Hyperhidrosis Explained: Causes, Symptoms, And Treatments
Sweating is a vital function carried out by the human body (per WebMD). Not only does it help to lower core temperature, but it also helps ensure the body maintains a normal temperature range. However, when your body loses its ability to control how much sweat is produced, it can be a sign of a disorder called hyperhidrosis.
According to the Journal of the American Academy of Dermatology, hyperhidrosis is a disorder of the skin that affects roughly 4.8% of the population in the United States. With more than 2 million sweat glands found on the human body, overactivity of these glands caused by hyperhidrosis may result in readily apparent symptoms, the most common being excessive sweating (via Shanghai Chest).
The good news is that hyperhidrosis is not a life-threatening condition. It can be easily diagnosed by a healthcare provider simply by taking a proper (life) history and physical exam. Even more, hyperhidrosis has several treatment options, including various oral medications, prescription-strength deodorants, surgical procedures, and medical devices. Let's take a look at the symptoms, causes, and treatments for hyperhidrosis.
Regulating body temperature
A normal body temperature, according to Informed Health, averages around 98.6 degrees Fahrenheit. It is also the case that each individual has their own unique "normal" temperature, which may be slightly higher or lower than the 98.6 degrees Fahrenheit average. In a healthy individual, this "normal" temperature will also fluctuate, mainly in response to changes in your surrounding environment, during vigorous activities such as exercise, and possibly even based on the time of day during which your temperature is measured.
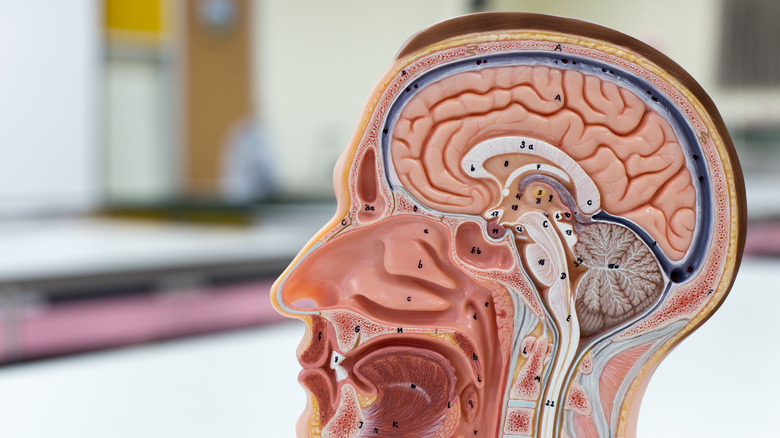
Your body temperature is regulated by a part of your brain called the hypothalamus. You might recognize the hypothalamus as also being responsible for controlling hunger, thirst, mood, sleep, and your sex drive (via MedlinePlus).
One of the most important roles of the hypothalamus is to continually monitor your body's internal temperature. When your core body temperature falls too high or too low from normal, the hypothalamus will send signals to various organ systems throughout the body so they can make the appropriate adjustments in returning the core temperature back to normal.
When your temperature drops below 98.6 degrees Fahrenheit, your hypothalamus tells the body to generate more heat, often through shivering or raising of the basal metabolic rate, also known as BMR (per American Family Physician). On the contrary, when your temperature rises above 98.6 degrees Fahrenheit, signals from your hypothalamus are sent to stimulate sweat glands in the skin throughout the body. Once on the surface of your skin, the sweat is able to cool down the body by a process called evaporative cooling (via Advances in Physiology Education).
This overall process by which the body maintains a constant core temperature is referred to as thermoregulation.
The types of hyperhidrosis and their causes
Hyperhidrosis, according to the Cleveland Clinic, is a condition defined by your body sweating more than necessary. In order to better understand this condition, hyperhidrosis is commonly separated into two distinct categories: Primary and secondary (per the Journal of the American Academy of Dermatology).
Primary hyperhidrosis, also known as idiopathic hyperhidrosis, refers to excessive sweating for at least six months due to an unknown cause (via NCBI StatPearls). According to the Journal of the American Academy of Dermatology, this type of hyperhidrosis shows a pattern of sweating that is described as focal, meaning that the excessive sweating is most prominent in the underarms, palms of the hands, soles of the feet, and the head.
On the other hand, secondary hyperhidrosis is due to an identifiable cause. This type of hyperhidrosis may display a pattern of sweating that is either focal, localized, or distributed across the whole body (commonly referred to as generalized).
The cause of primary hyperhidrosis is not fully understood. One theory suggests that it might be due to a malfunctioning nervous system, leading to an overstimulation of otherwise healthy and normal sweat glands. Another theory suggests that primary hyperhidrosis could be the result of an abnormal control of emotions. This theory suggests that the "sweat center" of the hypothalamus may be under complete control of the parts of the brain that regulate emotions and that it's disconnected from the parts that regulate temperature.
Meanwhile, secondary hyperhidrosis is much less common and differs from primary hyperhidrosis in that it has an identifiable cause. A number of conditions, diseases, and medications can result in secondary hyperhidrosis (via Dermatologic Surgery). Some of the more common causes include fever, pregnancy, and menopause. Less commonly, secondary hyperhidrosis will be a result of an underlying medical condition.
Conditions that may trigger hyperhidrosis
According to VisualDx, there are a number of medical conditions that can trigger excessive sweating.
Hyperhidrosis that is localized to the underarms, palms of the hands, soles of the feet, and the head may be the result of Frey syndrome, peripheral neuropathy, spinal cord injury, anxiety, or obesity. Frey syndrome is a rare complication resulting from injury to the salivary (parotid) gland in the cheek (per the National Organization for Rare Disorders). Peripheral neuropathy refers to the many conditions that stem from damage to the peripheral nerves, according to the Mayo Clinic.
Generalized hyperhidrosis, or excessive sweating not localized to any specific part of the body, is often the result of various metabolic diseases, neurologic conditions, infections, medications, or substance abuse (per VisualDx).
Diabetes and hyperthyroidism are two of the most common metabolic causes of hyperhidrosis. In terms of infections, hyperhidrosis can be triggered by tuberculosis, malaria, or brucellosis. Neurologic causes include stroke or Parkinson disease. Some other conditions that may cause excessive sweating include congestive heart failure, lung cancer, and lymphoma.
With regards to medications that can result in hyperhidrosis, the list is long and extensive. However, some of the most commonly prescribed medications include antidepressants, ciprofloxacin (an antibiotic), acyclovir (an antiviral), and Tylenol.
Signs and symptoms
According to the Cleveland Clinic, symptoms of hyperhidrosis not only vary greatly in their severity, but will also affect each individual differently. Excessive perspiration, being the most common and apparent symptom, may ebb and flow over a long period of time. It may also present as a constant everyday challenge.
Excessive sweating may be severe (per the American Journal of Managed Care). Some cases of hyperhidrosis may result in the pooling of sweat under the arms and around the back to the point where someone would need to change their clothes just to feel comfortable again. Other cases of hyperhidrosis might be less severe, in which sweat may simply bead on the cheeks or forehead, and occasionally drip down onto other parts of the body or the floor.
Excessive sweating caused by hyperhidrosis may also lead to itching, inflammation, and possibly even infection. These would be caused by sweat irritating the affected area. Excessive sweat may also result in a foul-smelling body odor, caused by certain bacteria on the skin flourishing in the moist environment. Skin changes, such as paleness, discoloration, cracks, or wrinkles could be another sign of hyperhidrosis, as constant and excessive sweat disrupts the normal appearance of the skin. In severe cases, this condition may even lead to the disintegration of skin on the soles of the feet.
These signs and symptoms, especially when severe, will often prompt individuals to seek medical care. A healthcare provider will likely rely on these findings to make a proper diagnosis and establish the correct treatment plan.
This is how hyperhidrosis is diagnosed
Excessive sweating can be an embarrassing issue to bring up to a healthcare provider. In many cases, it's never brought up and the individual ends up having to manage the condition on their own (via the Cleveland Clinic). However, by speaking with a provider about their symptoms, many people will find relief.
When making a diagnosis of hyperhidrosis, a healthcare provider will likely want to take a thorough and accurate history. An individual will be asked a series of questions such as how often or when symptoms occur, what parts of the body sweat the most, how much of an impact sweating has on daily activities, if sweating stops during sleep, and if there is a family history of hyperhidrosis.
If a healthcare provider is unable to determine the cause of your excessive sweating, they may order a number of tests which can help make the diagnosis (via Shanghai Chest). One of the most commonly used tests is the starch-iodine test. This test is performed by applying a 2% iodine solution to the most affected areas and allowing it to dry. Powdered starch is then brushed onto the area. As sweat is produced, the brown iodine color will turn a dark purple or black, indicating a positive result.
Medical treatment
Prescription-strength antiperspirants (deodorants) containing aluminum chloride hexahydrate (ACH) are the mainstay of treatment for focal hyperhidrosis, according to Dermatologic Surgery. Three of the most commonly prescribed deodorants include Drysol Extra Strength (20% ACH), Hypercare (15% ACH), and Xerac (6.25% ACH) (via Medscape). Aluminum, which serves as the active ingredient in these deodorants, works by obstructing the sweat ducts in the skin and inducing atrophy of the sweat-producing cells that exist in the sweat glands (per Cedars Sinai). These deodorants are typically applied to dry skin at nighttime and are washed off after waking up, as they may cause some irritation to the skin and eyes.
Another class of drugs used to treat hyperhidrosis includes the anticholinergics (per the Journal of Vascular Surgery). These agents work by blocking the activity of a specific neurotransmitter (acetylcholine), which is responsible for triggering sweat glands to produce and secrete sweat. The most commonly prescribed drug of this class is oxybutynin (Ditropan). Several studies have shown that this medication was very effective and well tolerated when used to control symptoms of hyperhidrosis.
Botox® is another approved treatment for hyperhidrosis, specifically for hyperhidrosis affecting the underarms and palms, according to the Journal of the American Academy of Dermatology and Clinical and Experimental Dermatology. Similar to the anticholinergics, Botox works by blocking the activity of acetylcholine, resulting in decreased sweat production. Several small injections of botox are commonly made over the affected areas, and results can be seen within the first week. The effects of Botox treatment for hyperhidrosis affecting the underarms typically last up to eight months, while treatment for hyperhidrosis of the palms may last as long as 12 months.
Individuals with hyperhidrosis stemming from an abnormal control of emotions might be prescribed beta-blockers (e.g., propranolol) or benzodiazepines (e.g., Xanax, Ativan). These medications may be given prior to a specific stressful situation to reduce the amount of sweating (via U.S. Pharmacist).
Prescription-strength cloth wipes containing glycopyrronium (Qbrexza®) can also be used to reduce underarm sweating (per Skin Therapy Letter). These wipes require daily use, but have been shown in two separate clinical trials to reduce sweat severity and sweat production in patients with hyperhidrosis.
Surgical treatment
Individuals seeking permanent treatment of hyperhidrosis will likely require surgical intervention (per the Cleveland Clinic). Surgery may also be considered in cases where all other medical options have not been successful. Surgeries used to treat hyperhidrosis focus on either removing certain sweat glands or carefully disconnecting nerves responsible for excessive sweating (this process is called sympathectomy).
The most recommended surgery, according to The Society of Thoracic Surgeons, is an endoscopic thoracic sympathectomy (ETS). This surgery is performed by first making two to three small incisions under the arm where excessive sweating occurs (via MedlinePlus). The lung is deflated and a fiber optic camera is introduced to visualize the problematic nerves. The surgeon will then cut the nerves responsible for the excessive sweating, reinflate the lung, and close the incision sites. Unfortunately, one clinical trial showed that 24% of patients who underwent ETS developed sweating in other areas that the surgery didn't treat (compensatory hyperhidrosis), according to The British Journal of Surgery.
Another surgical option, according to the Journal of the American Academy of Dermatology, is the direct excision of sweat glands in the areas most affected by hyperhidrosis. This procedure, called suction-curettage, is similar to liposuction, but instead of pulling out fat, it works by suctioning out the layer of deep skin where the sweat glands are located (per Clinical Trials).
While surgery has the potential to provide long-term or permanent relief for patients suffering from hyperhidrosis, there are always risks that should be discussed between you and your healthcare provider.
Other treatment options for hyperhidrosis
According to the Cleveland Clinic, individuals who do not respond to first-line treatments or surgery could consider certain alternative treatment options. One such alternative treatment is iontophoresis. This method involves the use of a special battery-powered device that emits a low electrical current to the hands and/or feet while they are placed in a shallow tub of water. Iontophoresis sessions typically last 10 to 20 minutes, and can be performed by a healthcare provider or by the patient themselves. The Drionic® iontophoresis devices "have a definite place in the treatment of hyperhidrosis," according to the Journal of the American Academy of Dermatology. Drionic has products specifically designed to treat hyperhidrosis of the hands, feet, and underarms (per Drionic).
Another alternative therapy that can be used to reduce excessive sweating caused by hyperhidrosis is the miraDry® device (via miraDry). This is the only FDA approved device for non-surgical permanent removal of sweat glands from the underarms. It is administered by a healthcare professional and relies on thermal energy (heat) to destroy sweat glands. It requires only one or two treatments, and can provide lifelong relief for patients suffering from hyperhidrosis.
Living with hyperhidrosis
According to the American Journal of Managed Care, hyperhidrosis affects approximately 4.8% of Americans. In particular, it affects mostly younger adults between the ages of 18 and 39. Living with excessive sweating caused by hyperhidrosis can have a tremendous impact on many aspects of daily living. In many cases, healthcare providers may underestimate how social life, emotional and mental health might be affected.
In terms of general lifestyle, individuals with hyperhidrosis often have to pay close attention to their choice of clothing (avoiding bright colors or polyester fabrics), choice of food (avoiding spicy or sour foods), and may even have difficulty with daily tasks such as turning door knobs, opening jars, or holding electronic devices.
When it comes to emotional and mental health, dealing with hyperhidrosis can increase the likelihood that someone develops depression, anxiety, feelings of embarrassment, low self-esteem, and loss of confidence. In some cases, the sweating caused by hyperhidrosis may become severe enough that an individual might need to change careers or even risk getting fired from their job.
The bottom line is that hyperhidrosis can have widespread implications on just about all aspects of life. Healthcare providers should keep this in mind while managing the care of these individuals.
Celebrities affected by the condition
You might be surprised to know that there are actually quite a few celebrities that suffer from hyperhidrosis (via Neat Apparel). Robert Pattinson, one of the stars of the Twilight movie saga, has openly acknowledged that he sweats like a "crazy person" and that he has had several awkward film shoots because of it. While shooting the movie Maps to the Stars, Pattinson admitted that other actors were concerned about his health due to his excessive sweating on set.
Cameron Diaz is another Hollywood superstar with hyperhidrosis. On several occasions, including at a red carpet event for the premier of What to Expect When You're Expecting, Cameron has been spotted with sweat patches under her arms (per Page Six).
Academy and Oscar award winner Halle Berry has been very open about her excessive sweating. During a 2010 appearance on Ellen, she actually revealed her underarm stains to the audience. There is also a possibility that Halle has used Botox to treat her condition, according to Women's Health.
Steve Carell is another well known Hollywood actor who may have hyperhidrosis. While filming episodes of The Office, co-actor Rainn Wilson said that the production crew had to keep the set at a frosty 64 degrees Fahrenheit in order to prevent Steve's clothes from ending up stained (via Looper). Other crew who couldn't stand the cold had to rely on space heaters to keep warm during filming.