When You Have High Cholesterol, This Is What Happens To Your Body
If you have been told by your doctor that you have high cholesterol, then you're in the company of tens of million others in the U.S., according to the American Heart Association (AHA). Between 2015 to 2018, the last time period for which the AHA has data, around 28 million adults over the age of 20 had a cholesterol reading of 240 or higher, which the definition of "high cholesterol." That's nearly 12% of all adults in the U.S. Of those, the largest race and gender demographic with high cholesterol is white females (13.1%). The next most likely demographics to be diagnosed with high cholesterol are Asian males (13%), followed by Hispanic males (12.4%), Black females (10.5%), Asian females (10.3%), white males (10.1%), and finally Black males and Asian females, who were tied at 9.2%.
Clearly, high cholesterol is an equal-opportunity condition. Further, as many as 7% of all children and adolescents in the U.S. have high cholesterol, according to the Centers for Disease Control and Prevention (CDC). And that's only counting the people who have had their cholesterol tested by healthcare professionals, since high cholesterol can be measured only via blood test, the CDC also states. Perhaps that's why just barely over half of U.S. adults who might be benefitting from cholesterol-lowering medication are actually taking it. So, what exactly is cholesterol, and what happens to your body when your cholesterol is said to be high?
What is high cholesterol and what are the symptoms?
Cholesterol is not fat, but rather, a fat-like substance that is found in every cell of the human body, according to MedlinePlus, and it's there because our bodies need it — among other reasons, to make the hormones needed to keep our metabolisms running and to manufacture vitamin D from sunlight. We're guessing that you've never seen any (legitimate) supplements purporting to raise cholesterol levels, though, and that's because the human body is quite efficient at manufacturing all of its own cholesterol needs. Although some foods, all of which are animal products, contain cholesterol, what actually causes cholesterol to rise beyond optimal levels is not the ingestion of those foods so much as a number of factors relating to your overall diet — and most particularly, the "mix of fats and carbohydrates" you consume, according to Harvard T.H. Chan School of Public Health.
The presence of high cholesterol levels in the blood is associated with no telltale symptoms, according to the CDC. Only a healthcare professional can confirm your cholesterol levels, and only through an analysis of your blood. Fortunately, cholesterol testing is a standard of care at well health visits. In addition, high cholesterol is associated with a number of health conditions that may present with symptoms of their own. If you go to your healthcare professional complaining of any of those symptoms, then they may wish to test your cholesterol levels.
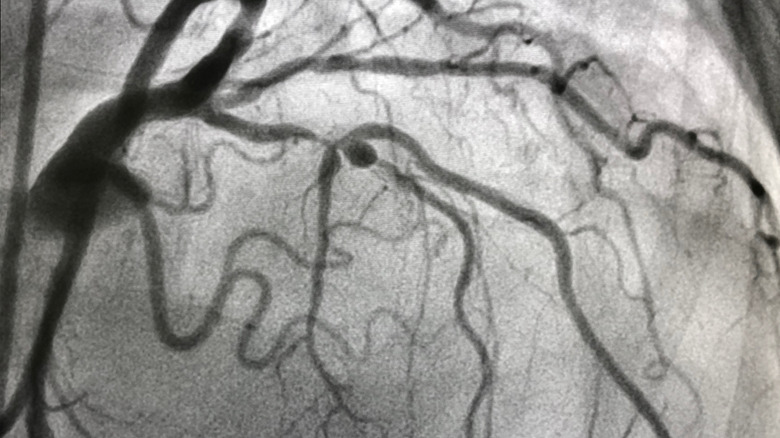
High cholesterol can cause plaque buildup in the blood
Excess cholesterol circulating in your blood can cause "plaque" to form in your circulatory system, per the CDC. When plaque builds up, it can interfere with optimal circulation (via Beaumont Health). There are no known symptoms of plaque buildup, but when it reaches a critical mass, so to speak, then you may experience symptoms of atherosclerosis, which Mayo Clinic defines as "the buildup of fats, cholesterol, and other substances, in and on your artery walls," that causes the narrowing and stiffening of the arteries. Atherosclerosis is also known as coronary artery disease (CAD), coronary heart disease, and ischemic heart disease. Whatever you may wish to call it, the CDC says it's the most common type of heart disease in the U.S.
Atherosclerosis in the arteries leading to and from the heart can cause chest pain and/or pressure. Known clinically as "angina," these sensations constitute a major symptom of heart attack. And this is often the symptom that motivates the person experiencing it to reach out for medical assistance. Whether or not a heart attack is diagnosed, the presence of angina will lead to your having a blood test that may reveal high cholesterol as well as any number of other indicators of heart disease and other conditions caused by high cholesterol. If you have experienced angina and are diagnosed with high cholesterol, it's possible that you have one of these other conditions as well.
It can cause peripheral artery disease
When high cholesterol causes plaque buildup in the bloodstream, the consequences may be observed not only in the heart but in other parts of the body, as well. For example, peripheral artery disease (PAD) affects blood flow to the limbs — often the legs in particular, according to Mayo Clinic. In its early stages, PAD often has no symptoms. However, as it progresses, PAD can lead to pain while walking, known clinically as "claudication." Claudication is most noticeable while you are walking, and tends to abate upon resting. The pain may feel like cramping in the hips, thighs, or calf muscles. Peripheral artery disease can also present as numbness, coldness, weakness, or change in color of the limbs, as well as sores on the limbs that won't seem to heal — all of which are caused by decreased circulation. If allowed to progress further, pain may be experienced while performing any kind of physical movement or activity.
Like coronary artery disease/atherosclerosis, PAD can signal that one is at an increased risk of heart attack or heart failure. In addition, both CAD and PAD can increase the risk of stroke, blood clot, kidney disease, and amputation of a limb due to death of the tissue (necrosis) to which blood flow has been restricted.
It can increase your risk of high blood pressure
High cholesterol is a risk factor for heart disease, according to Healthline. So, too, is high blood pressure. When someone has both high cholesterol and high blood pressure, the risk of heart disease is even greater than the sum of their parts, so to speak. Moreover, this is true even if your numbers are only slightly higher than recommended. In addition, elevated cholesterol levels in the blood can contribute to the formation of plaque, per CDC, and plaque buildup can interfere with optimal blood flow through the circulatory system, even if that buildup has not yet reached the level of atherosclerosis (the term for more advanced plaque buildup). Indeed, even at earlier stages, plaque buildup may be enough, in and of itself, to cause the blood pressure to become and remain elevated (via Cleveland Clinic).
Moreover, the consequences of having both high cholesterol and high blood pressure are not mitigated by the fact that the high cholesterol may have caused the high blood pressure. In other words, even if it was your high cholesterol that caused your blood pressure readings to rise, your risk of heart disease is still worse than if you were living with only one of these conditions.
If your cholesterol is high, it can increase your risk of stroke
One of the things that happens to your body when you have high cholesterol is that your risk of stroke increases, per the Stroke Association. The reason is that excess cholesterol can contribute to the buildup of plaque in blood vessels, thereby stiffening and narrowing the arteries, which may have the effect of impeding optimal blood flow, per CDC. When this happens, blood clots may form, with the result being an ischemic stroke, according to University of Michigan Health. A transient ischemic stroke is said to occur when a blood clot that causes stroke symptoms resolves on its own. These "TIA" strokes are associated with the risk of a future stroke, and one which may not resolve on its own.
Even without the formation of a blood clot, however, a stroke may occur when obstructed blood flow creates enough pressure in a blood vessel to cause the blood vessel to burst/rupture. When the rupture restricts blood flow to the brain, it's known as "hemorrhagic stroke." Further, a stroke may occur with no symptoms being observed (e.g. the person is sleeping or otherwise unaware). This is known as a "silent cerebral infarction" or "silent stroke." A silent stroke is often caused by atrial fibrillation, which is a form of irregular heartbeat commonly seen in people older than age 65, and it is also associated with high levels of HDL, according to a 2014 study published in the Journal of the American Heart Association.
You're at higher risk for gout flare-ups
Gout is a painful inflammation in one or more joint. Generally speaking, however, gout can't be diagnosed through the presence of pain alone. For a gout diagnosis, uric acid levels in the blood must be elevated (i.e., uric acid levels measured above 6.8 mg/dL, per Hyperuricemia), which requires bloodwork to ascertain. Unlike other forms of arthritis, gout causes pain because of uric acid forming crystals that settle in the joints, causing pain and inflammation (via Creaky Joints) — although not everyone with excess uric acid will necessarily end up experiencing the painful condition associated with a gout attack (via Cleveland Clinic).
If you have already had an attack of gout or are known to be at risk, then having high cholesterol can increase your chances of having a gout flare-up, according to a 2019 study published in the Annals of Rheumatic Diseases. All of that study's subjects were already gout patients, but researchers found that those with higher cholesterol levels tended to have more frequent gout attacks. The researchers theorized that "higher levels of cholesterol can activate the innate immune and induce inflammatory response," thus lowering the threshold for a gout attack and increasing its duration. Although the causal connection has not been established as scientific fact as yet, it is nevertheless known that both gout and high cholesterol are associated with obesity, high blood pressure, and insulin resistance, as well as with metabolic disorder, per Vascular Health Clinics.
The relationship between high cholesterol and anxiety
When you have high cholesterol, it may negatively impact not only your physical health, but also your mental health, according to MD Edge Psychiatry. As the site points out, in a number of scientific studies, "high cholesterol levels have been associated schizophrenia, obsessive-compulsive disorder, panic disorder, generalized anxiety disorder, and posttraumatic stress disorder." What is not entirely clear, however, is whether a causal relationship exists, and in which direction it may go, according to Dr. Hooman Madyoon of the Beverly Hills Vein and Cardiovascular Institute.
Dr. Madyoon theorizes that anxiety may cause metabolic changes that cause cholesterol levels to become higher, all other things being equal (including diet). On the other hand, it is also possible that some of the metabolic changes that are caused by high cholesterol levels (for example, the buildup of plaque in the arteries and related physical symptoms) may contribute to anxiety by undermining the function of the nervous system, as was suggested by a 2014 study published in the journal Behavioral and Brain Functions. In that particular study, rats who were fed a high-cholesterol diet and then placed in a maze were found to exhibit both anxious behavior and neurochemical changes associated with anxiety in rats. More research is needed with regard to the relationship between high cholesterol and mental health problems, but there does appear to be a connection.
High cholesterol may offer some protection against depression
"For the last quarter century, we have been told that cholesterol is dangerous for our health and were advised to avoid it in order to live a healthier life," wrote Dr. James M. Greenblatt in a 2015 essay published by The Great Plains Laboratory. "However, cholesterol is essential in maintaining good mental health [because] the brain is the most cholesterol-rich organ in the body, and depriving the brain of essential fatty acids and cholesterol can lead to detrimental health problems." For example, as Dr. Greenblatt pointed out, citing a numerous studies and one 2008 meta-analysis published in Annals of Behavioral Medicine, lower cholesterol levels are associated in various studies with an increased risk of depression
Likewise, a 2008 study published in the Annals of Behavioral Medicine demonstrated that higher total cholesterol levels were associated with lower levels of depression. A 2010 study published in Biological Society showed that in elderly women, low levels of HDL (the "good cholesterol"), in particular, were associated with higher depression risk, not to mention greater risk of cardiovascular disease. This study also showed that men with lower levels of LDL — the "bad" cholesterol — were at greater risk for depression, though the plus side is they were lower risk for cardiovascular disease. There is clearly a lot to be learned still in this area, but for the moment, it seems well-accepted that having below-normal levels of cholesterol can put you at a greater risk of depression.
If you or someone you know is struggling with mental health, please contact the Crisis Text Line by texting HOME to 741741, call the National Alliance on Mental Illness helpline at 1-800-950-NAMI (6264), or visit the National Institute of Mental Health website.
Low cholesterol is associated with a higher rate of suicidal depression
"There is strong scientific evidence indicating that low cholesterol and suicide, particularly violent suicide, are linked," according to Dr. James M. Greenblatt, per The Great Plains Laboratory. Examples offered by Dr. Greenblatt included a 2004 study, which found that among depressed patients who had attempted suicide, the average total cholesterol reading was 150 mg/dL, as compared with 180 for depressed but non-suicidal patients and 190 among a non-depressed control group, and concluded that low total cholesterol could be used "as an indicator of suicide risk." Dr. Greenblatt's evidence also included a 2008 study published in Psychiatry Research, which demonstrated that among 35 people who attempted suicide, those who had opted for "violent" means had "significantly lower total cholesterol" levels than those who had opted for non-violent means.
Of course, as with the relationship between high cholesterol and anxiety, there is an unresolved question of causation when it comes to the relationship between high cholesterol and depressive ideation and behavior. As a 2000 study published in the academic journal Bipolar Disorder pointed out, "Cholesterol may be a state rather than a trait function, and may be influenced by the acute mood state."
If you or anyone you know is having suicidal thoughts, please call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).
High cholesterol can harm your eyes
If you have high cholesterol and you let it go unchecked for long enough, you may run the risk of damaging your eyesight and your eyes. One of the main health concerns high cholesterol can cause is plaque buildup in the arteries, which may present with chest pain and pressure. As it turns out, that plaque can also break off from the walls of your arteries and get stuck in the small blood vessels of the eye, as ophthalmologist Nicole Bajic explained to the Cleveland Clinic. And this can cause vision trouble or full-on vision loss, Dr. Bajic says.
Other ways that high cholesterol can change your eyes include a condition called "arcus senilis," or "corenal arcus," which causes a "white or grayish ring or halo [to develop] in the periphery of the cornea, the clear layer of your eye that protects your iris" (via Cleveland Clinic). However, the ring itself doesn't interfere with your eyesight, according to Dr. Bajic, nor do the little nodules of yellow fat that may appear around on the skin around your eyes if you allow your high cholesterol to go unchecked for long enough. These are known as "xanthelasma," and while they aren't physically painful, they can be distressing, Dr. Bajic notes.
High cholesterol may be associated with tendon issues
Though it may not be the first consequence of high cholesterol that comes to mind, it turns out that high cholesterol can damage your tendons, according to the footcare professionals at Alliance Foot & Ankle Specialists (AFAS). The site notes that people with high total cholesterol — or even just elevated LDL cholesterol (the "bad" kind) — tend to have more tendon pain. Since the Achilles tendon is the biggest tendon in the body, a significant amount of research has developed with regard to the connection between high cholesterol and Achilles pain and rupture.
One theory as to why those with high cholesterol are more likely to experience problems with their Achilles tendon is that cholesterol deposits, known as xanthomas, are prone to developing in the Achilles tendon, as explained in a 2005 study published in the European Journal of Clinical Investigation. The presence of xanthomas in the Achilles tendon can cause biomechanical issues as well as discomfort. Another theory, one posed as a possibility by a 2021 study published in PLOS One, is that genetic predisposition to high cholesterol may be bundled with the genetic predisposition to Achilles dysfunction. Still another theory is that the buildup of cholesterol in the blood triggers inflammation in the body, which can have deleterious affects on the tendons, including the Achilles (via AFAS).
Both high AND low cholesterol levels can be problematic
Generally speaking, we associate high cholesterol with worse health outcomes and low cholesterol with better ones. Although there is some level of truth to this, the reality is far more nuanced — as it turns out, having your cholesterol levels be too low may cause its own set of problems. A 2016 study published in the Clinical Journal of the American Society of Nephrology suggests that when it comes to the "good" cholesterol, HDL, any extreme of cholesterol status can be harmful to your health.
"Having elevated or low [HDL] levels are both equally harmful," according to the American Journal of Managed Care (AJMC) in an article about the 2016 study, which included data on more than 1.7 male U.S. veterans. Those with low HDL cholesterol levels were more found to be more likely to die prematurely from all causes than those with middling HDL levels. "The relationship between increased levels of HDL cholesterol and early death is unexpected and not fully clear yet," according to senior study author, Dr. Ziyad Al-Aly. But what seems clear for the moment is that "the risk of premature death increases at both ends of the spectrum."