Dr. Nora Lansen On Holistic Primary Care, Doctor-Patient Relationships, And Mental Health - Exclusive Interview
When she evaluates a patient, Dr. Nora Lansen, primary care physician and virtual clinical director at Galileo, doesn't just talk to them about their physical symptoms. She also asks about their lifestyle, their stress levels, and their trauma history because she knows that mental health is directly related to physical health. Dr. Lansen uses all these details to build a complete picture of each of her patients so she can assess the cause of their symptoms, which is sometimes more mental than physical.
In many traditional primary care settings, doctors don't have the time or resources to get all these details — not because they're bad doctors, but because the healthcare system isn't set up to allow doctors to dedicate the needed time and energy to their patients. When this happens, doctors can easily miss crucial clues that point to underlying mental health issues.
In an exclusive interview with Health Digest, Dr. Lansen revealed how she builds solid, trusting relationships with her patients, how she cares for their mental health as well as their physical health, and what common symptoms can point to underlying problems with mental health.
Building the doctor-patient relationship
Can you tell us a little bit about your background and why you decided on a holistic approach to primary care?
My path to a career in healthcare was somewhat circuitous. I have an undergraduate degree in creative writing and a Master's degree in literature. I've always been interested in the human condition — not just how the human body works, but how we experience the world. Once I started my journey into healthcare, I gravitated toward primary care because I found it to be the one area of medicine that really perceives the patient as a whole person, not just a composite of discrete body systems. In primary care, we consider a multitude of elements when evaluating a person's well-being – lifestyle, stressors, past impactful experiences, how a person relates to the world, what "being healthy" looks like to them — variables that meaningfully contribute to a patient's overall health.
Why is a patient's relationship with a primary care physician so important?
One of the benefits of a solid relationship with a primary care provider is that it promotes openness and honesty, which can directly impact a patient's health. Glossing over a sensitive detail or feeling too embarrassed to open up about a weird symptom can lead to an inaccurate diagnosis and delayed treatment.
In general, no matter what your health concern is, it's a whole lot less stressful to talk to someone you feel comfortable with. Since we know that stress negatively impacts health, an anxiety-free visit with a PCP is exactly the right idea.
How do you focus on building that relationship with your patients, and how can doctors make their care more relationship-focused?
Most doctors in practice today are aware that a paternalistic approach to medicine doesn't benefit the patient. Delivering care in a bossy way neither contributes to a good patient experience nor does it improve health outcomes. Interactions between patients and providers should always be patient-centered.
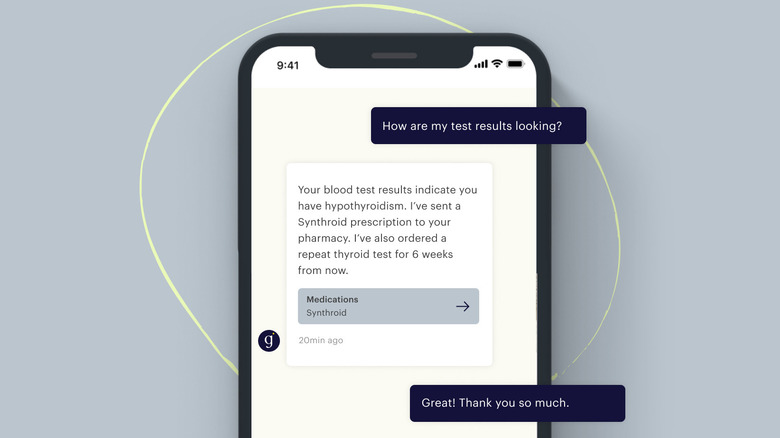
Effective communication should be a central focus, whether in person, by text, by phone, or by video. It's critical for the primary care provider to be a receptive listener — to create space that allows a patient to say what they have to say without feeling pressured or rushed. This can be difficult in a traditional outpatient setting, when visits are brief and the office is busy. But it's when patients feel rushed that they are most likely to leave out relevant pieces of information about their health.
Creating health equity with telemedicine
What makes Galileo so unique, and why do you think Galileo is able to attract some of the best healthcare providers to work there?
Galileo's mission is to provide affordable, high-quality, 24/7 access to healthcare for all. It's a unique and very meaningful goal. That makes it easy for us to attract the best healthcare providers from across the country: smart, experienced clinicians who are devoted to providing high-quality care and who want to escape the administrative burden of the traditional medical model. As virtual care has become more mainstream, patients and providers alike have come to realize the inherent transformative power of digital care. Healthcare is a human right. It should not be an optional bonus for those who have the means to access it. Providing care digitally is one of the most sensible ways to increase access to care.
How is virtual primary care changing access to healthcare?
Virtual primary care is reliably enabling access. The current infrastructure of healthcare in the U.S. is so complex and the process of accessing care in a traditional setting so onerous that many people try to avoid it altogether. It shouldn't be that way. For most people, an in-person doctor's visit involves taking time off of work, going to a doctor's office, sitting in a waiting room, sometimes for hours, and chatting with a clinician for mere minutes. Often, there's not enough time to address even half of the items a patient wants to cover. Doctors are so busy recording everything that sometimes, they barely seem to be paying attention.
Virtual care removes many of these barriers. It provides access to clinicians when and where it's most convenient for the patient, without the hassle of a waiting room and without taking time off from work. Anyone with an employer health plan should ask their HR team if they offer access to Galileo, or they can visit https://galileo.io/get-galileo/ for info on how to sign up as an individual.
Caring for physical and mental health
How do you, as a primary care physician, help care for people's mental health as well as their physical health?
It's almost impossible to address any physical concern without also assessing a patient's emotional well-being. Through active listening, primary care providers can pick up on all sorts of information, including things that may seem unrelated at first, but ultimately provide important details about what's going on for someone.
For example, a patient might express concern that she's experiencing stomach pain every night after dinner. She thinks it must be acid reflux and asks for a prescription. The patient describes what she's been eating and tells her PCP it's probably from all of the processed food she's been snacking on lately. Her PCP takes a moment to ask why she's been eating more processed foods than usual, and she explains that she's been putting in way more time at work because there have been a lot of lay-offs at her company and she's worried about losing her job, so she ends up ordering take-out or grabbing food from the vending machine.
That information takes the conversation in a direction that results in a diagnosis of anxiety, and that warrants a very different treatment plan than one she would receive for acid reflux. Since primary care providers are knowledgeable about symptoms from head to toe, we can elicit key pieces of information that serve as guideposts along the way to an accurate diagnosis. Because we are trained to manage a full spectrum of issues, we can treat a range of conditions, from acid reflux to anxiety and many things in between.
Why do mental health struggles sometimes manifest as physical symptoms?
We've long known that there is a connection between mind and body. Science hasn't yet fully explained the biochemistry of it, but emerging research demonstrates all sorts of interesting links. For instance, there is evidence that a relationship exists between the bacteria that occupy our digestive system – our "gut flora" — and the effective functioning of our neuroendocrine system, which directly impacts our behavioral health. More of these connections will be revealed over time and will better explain how intricately linked our physical and mental health is.
In the meantime, simply maintaining an awareness of the mind-body connection is important. Exercise, meditation, adequate sleep — optimizing the basics as much as possible helps to ensure overall wellness.
How mental health impacts physical health
What symptoms can indicate an underlying mental health issue?
Common symptoms of anxiety and depression include fatigue, weight change, headache, chest pain, palpitations, and stomachache. These aren't the only symptoms; they're just some of the most common ones. Almost anything — including visible signs, like hives — may have emotional distress as a root cause. This is not to say that every physical symptom is fabricated by an anxious patient, simply to say that many mental health issues can manifest physically.
If you see those kinds of symptoms in a patient, what steps do you take to assess whether they may have an underlying mental health issue?
It's important to consider all possible diagnoses and contributing factors, so an initial evaluation often involves testing, like bloodwork, to evaluate for a physical cause. For instance, hypothyroidism is a clinical condition that has many of the same symptoms as depression. If a patient is tired and gaining weight, in addition to assessing for depression, a clinician might order a thyroid blood test.
There are validated mental health assessments — like the GAD-7 for anxiety and the PHQ-9 for depression — that help to narrow a diagnosis of a mental health issue through a series of questions and answers. Often, the first step in the treatment of a mental health issue is to establish care with a skilled mental health professional, like a talk therapist. A patient's response to treatment can actually help to confirm a diagnosis.
Are physical illnesses due to underlying mental health struggles becoming more prevalent? If so, why?
The scientific community is becoming increasingly aware of the impact of mental health issues on the body. For example, depression seems to be a contributing factor to heart disease. In a more nuanced way, mental health contributes to a variety of other chronic conditions; depression can lead to overeating, which can lead to weight gain, which can lead to diabetes. The mind-body connection is strong in both subtle and overt ways.
Learn more about Galileo at https://galileo.io/.
This interview was edited for clarity.