13 Common Causes Of Stomach Pain
For all but a gym-dedicated few, the abdomen tends to be a literal soft spot. But even without rock-hard abs, we shouldn't feel too vulnerable, since the abdomen is well protected. As Healthline states, "The abdominal muscles provide postural support, protect internal organs, and perform other important functions."
When describing the abdomen, it is commonly split into four quadrants. According to the American Academy of Family Physicians, the location of your stomach pain can give clinicians important clues about the problem you are experiencing. The right upper quadrant is home to the liver, gallbladder, part of the small and large intestines, part of the pancreas, and much of the stomach. The left upper quadrant hosts parts of the stomach, the spleen, and part of the small and large intestines. Pain in the lower left quadrant can include ovarian, fallopian tube, and uterine issues. It also holds part of the small and large intestines, including the sigmoid colon and rectum. The left kidney, ureter and half of the bladder also share this space. Lastly, the right lower quadrant includes urinary structures such as the right kidney, right ureter and right part of the bladder. Similarly, the right sided parts of the ovary, fallopian tube, and uterus share this quadrant. This part of the body is home to the small intestines, the first part of the colon, and the infamous appendix.
Here are some of the possible reasons why you experience stomach pain, and how to prevent or treat them.
Gastroesophageal reflux disease
Sometimes, spaghetti bolognese can prove to be a volcanic decision. That is because foods high in fat and acidity can trigger heartburn. According to the Mayo Clinic, heartburn occurs when stomach acid bubbles from its caldron into the esophagus. The cells of the esophagus are not adapted for a high pH environment, which is why they are susceptible to this condition.
It is normal for occasional heartburn to occur. However, frequent heartburn is commonly called gastroesophageal reflux disorder (GERD). It is important to manage frequent heartburn in collaboration with a medical professional like a gastroenterologist. This is because GERD can result in increased risks of dangerous conditions like ulcers, perforated organs, and certain cancers.
Fortunately, GERD can be treated very effectively with oral medications such as proton pump inhibitors like Prilosec and H2 receptor blockers such as Pepcid. These medicines are typically well-tolerated and inexpensive, especially when prescribed by a medical professional instead of purchased over the counter.
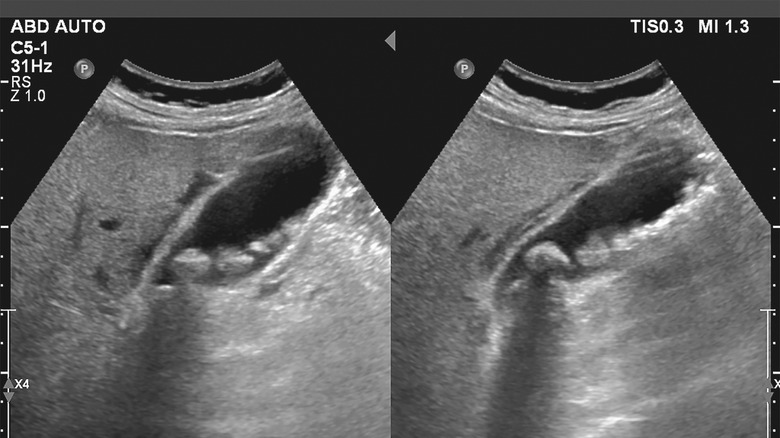
Abdominal aortic aneurysm
According to the Society of Vascular Surgeons (SVS), aneurysms occur when a portion of the blood vessel weakens, causing that spot to inflate as blood passes within it.
SVS notes that abdominal aortic aneurysm is what medical professionals call an aneurysm that occurs on the aorta, which serves a similar function to a central highway in a big city. It carries blood directly from the heart with branches to specific regions of the body. As you can imagine, an aneurysm in this location is particularly high risk. Thankfully, abdominal aortic aneurysms take time to develop and are rarely symptomatic until rupture.
A ruptured abdominal aortic aneurysm is often described as a severe, tearing sensation in the abdomen. Classically the pain radiates through the body towards the back, as if being impaled by a spear. Death can occur quickly.
This condition is strongly associated with males and tobacco users. Knowing this, screening recommendations for abdominal aortic aneurysm are well studied. Thus, your primary care provider can help keep you on track at annual check-ups. A screening test at the appropriate time can be the difference between fixing your aneurysm and dying because of it.
Gastroenteritis
Incidentally, the stomach flu has no relation to the influenza virus. Still, other viruses and bacteria may cause our stomachs to turn into knots and lead to vomiting and/or diarrhea. When this occurs, it is called acute gastroenteritis. As the American Academy of Family Physicians (AAFP) notes, "Infectious etiologies typically result in an acute onset of symptoms [and] viral gastroenteritis is particularly common."
So, what does the workup of nausea look like? AAFP describes a stepwise approach. "First, attempt to recognize and correct any consequences of the symptoms, such as dehydration or electrolyte abnormalities. Second, try to identify the underlying cause and provide specific therapies." It is particularly important to keep track of how symptoms began, where pain is located, and the timing of the discomfort. Things like gastroenteritis tend to begin quickly and without a characteristic pattern. Additionally, symptoms like diarrhea, muscle aches, fatigue and known sick-contacts all point to gastroenteritis.
Typically, gastroenteritis is caused by a viral infection. Thus, antibiotics have a very limited role in treatment. Even among bacterial causes, symptoms tend to be the result of toxin release as bacteria are killed by the immune system. So, antibiotics wouldn't do any good. Instead, good hydration and symptom control with anti-nausea medications can hold you over until symptoms resolve.
Constipation
Constipation is a significant cause of abdominal pain. Sure, it can be uncomfortable to talk about our bowel movement, but it is much more uncomfortable to leave constipation untreated. According to the AAFP, when constipation is left untreated, it "can lead to fecal impaction (with resulting fecal incontinence), particularly in older and confused persons." Additionally, this painful condition may factor into your risk of developing hemorrhoids or diverticular disease, though more research is required to support this idea.
How should we define constipation, then? Generally speaking, constipation is when a person experiences 2 or fewer bowel movements a week for 2 consecutive weeks. But this is not a hard-and-fast rule. Simply, if you aren't pooping as much as you usually do and you're feeling discomfort because of it, you would be wise to talk to your primary care provider.
Like so many medical conditions, the best way to manage constipation is to reduce your risk. The AAFP notes that risk factors include, "a low-fiber diet, low fluid intake, reduced mobility, consumption of drugs such as opioids and anticholinergic antidepressants, and Parkinson disease." Thankfully, there are many clinically effective treatments for people experiencing constipation. Dietary fiber supplementation, especially with psyllium, is a well-known home treatment. If that doesn't seem to help, laxatives may be of use. The AAFP notes that laxatives containing polyethylene glycol are among the safest, most effective laxatives available.
Hernia
The abdominal wall is composed of 7 layers. Typically, this is more than enough to keep our abdominal organs safe. However, a weakness in this tissue can cause abdominal contents to protrude through the abdominal wall. This is called a hernia.
There are many types of hernias, according to the Journal of the American Medical Association (JAMA). These include umbilical hernias at the belly button, inguinal hernias in the groin, and incisional hernias at points of prior surgery. As JAMA notes, "The first symptom of a hernia is usually a small bulging under the skin... but may produce discomfort and get larger..." Usually, hernia contents can be pushed back into the abdomen, but sometimes intestines become trapped which may compromise blood flow to the tissue. If this occurs, symptoms may include "pain, often with nausea, vomiting, or constipation."
Ways to properly deal with minor hernias include wearing ample support in the form of a truss or girdle, as well as taking a break from strenous work or heavy lifting. If the hernia is particularly bothersome, definitive treatment is achieved through surgical repair of the hole in the tissue.
Dysmenorrhea
The American College of Obstetricians and Gynecologists (ACOG) states that over half of women who menstruate "have some pain for 1 to 2 days each month." This pain is called dysmenorrhea. Dysmenorrhea should be evaluated by a obstetrics and gynecology clinician (OB-GYN) to ensure something more sinister isn't occurring. Uterine fibroids, adenomyosis and endometriosis can all present with similar symptoms.
The workup of dysmenorrhea may include a trial of medication, use of estrogen and progesterone containing contraception methods, ultrasound and even a procedure called laparoscopy. In this procedure, the examining physician makes a small incision near the patient's belly button, and then inserts a "thin, lighted camera" called a laparoscope into the abdomen. Laparoscopy allows an OB-GYN physician to get a direct visualization of one's pelvic organs to identify any abnormalities that may explain symptoms.
For mild dysmenorrhea, a class of drugs called non-steroidal anti-inflammatory (NSAID) medications can be very effective. This includes over-the-counter drugs like ibuprofen. That is because evidence suggests that a naturally produced chemical called prostaglandin may be the culprit behind menstrual pain. NSAIDs directly inhibit prostaglandins, leading to symptom relief.
Peptic ulcer disease
Peptic ulcer disease (PUD) causes abdominal pain when the lining of the gastrointestinal tract breaks down in one spot. Typically, a thick layer of mucous protects the GI tract, but in PUD, this mucous is absent, leading to auto-digestion of the exposed lining. If left untreated, PUD can lead to perforation of the stomach or intestine. As the American Academy of Family Physicians states, "The predominant causes in the United States are infection with Helicobacter pylori and use of nonsteroidal anti-inflammatory drugs," causing 48 and 24 percent of cases respectively.
Symptoms of PUD can range from mild to severe, though its usual symptoms are "episodic gnawing or burning epigastric pain; pain occurring two to five hours after meals or on an empty stomach." Evaluation for PUD can be done through various tests for H. pylori, including a blood test, breath test, or stool test. However, endoscopy and biopsy of tissue are the gold standards of diagnosis. If H. pylori is confirmed, antibiotics and antacids will likely be prescribed. Other lifestyle changes, such as eliminating NSAIDs, can be helpful as well.
Gallstones
The liver produces a substance called bile, which aids in fat digestion. Bile ducts within the liver collect bile and channel it out through a structure called the common bile duct. The common bile duct eventually meets with ducts from the pancreas, where it is sprayed into the duodenum to help digestion. But bile isn't produced on command — it requires a storage center we call the gallbladder. According to Johns Hopkins, it is a balloon-like organ that sticks to the liver and connects to the common bile duct. Thus, it can receive and store bile from the liver.
However, certain conditions can cause stones to form and sometimes lodge within the bile duct. This can lead to cholecystitis, an acute infection of the gallbladder. Cholecystitis presents with worsening abdominal pain in the right upper quadrant, commonly after eating a meal. Gallstones increase the risk of infection and damage to structures like the gallbladder, bile duct, liver and pancreas.
Typically, gallstones require surgical removal of the gallbladder called a cholecystectomy. This procedure is often done laparoscopically: The surgeon uses small incisions, long instruments, and a camera to perform the operation without opening the abdominal wall. Removal of the gallbladder is typically a well-tolerated procedure. Patients can go on to live a normal life without the organ, as the liver learns how to do the gallbladder's job.
Irritable bowel syndrome
Unexplained chronic constipation, diarrhea, or both can be a sign of irritable bowel syndrome (IBS). Unfortunately, it can be tricky to diagnose. According to Mount Sinai, "The way most doctors diagnose IBS is by gathering your history and ruling out other things like lactose intolerance, gluten intolerance, or some sort of bowel infection." Adding to this, they note that while there isn't any particular test for diagnosing IBS, a physician may suggest a colonoscopy "just to make sure the colon looks okay."
The main symptoms of IBS include crampy abdominal pain, gas, and changing bowel habits. Frequently, symptoms are resolved by having a bowel movement. Furthermore, IBS symptoms are more likely to wax and wane over time.
Treating IBS can be difficult, but several lifestyle factors have been associated with an improvement in symptoms. Avoiding coffee, tea, or colas can help. Along with this, symptoms may improve by eating smaller meals or increasing fiber intake. Medications are available, but it is best to talk to your primary care physician to find an option that works best for you.
Pancreatitis
Pancreatitis is the result of enzymatic digestion of healthy tissue. Authors of a study published by StatPearls identified the most common symptom of pancreatitis as abdominal pain in the area above the belly button and below the diaphragm, although it could occasionally happen in the chest or radiates toward the back as well.
Diagnosis of pancreatitis should take into consideration the presence of at least two of these three conditions: acute pancreatitis detected via abdominal imaging, abdominal pain that's consistent with acute pancreatitis, or a serum lipase level thrice the upper limit of the normal range or higher. Lipase is an enzyme produced in the pancreas which helps break down fat. It is produced in pancreas cells and excreted into pancreatic ducts, where it later is squirted onto food in the intestines. If lipase and other enzymes escape the pancreas, they can begin digesting the organ itself, leading to unique and intense symptoms.
There is no medicine that can cure pancreatitis. Rather, giving the organ time to rest and heal is all the treatment needed. This is usually done in the hospital with aggressive IV fluid administration, coupled with a short period of not eating or drinking.
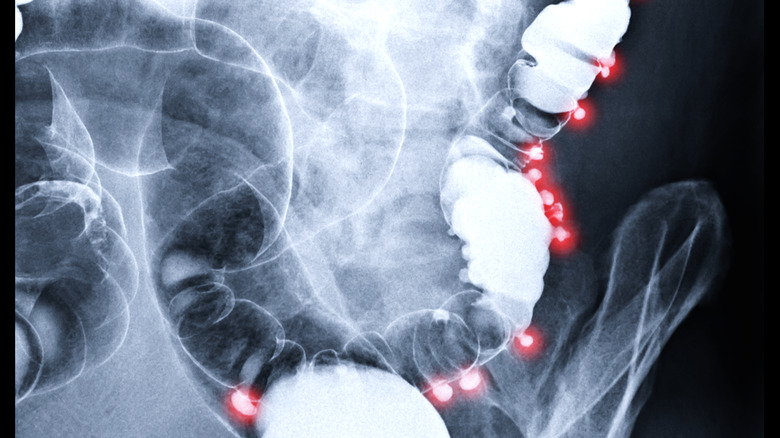
Diverticulitis
We like to think of the intestines, both large and small, as a perfectly shaped tube. And for most of the GI tract, this is true. However, parts of the large intestine can be pocked with small pouches or bulges called diverticula (via the Cleveland Clinic). The presence of diverticula in the colon is common and generally non-problematic. However, if one of these pouches becomes inflamed, abdominal pain can occur. This condition is called diverticulitis. The development of diverticulitis is complicated. A lack of fiber in the diet may be a major contributor, it can cause "a buildup of waste (constipation) in your colon." When you are constipated, the walls of your colon feel the additional pressure, which can lead to the formation of diverticula in your colon's "weak areas."
The characteristic symptoms of the condition may include left lower quadrant pain, fever, nausea and/or vomiting, and (occasional) rectal bleeding. Notably, the diagnosis of diverticulitis consists of multiple modalities, including blood tests, CT scans, colonoscopies and stool sample examinations, to name a few. Treatment consists of various antibiotic options, as well as pain medication and changes to diet. Sometimes, though, diverticulitis is severe enough to warrant the removal of the inflamed section of the colon.
Appendicitis
Picture this: A patient has new and intense pain in the right lower quadrant with associated fever, nausea and/or vomiting. This characteristic patient presentation is classic for appendicitis, according to Johns Hopkins Medicine.
The appendix is a small tubular structure sitting on the colon. This tube connects directly with the cecum, or the first part of the colon. Thus, colon bacteria can live within the organ, causing no problems. However, if the appendix becomes inflamed, the tube may seal, allowing the resident bacteria to grow unchecked. This can lead to infection, the creation of an abscess, and even a life-threatening perforation of the appendix. Ironically, perforation of the appendix can actually lead to a temporary resolution of symptoms. However, this is a medical emergency requiring immediate surgical intervention.
Appendicitis can be diagnosed through a combination of physical exam findings, diagnostic labs, and imaging studies performed at the emergency department. Blood tests would likely include a complete blood count to assess signs of infection, as well as a complete metabolic panel to monitor abdominal organ function. However, diagnostic imaging via CT scan remains the gold standard for diagnosing appendicitis. This condition is treated by a general surgeon, often urgently, via a procedure called an appendectomy. A surgeon will cut and seal the appendix, removing it from the body and ensuring that the abdomen will not sustain further damage.
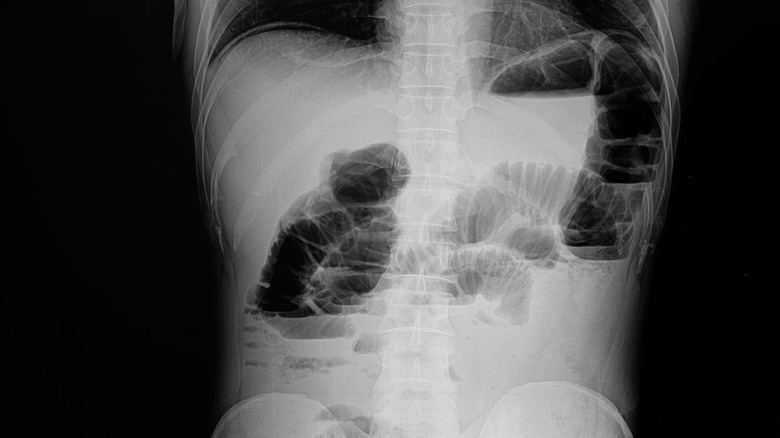
Small bowel obstruction
Humans have about 22 feet of intestines coiled within the abdomen. It is amazing that kinks and tangles do not regularly happen. That said, things can sometimes go wrong. Twists in the bowels can cause the tube to become pinched, akin to how headphones can tangle in your pocket. When this happens in the intestines, it is called a small bowel obstruction. According to an article in StatPearls, the two most common causes of small bowel obstruction are postsurgical adhesions and incarcerated hernias. Adhesions are strands of sticky scar tissue that form inside the abdomen after surgery. They sometimes cause the bowels to narrow at distinct points.
The most common way the condition manifests is through "complaints of abdominal pain, distention, nausea, and vomiting." During a physical examination, a clinician may find reduced and high-pitched bowel sounds, as well as abdominal tenderness that "may be diffuse or focal with the presence of distention." Furthermore, the clinician may also notice peritonitis signs like "rebound, guarding, and rigidity." A diagnosis can be made with a CT scan of the abdomen and pelvis, which would reveal the exact point in the intestines where the obstruction is occurring. An expert can see the distension from increased pressure on one side of the intestines and a narrowing on the other side of the blockage.
Treatment includes antibiotics, fluid resuscitation, pain control, and nasogastric decompression. In such cases, though, you shouldn't put off a surgery consultation.