Pancreatitis Explained: Causes, Symptoms, And Treatments
On June 28, 2022, Kourtney Kardashian rushed her hubby-of-one-month, Travis Barker, to a local hospital, after which he was subsequently transported via ambulance to Cedars-Sinai Medical Center (per TMZ). Although the paparazzi were on hand to memorialize the melee, few outside Barker's immediate family had any idea what was going on. Needless to say, wild speculation ensued (via Tech ARP). Nor did it help that Barker had tweeted "God save me" earlier that day, or that his daughter, Alabama, had taken to social media to ask for prayers of her own (via Page Six).
It was reported the next day (via the New York Post) that Barker had been complaining of excruciating abdominal pain caused by pancreatitis, which in turn had been set off by a colonoscopy. For the average person, it wasn't clear how a colonoscopy might set off a bout of acute pancreatitis, but Barker shed some light a few days later when he tweeted that prior to the incident, he'd undergone endoscopic removal of a very small polyp (which was presumably discovered during a colonoscopy), and that during the procedure, a pancreatic duct had been damaged. The result, as he put it, was "severe life-threatening pancreatitis."
If the colon polyp/pancreas connection seems a bit abstruse, hang in there. Here's what pancreatitis is — and why a nick to a pancreatic duct might lead to a severe case of it — as well as its causes, symptoms, treatments, and how to prevent it.
What is the pancreas, and what does it do?
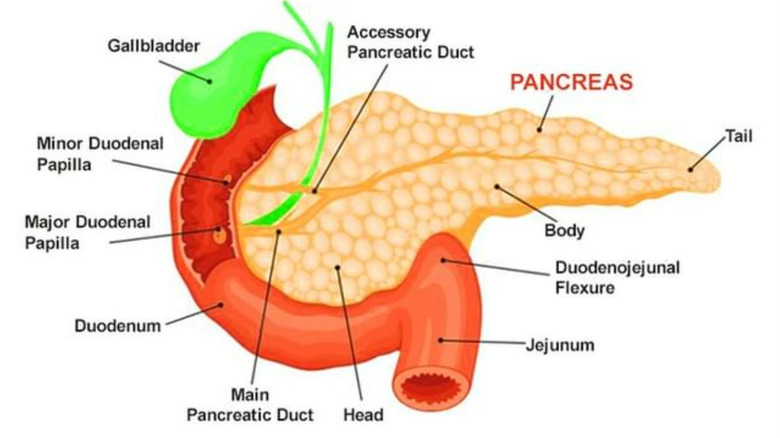
The pancreas is an abdominal organ that can be found in the abdomen's upper left quadrant, per Columbia Surgery. It consists of a head, neck, body, and tail, and is adjacent to the small intestine via the duodenum. The pancreas is an approximately six-inch-long organ that functions as a gland (via the Cleveland Clinic). That means its primary purpose is to secrete enzymes, hormones, and/or other substances.
The pancreas actually secretes both enzymes and hormones, both of which support metabolism via two distinct functions. The first function is to secrete several digestive enzymes that travel via duct to the small intestine to help further break down foods that we've consumed, after the stomach has done its work and before the digested contents reach the large intestine for the grand finale. These enzymes include lipases (which helps break down fats), proteases (which helps break down proteins), and amylases (which helps break down starches).
The second function is to secrete hormones that are essential to the digestive process, including insulin, which helps move digested sugar from the bloodstream to the cells of your body where it provides energy for everything your cells need to do, including remaining alive. There's also glucagon (which tells your liver when to release stored sugar for the purpose of replenishing energy), gastrin (which tells the stomach to make gastric acid for digestive purposes), and amylin (which controls the rate of stomach emptying and feelings of satiety).
What is pancreatitis?
Pancreatitis that comes on suddenly, like what Travis Barker said he's been dealing with since late June (via TMZ), leads to around 300,000 emergency department visits (via Jama) and 275,000 hospital stays, every year in the U.S. (via NIDDK). NIH's StatPearls calls acute pancreatitis the "leading cause of gastrointestinal-related hospitalization" in the U.S. According to the NIDDK, it strikes people at all ages (including children), but it's most common in adults ages 40 and above (per StatPearls).
Pancreatitis refers to an inflammation of the pancreas, which occurs when the enzymes secreted by the pancreas for digestive purposes become active before they have a chance to drain from the pancreas into the small intestine. Aside from seriously impairing digestion and energy metabolism outside the pancreas, those digestive enzymes are essentially digesting the pancreas itself (via MedlinePlus). This irritates the cells of the pancreas, which can ignotes an inflammatory response, including redness, swelling, and sometimes bleeding within the pancreas (via NIDDK).
Acute pancreatitis that never fully resolves or that keeps flaring up over time is known as chronic pancreatitis, per MedStar Health. Both are characterized by inflammation and elevated pancreatic enzymes, but they're considered distinct diseases, according to Difference Between. We will be discussing the differences between acute and chronic pancreatitis below, along with possible causes, symptoms, complications, and treatments, as well as ways to prevent pancreatitis.
What is acute pancreatitis?
According to NHS Inform, acute pancreatitis is an inflammation of the pancreas that develops suddenly, as it did with Travis Barker. The severity with which acute pancreatitis presents can vary widely, as does its prognonsis, per NIH's StatPearls. Mild acute pancreatitis carries a low mortality rate of around 2%. Full recovery may not even require a hospital stay and may be accomplished via nothing more than IV fluids, pancreatic enzyme supplementation, and attention to diet (via AZ Central). At its most severe, however, acute pancreatitis can be fatal.
Severe cases of acute pancreatitis can progress to multiple organ failure within as little as a week, according to MedScape. Severe acute pancreatitis may also involve "acute respiratory distress syndrome, acute renal failure, cardiac depression, hemorrhage, and hypotensive shock." Severe cases of acute pancreatitis account for approximately 20% of all acute pancreatitis cases. In acute pancreatitis patients who progress to multiple organ failure, the mortality rate may be as high as 30%.
From the various sources cited, it appears the greatest challenge acute pancreatitis presents for healthcare providers is how to accurately assess the risk of the potential for serious complications. Factors include age of the patient (more advanced age is associated with more complications and higher mortality, per StatPearls), the presence of relevant comorbidities, and what's actually causing the pancreatic inflammation (if it's caused by duct blockage, that's associated with a worse prognosis than if it's associated with alcoholism, per MedScape).
What is chronic pancreatitis?
Acute pancreatitis may be very painful and/or terrifying, but if treated promptly and appropriately, and assuming the absence of comorbidities, it can resolve within one to two weeks, per Live Healthily. When acute pancreatitis does not fully resolve or when pancreatitis is a recurring problem, it may rise to the level of chronic pancreatitis (via Healthline). This happens in approximately one-third of acute pancreatitis cases, according to a paper published in JGH Open. However, a significant number of chronic pancreatitis cases begin without any acute episode at all. Accordingly, and because chronic pancreatitis is defined by the presence of long-term damage to the pancreas, chronic pancreatitis is regarded by the medical community as a diagnosis separate and apart from acute pancreatitis, which is what Travis Barker has been diagnosed with.
Just as acute pancreatitis can interfere with digestion, so too can chronic pancreatitis, except that the problem does not get resolved. Because the pancreas is critical to the manufacture of insulin — which is critical to blood sugar metabolism — chronic pancreatitis is often associated with type 2 diabetes. In fact, 45% of people with chronic pancreatitis will develop diabetes, according to Healthline. Because chronic pancreatitis is the result of long-term damage to the pancreas, whether caused by repeat bouts with acute pancreatitis or otherwise, it is rare in children and most common in adults over the age of 30 (via the National Pancreas Foundation).
What are the causes of pancreatitis?
Pancreatitis has many possible causes, but the most common are gallstones and heavy alcohol consumption (via Columbia Surgery). Gallstones are often to blame in acute pancreatitis because their presence can block the pancreatic duct, which can cause pancreatic dysfunction and the inflammation that characterizes pancreatitis (per the Mayo Clinic).
Heavy alcohol consumption may be to blame in acute pancreatitis to the extent that the byproducts of alcohol metabolism may be damaging to the acinar cells of the pancreas — i.e., the cells responsible for secreting the pancreatic enzymes that the digestive system needs and that can harm the pancreas when activated while still in the pancreas, per Johns Hopkins Medicine. However, alcohol abuse is more closely associated with chronic pancreatitis because over time, it can lead to permanent scarring and other damage to the pancreas and its ducts.
Other blockages within the pancreas and its ducts may be responsible for some cases of pancreatitis. These include blockages caused by tumors including pancreatic cancers, cysts, genetic malformations, physical trauma and scarring therefrom, calcium deposits caused by elevated blood calcium levels, fatty deposits caused by elevated blood lipids, autoimmune dysfunction, and even the presence of parasites. In as many as 15% of cases of acute pancreatitis, there is no identifiable cause, according to Columbia Surgery. Meanwhile, for up to 25% of cases of chronic pancreatitis, there is no identifiable cause, according to a paper published in Best Practices and Research in Clinical Gastroenterology.
Symptoms of pancreatitis
Travis Barker's first symptom of pancreatitis was severe abdominal pain, per 7NEWS. Abdominal pain — usually felt under the ribcage and always felt in the upper abdomen — is in fact the most common symptom of both acute pancreatitis and chronic pancreatitis, although some people with chronic pancreatitis don't actually present with pain, or at least not consistently, according to NIDDK and Everyday Health.
The pain that is associated with any form of pancreatitis may begin as mild, but it may worsen after eating or drinking or when lying on one's back. Pain can range from mild to debilitating (via Medical News Today), and may be accompanied by fever and malaise, nausea and vomiting, elevated heart rate and pulse, swelling and tenderness in the abdomen, bloating, jaundice, and pain that radiates throughout the back. The way that the pain presents may offer a clue as to the cause of acute pancreatitis (via Everyday Health): When caused by gallstones, the pain tends to be of a stabbing nature, whereas when caused by alcohol use, it tends to be more diffuse.
Because of the long-term damage associated with chronic pancreatitis, symptoms may include weight loss, malnutrition, and changes in bowel movements, including diarrhea and/or oily, clay-colored, and/or foul-smelling stool, per NIDDK. Because chronic pancreatitis interferes with insulin production, a diagnosis of type 2 diabetes is seen in as many as 50% of chronic pancreatitis cases, according to Diabetes.co.uk.
Diagnosis of pancreatitis
If you have stomach pain along with any of the symptoms of acute pancreatitis, you should get yourself evaluated by a medical professional. Severe cases of pancreatitis can quickly become life-threatening, and medical professionals are in a far better position than you as a layperson to determine if you have pancreatitis, its causes, and whether and to what extent it has the propensity to become severe and life-threatening, per a 2021 review of acute pancreatitis in JAMA Network.
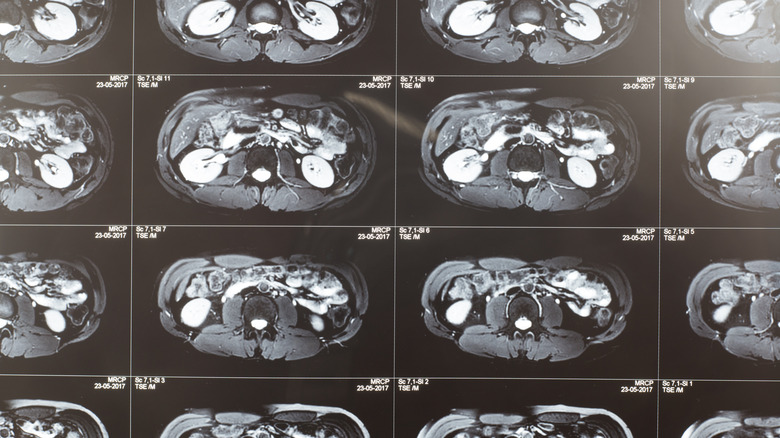
Diagnosis usually begins with a review of your medical history, a physical exam, a discussion of your symptoms and various lab and imaging tests (via NIDDK). Your medical history will probably include your family history of pancreatitis, pancreatic cancer, and biliary disease. Your physical exam will likely include your provider palpating your abdomen to determine the presence and extent of swelling, pain, bloating, tenderness, and any palpable masses. Lab testing will almost always include blood testing to check for elevated pancreatic enzymes, as well as elevated levels of calcium, blood lipids, and white blood cells (which could indicate infection), and elevated kidney and liver enzymes (suggesting dysfunction or failure of either).
When chronic pancreatitis is suspected or when lab testing indicates malnutrition, stool samples may provide your doctor with valuable clues as to how your digestive system is working. Imaging such as CT scanning, MRI, and endoscopic ultrasound may also be used to look for visible inflammation, blockages, and other abnormalities.
Potential complications from acute and chronic pancreatitis
"Acute pancreatitis may be associated with both local and systemic complications," per to a paper published in Gastroenterology. According to NHS, local complications include the development of cysts on the surface of the pancreas known as pseudocysts, which can cause discomfort and become infected. Another complication is pancreatic necrosis due to lost or diminished blood supply to the pancreas that may occur as a result of inflammation.
Although this particular complication is local, it can lead to infection, which can in turn set off sepsis, a systemic reaction to infection in which the "infection-fighting processes turn on the body" (per the Mayo Clinic) and cause organ dysfunction, possible organ failure, and even death. Organ failure is seen in about 20% of all cases of acute pancreatitis, according to the aforementioned paper, but it's not always the result of necrotic infection. In fact, as the authors of that paper note, progression to organ failure is usually observed early relative to diagnosis and is an "important determinant of outcome in acute pancreatitis." Research is ongoing on how to predict and prevent organ failure in acute pancreatitis.
Another complication of acute pancreatitis is chronic pancreatitis, which can occur as a result of damage from acute pancreatitis (per NHS). Since diabetes is a complication in nearly half of all chronic pancreatitis cases (according to Healthline), it may be viewed also as a distant complication from acute pancreatitis.
The relationship between pancreatitis and pancreatic cancer
Since inflammation is associated with — and is known to predispose — the development of cancer in humans, it stands to reason that a diagnosis of pancreatitis can increase the risk that you will one day be diagnosed with pancreatic cancer. In fact, this has long been considered scientific fact, per ScienceDirect. However, the reason for the direct relationship between incidence of pancreatitis and increased risk of pancreatic cancer is not yet fully understood.
For example, some have suggested that the relationship may exist, at least in part, because pancreatic cancer is sometimes initially misdiagnosed as pancreatitis, which means that in some cases, a diagnosis of pancreatitis will, of course, lead to a diagnosis of pancreatic cancer. As Johns Hopkins Pathology points out, a cancerous pancreatic tumor could also be directly responsible for causing a case of acute pancreatitis because it can block access to the pancreatic duct, causing pancreatic enzymes to back up into the pancreas. Others, such as the authors of this 2021 review published in Diseases, frame it slightly differently, seeing acute pancreatitis as an early warning sign of pancreatic cancer while noting that repeat bouts of pancreatitis — i.e., chronic pancreatitis — may be the more significant driver in the development of pancreatic cancer.
Research on the mechanisms by which pancreatic inflammation can lead to pancreatic cancer is ongoing (via MD Anderson Cancer Center).
Treatment for pancreatitis
Pancreatitis treatment differs depending on whether the presentation is acute or chronic. Acute is more emergent because it requires rapid assessment of the various factors that may influence severity and illness progression, per a 2021 review of acute pancreatitis published in JAMA Network. Mild acute pancreatitis symptoms can generally be addressed via IV fluids (to combat dehydration that may result from gastointestinal distress), pain medication, and a slow but persistent re-introduction to eating (mostly clear liquids and balnd foods at first), according to the Mayo Clinic.
In treating acute pancreatitis, the first week or two is particularly critical (via a paper published in World Journal of Gastroenterology), because severe inflammation can lead to organ failure. That can be treated with intensive care, including ventilation and/or dialysis, as needed, per Kindred Hospitals. Once the risk of early organ failure has passed, treatment focuses on preventing necrosis and secondary infection, which could lead to sepsis and late organ failure.
Chronic pancreatitis is treated in the same way in terms of intermittent acute inflammatory flareups, but treatment of chronic pancreatitis must also address the various complications that may be present, including diabetes and its various sequelae, as well as complications arising from long-term malnutrition. Various surgeries may be recommended, including for the purpose of removing scar tissue or damaged pancreatic tissue. As the authors of a 2015 paper in the Indian Journal of Surgery put it, optimal treatment of chronic pancreatitis is multidisciplinary.
How a colonoscopy can lead to acute pancreatitis
A case of acute pancreatitis can be set off by injury or trauma to the pancreas, according to a paper published in the Journal of Trauma. Colonoscopy itself is a "well-tolerated and safe diagnostic procedure, usually performed under conscious sedation," according to Dr Rajesh Gopalakrishna, Clinical Professor, Gastroenterology and Hepatology, Amrita Hospital (via The Indian Express). Nevertheless, "acute pancreatitis is a rare complication after colonoscopy," as Dr. Gopalakrishna pointed out, although it is "more likely to be seen after balloon-assisted enterotomy [sic] of the small bowel." Presumably, this is because the small intestine is in close proximity to the pancreas via the duodenum.
Be that as it may, that a colonoscopy and/or related polypectomy may catalyze a case of acute pancreatitis is accepted, albeit not well-understood, according to the authors of a 2019 case study published in the International Journal of Surgical Case Reports regarding the occurrence of acute pancreatitis in a 53-year-old woman following a colonoscopy. "Hypotheses include mechanical trauma to the pancreas caused by the endoscope particularly at the splenic flexure, over-insufflation of the colon, external abdominal pressure, and transmural colonic burns via electrocautery causing irritation to the pancreas." It is not known to the public at this time precisely what happened during Travis Barker's endoscopic procedure that may have set off his pancreatic inflammation, but perhaps, as more information becomes known, Barker's case will contribute something valuable to this growing body of knowledge.
Things you can do to prevent pancreatitis
One of the direct causes of pancreatitis, both acute and chronic, is excessive alcohol consumption, per Columbia Surgery. In fact, about 70% of all cases of pancreatitis may be due to "chronic heavy alcohol consumption," according to the authors of a paper published in the World Journal of Gastroenterology. It's not clear how excessive or heavy alcohol consumption is defined, but research has shown that consuming four to five servings of alcohol per day is associated with a significantly higher risk of pancreatitis (via the Mayo Clinic).
Accordingly, pancreatitis prevention would logically involve drinking considerably less than that. Since gallstones are another significant cause of pancreatitis, a diet that is supportive of gall bladder health can help manage pancreatitis risk, per Everyday Health. According to the NIDDK, such a diet might include lots of fruits, vegetables, beans, and whole grains while cutting back sugar, refined carbohydrates, fried foods, and unhealthy fats.
Prevention can also involve cutting out cigarette smoking since, as Mayo Clinic points out, smokers are at three times of a higher risk of developing chronic pancreatitis than non-smokers, whereas quitting smoking can cut that risk in half. Since obesity is correlated with a higher risk of pancreatitis, weight reduction and maintenance can help, as can avoiding type 2 diabetes, which is also correlated with a higher risk of pancreatitis. Finally, a 2022 study published in Nutrients suggests that getting adequate vitamin D can help lower the risk of pancreatitis.