Why You May Have Lower Back Pain On Just The Left Side
Most of us have dealt with low back pain at some point in our lives. In fact, the American Association of Neurological Surgeons reports that as many as 85% of people in the U.S. will deal with back pain at one time or another. A study published in the Mayo Clinic Proceedings found that back pain was the third most common reason for doctor's visits in the U.S., behind skin conditions and osteoarthritis. The 2019 National Health Interview Survey, which is conducted by the Centers for Disease Control and Prevention (CDC), found that back pain was the most prevalent kind of pain experienced in the U.S., with 39% of respondents reporting an episode of back pain within the three months prior to taking the survey.
Often, low back pain is felt on both sides of the body. However, according to the Cleveland Clinic, some people experience back pain that only impacts one side of the body. Lower back pain that's only felt on the left side of the body can be caused by a number of different ailments, ranging in severity from normal aches and pains to emergency situations. Here are some of the common reasons why your back pain might be localized to just the left side.
Muscle strain or sprain
The majority of low back pain is caused by damage to the muscles, ligaments, and tendons in the back, according to Dr. Anthony Romero, an orthopedic surgeon at Cottage Health. Though the damage may be caused by a specific injury, it can also be caused by the strains of everyday life. Bending or twisting in just the wrong way, consistently poor posture, and repetitive movements can all damage the tissues in the back, causing low back pain. Orthopedic surgeon and founder of the Alexander Bone & Spine Institute Dr. Lawrence Alexander wrote in Spine Health that low back pain can also be caused by standing or sitting for long periods of time, or even just sleeping in a weird position.
Because the back supports the entire body, it's prone to wear and tear, which makes the muscles, tendons, and ligaments vulnerable to injury. Luckily, low back pain from a strain or sprain will likely heal on its own within a few weeks. You can take some over-the-counter painkillers and rotate ice and heat on the injured area to get some relief (per Cottage Health). It's also important to stay active. Though this seems counterintuitive given the amount of pain you're likely in, keeping your body moving is essential to healing low back injuries.
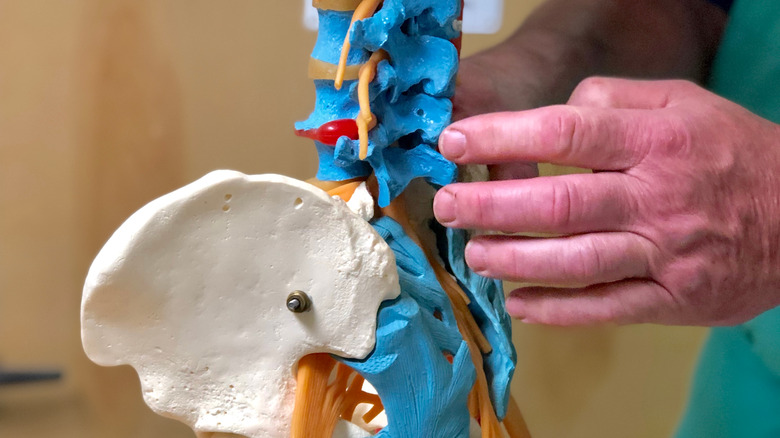
Sciatica
The sciatic nerve, which begins in the low back and continues down the back of each of the legs, is responsible for sensation all the way down the leg to the foot, and for the muscle movements of the back of the leg and the knee. According to Penn Medicine, when the sciatic nerve is injured or gets compressed by the surrounding tissues, it can lead to sciatica. Symptoms of sciatica include pain, numbness, and tingling in the buttocks, low back, leg, and feet. Typically, these symptoms only occur on one side of the body because the sciatic nerve on that side is injured or compressed.
Sciatica is actually a symptom of another medical condition, so it's not really a cause of low back pain. Whatever's causing the injury or compression of the sciatic nerve is the actual culprit. Spinal injuries or conditions like stenosis or a slipped or herniated disc can either directly put pressure on the sciatic nerve or cause inflammation that puts pressure on the sciatic nerve. Fractures in the pelvis, tumors, or muscular injuries, especially to the piriformis in the buttocks, can also cause sciatica.
To treat sciatica, the underlying condition needs to be properly diagnosed and addressed. Sometimes this is as simple as controlling inflammation with over the counter medicines, heat, and ice. If the cause is related to the spine, more intensive treatments may be necessary.
Piriformis syndrome
The piriformis muscle is located in the buttocks and it connects the upper part of the leg to the lower part of the spine, per Harvard Health Publishing. To connect these structures, the piriformis muscle goes through the pelvic bone, right next to the sciatic nerve. When the piriformis muscle is damaged, the swelling can push on the sciatic nerve, causing sciatica. This leads to intense lower back pain that extends through the buttocks and down the back of the leg. Indeed, piriformis syndrome is the underlying cause in about 5% of cases involving leg and buttock pain, according to a review published in The Orthopedic Clinics of North America.
Piriformis syndrome has a few classic symptoms that differentiate it from other forms of low back pain. Pain that gets worse when you're sitting down, especially on one side more than the other, is a hallmark of piriformis syndrome (via Harvard Health Publishing). Pain in the buttocks or hips that radiates to the lower back and down the legs, as well as muscle spasms along the length of the piriformis muscle, also differentiate piriformis syndrome from other forms of low back pain.
Piriformis syndrome can be caused by a direct injury to the piriformis, a misalignment of the spine, prolonged sitting, extreme exercise, and irregular gait. Anti-inflammatories, physical therapy, and stretching are the recommended treatments for piriformis syndrome.
Sacroiliac joint pain
The sacroiliac joints (SI joints) are the joints on either side of the pelvis, right next to the spine, per Sacroiliac Joint Pain. Both of the SI joints are responsible for shifting the weight from the upper body to the lower body when performing movements like going from standing to sitting and walking, explains WebMD. The SI joints aren't actually meant to move that much to do their job. The joints are supported by ligaments and muscles to ensure that they stay in place.
When the SI joint or the muscles and ligaments surrounding it suffer a direct or overuse injury, the structures get inflamed. This inflammation can cause significant lower back pain, typically just on the side that's injured. Damage to the SI joint or the surrounding tissues can happen in several ways, including falls, sports injuries, physical activities that involve a lot of impact such as running, uneven gait, or arthritis. People whose legs are a different lengths are especially prone to SI joint dysfunction because the discrepancy usually impacts gait.
SI joint pain can often be resolved with physical therapy, chiropractic adjustments, and anti-inflammatory medications. When your medical professional determines that the lower back pain in your lower back is due to SI joint pain, they'll discuss which treatments fit your particular situation.
Herniated disc in the lumbar spine
The spinal column is composed of small bones called vertebrae, and between each set of vertebrae there are fluid-filled sacs called discs. Dr. David Wu, an anesthesiologist and pain management specialist, explains on his blog that the discs protect the spine by absorbing the impacts created by the body's movements. Obviously, then, these discs are under a lot of pressure, literally and figuratively. As we age, the discs start to break down, and that degeneration can cause them to slip out of place or rupture. When they do, part of the disc starts to protrude between the vertebrae. This condition is called a herniated disc, or sometimes a slipped disc, according to the Mayo Clinic. Herniated discs are most common in the lower portion of the back, called the lumbar spine.
Herniated discs don't always cause pain, but when the bulging disc pinches a spinal nerve, it can hurt a lot. Typically, the pain is one-sided. The location and type of pain varies depending on where the disc is within the spinal column and whether it's compressing a nerve. If you're feeling pain on the lower left side of your back from a herniated disc, you'll probably feel pain in your buttocks as well. Some people also experience pain in their thigh and calf from a herniated disc. Since the pain is often nerve pain, some people also experience numbness and tingling in their back, buttocks, and leg.
Facet joint disorders
Attached to each vertebrae in the spine are tiny joints called the facet joints. According to a paper published in the medical journal Insights Into Imaging, a set of conditions called facet joint disorders can occur when the facet joints are injured or when they begin to degenerate. Facet joint osteoarthritis, which occurs when the joints degenerate, is the most common facet joint disorder. Research suggests that 10-15% of lower back pain in young people and up to 40% of lower back in older people is due to facet joint syndrome.
Spine Health notes that facet joints anywhere in the spine can be damaged, and sometimes more than one damaged facet joint is contributing to back pain. When facet joints in the lumbar spine — the low back — are impacted, symptoms include a persistent ache in the lower back, stiffness, and referred pain in the abdomen, hips, buttocks, and thighs. Facet joint disorders can also cause problems with posture and limit physical activity. If the damaged facet joint protrudes or shifts and compresses a nerve, sciatica symptoms may arise as well. Though it's possible for joints on both sides to become damaged, therefore causing pain on both sides, if the damage is relegated to one side, the pain will be one-sided as well.
Kidney stones
When urine is composed of too many chemicals and not enough water, the chemicals can start to form hard crystals. According to the National Kidney Foundation, the kidneys usually flush out chemicals before they build up into solid crystals. When they don't, other substances in the body attach themselves to these hard crystals, making them larger, until a kidney stone forms. Kidney stones are more likely to form if someone is chronically dehydrated, exercises excessively, or consumes too many foods containing chemicals that can build up in the urine, particularly oxalates.
Larger kidney stones can cause severe pain along with some other nasty symptoms, per The Iowa Clinic. Most people only experience symptoms from a kidney stone when it's large enough to block off a section of the urinary tract. Since the organs of the urinary tract are all in the middle and lower back, an obstruction anywhere along the urinary tract can cause lower back pain. Often this pain is limited to the affected side.
Back pain often isn't the only sign of a kidney stone, and some people don't have back pain but do have other symptoms. Some people have pain in their abdomen or groin. Nausea, vomiting, fever, and chills are common, as are urinary symptoms like trouble urinating, cloudy urine, or blood in the urine.
Kidney infection
The kidneys, which are primarily responsible for removing waste from the body, are located toward the back of the body, right below the ribcage, one on each side of the spine, per WebMD. Because of their location, the kidneys are sometimes the cause of back pain felt on just one side. Infections of the kidney, which often occur when an infection from the ureter or the bladder progresses to the kidney, are the most common source of kidney pain, notes K Health.
Often only one of the kidneys is fighting an infection, which is why the pain is often felt on just one side — though pain from a kidney infection is also frequently felt in the mid back or upper back (via WebMD). Though pain on the left side of the lower back is more likely a muscle strain than a kidney infection, pain from a kidney infection can be felt in the low back in rare circumstances.
Kidney pain is often experienced as a dull ache that won't go away no matter how you move your body, with intermittent stabbing pain. Back pain will rarely be the only symptom of a kidney infection. Usually the pain will be accompanied by a fever, trouble urinating, and/or cloudy or bloody urine. Sometimes nausea and vomiting also occur.
Urinary tract infection
The urinary system is made up of the kidneys, the bladder, the ureters, and the urethra. According to the Cleveland Clinic, a urinary tract infection, commonly called a UTI, refers to an infection that occurs anywhere in the urinary system. UTIs happen when bacteria enters the urinary system, usually through the urethra. Often the infection stays in the urethra or the ureters, but it can travel all the way up to the bladder or the kidneys.
Typically, UTIs don't cause back pain, according to PlushCare. More common symptoms include pain or burning during urination, feeling the need to urinate frequently, feeling an urgent need to urinate, bloody or cloudy urine, and pressure in the pelvis. However, severe UTIs can cause lower back pain that occurs on one side or across the entire low back because much of the urinary system is located in the mid to low back area.
Low back pain accompanied by more typical UTI symptoms can indicate a serious infection. You should see a doctor as soon as you can because the infection will not resolve without antibiotics. Likewise, your back pain will persist until the infection starts to resolve, usually a few days after starting antibiotics.
Endometriosis
For people with female anatomy, endometriosis may be the culprit behind chronic low back pain, especially if the pain occurs around the same time as the menstrual cycle (via The Femedic). Endometriosis is a chronic reproductive disease in which the lining of the uterus — the endometrium — grows outside of the uterus. The displaced tissue can grow in any part of the body, but most often grows on the organs and tissues surrounding the uterus.
When the endometrium grows on the bones, ligaments, muscles, tendons, or nerves in the lower back, it can cause pain before and during the menstrual cycle. The lower back may also hurt if endometrium grows on the bladder, kidneys, or bowel. Lower back pain from endometriosis may occur on both sides or just one side, depending on where the endometrium is growing. If the endometrium grows on or surrounding the sciatic nerve, endometriosis can also cause endometriosis sciatica, per Seckin MD Endometriosis Center. In rare cases, as described in a case study published in World Neurosurgery, endometriosis can grow directly on the spinal column and the nerves surrounding the spine, causing cyclical nerve pain.
Though lower back pain from endometriosis often starts as cyclical pain — pain that starts a week or so before your period and lasts through your period — it often becomes daily, chronic pain as the condition worsens. Back pain caused by endometriosis is almost always accompanied by pelvic pain, abdominal pain, and heavy, abnormal periods.
Fibroids
Since the uterus is located near the tissues that make up the back, problems with the uterus are often an unexpected cause of lower back pain for people with female anatomy. According to PainTheory, sometimes uterine fibroids can grow large enough to cause lower back pain, which can manifest on one side or both depending on the location and size of the fibroid. Uterine fibroids are benign tumors that grow in and on the uterus, explains Johns Hopkins Medicine. They can develop in the lining of the uterus, within the uterine cavity, or even on the outside of the uterus. Fibroids can be very small, but some can grow up to 20 centimeters. In some cases, fibroid growth can cause the uterus to expand up to ten times its normal size.
Large fibroids can begin to press on the tissues or nerves of the back or pelvis, which can cause low back pain as well as pelvic pain. According to the University of California San Francisco Health, fibroids that develop outside the uterus toward the back side are more likely to cause back pain than fibroids that develop inside the uterus. However, fibroids inside the uterus can cause back pain if they grow large enough. Other symptoms that indicate your back pain may be caused by fibroids are abnormal uterine bleeding, pelvic pain, urinary problems, and pressure in the pelvis or the rectum.
Inflammatory Bowel Disease
Crohn's disease and ulcerative colitis are similar conditions that cause inflammation in different parts of the bowel. According to a study published in the medical journal PLoS One, the umbrella term for these diseases is inflammatory bowel disease (IBD). When people with IBD have flare-ups, 50-70% experience pain as one of their symptoms. Sometimes this pain is caused by bowel inflammation and gastrointestinal distress, but some people also experience pain because of systemic symptoms originating outside the bowel. Researchers and doctors don't quite know what causes pain outside the bowel in people with IBD. Systemic inflammation that spreads through the body definitely plays a part in the pain, however, it doesn't explain why some people with IBD experience pain that isn't caused by inflammation.
The study states that about 38% of people with IBD experience back pain regularly. And according to another study published in the Journal of Crohn's and Colitis, back pain is a chronic issue for 13% of those with IBD. The majority of the back pain reported was localized to the low back. The exact location of the pain appears to be dependent on what part of the digestive system was impacted by the inflammatory bowel disease. In some cases, low back pain is limited to or more prominent on one side, but in others, the pain is consistent across the low back.
Pancreatitis
Inflammation of the pancreas, a small organ in the digestive system that sits behind the stomach, is known as pancreatitis. According to the National Health Service (NHS), acute pancreatitis happens when the pancreas is inflamed for a short period of time. Chronic pancreatitis happens when the pancreas is permanently damaged by long-term or repeated inflammation, usually due to multiple previous cases of acute pancreatitis.
Pancreatitis normally doesn't cause back pain. Severe abdominal pain is the most common symptom of acute and chronic pancreatitis. However, in rare cases, the pain from the abdomen progresses into the left side of the back. As the pancreas accrues more damage from inflammation, episodes of pain can become frequent and severe. Sometimes people have a constant dull ache in their abdomen with intermittent episodes of severe pain.
Acute or chronic pancreatitis probably isn't the cause of left-sided lower back pain for people who've never had pancreatitis before. However, there are always exceptions. A case study published in the Emergency Medicine Journal presented the case of a 63-year-old woman whose only symptom of acute pancreatitis was pain in the left side of her back. Still, there are several causes of left-sided low back pain more likely than pancreatitis.
When should you see your doctor about lower back pain?
Though back pain can seriously impact your day-to-day life and make you extremely uncomfortable, the cause usually isn't an emergency situation. As GoodRx discusses, relatively minor injuries to the tissues in the back are the most common cause of back pain. For the most part, back pain doesn't require a trip to the emergency room.
However, if the pain in the left side of your lower back is accompanied by other symptoms, it might be time to head to urgent care. The most common sign that your back pain is caused by an infection is a fever. So, if you suddenly spike a fever, get someone to take you to the doctor ASAP. If your left-sided lower back pain is severe and you don't get any relief from standing up, sitting down, or lying down in any position, then it's time to get checked out. If both legs start to feel weak or numb or you lose control of your bowel or bladder function, get to an emergency room immediately. This is often an indication of a serious condition.
The bottom line is that back pain on the lower left side all on its own, even if it's pretty bad, usually isn't a sign of an emergency. Often you'll start to feel better with a little rest and remedies you can undertake at home.