others," Dr. Albert Ko, the Raj and Indra Nooyi Professor of Public Health at the Yale School of Public Health, added.
Still, rapid antigen tests are useful. The Centers for Disease Control and Prevention recommends taking a rapid test at the end of your five-day isolation. "Collect the test sample only if you are fever-free for 24 hours without the use of fever-reducing medication and your other symptoms have improved (loss of taste and smell may persist for weeks or months after recovery and need not delay the end of isolation)," explained the CDC. If you test positive, you should continue to isolate until 10 days have passed. If you test negative, you can end isolation but need to continue wearing a mask around others until the 10 days are up. "Having the presence of two rapid tests — two days in a row — that are both negative is a very good indicator a person is no longer infectious," Somers told CNN.