Things That Are Making Your Athlete's Foot Worse
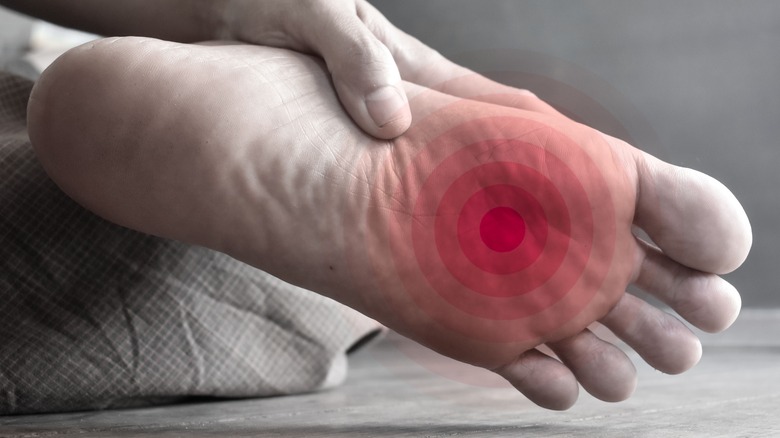
Athlete's foot, also known as tinea pedis or ringworm of the foot, is a fungal infection that affects the soles of the feet (via Medical News Today). It makes the affected site red, dry, scaly, flaky, or cracked. The area might also smell, itch, sting, or burn. Athlete's foot is caused by a type of fungus known as a dermatophyte, which multiplies and causes infections in dark, moist, and warm places. They spread from person to person through contact with a contaminated surface or infected person (or by touching their skin, socks, shoes, bedsheets, or towels).
Athlete's foot is common in developed countries, and its incidence is on the rise due to urbanization and changes in the type of recreational activities people perform. It is estimated that at any given time, 25% of people in the U.S. may have athlete's foot (via an article published in the Journal of Drugs in Dermatology). Moreover, an estimated 70% of people will have athlete's foot at some point in their lives (per Medical News Today).
Athlete's foot affects both children and adults, but it's most common among men. It's also possible for a person to have a hidden infection with no symptoms. This is usually an early stage of infection. Although athlete's foot is the most common fungal infection caused by dermatophytes, these dermatophytes can also infect your skin elsewhere, as well as your hair or nails.
Is what you have athlete's foot?
There are other skin conditions like eczema, psoriasis, or dermatitis that can affect the feet. It's important to be sure that what you have is athlete's foot, so you can treat it properly. The fungi that cause athlete's foot typically affect the superficial skin on the sole of the feet. This is because the fungi degrade and use the skin's keratin to grow (per Medical News Today). The skin on the sole of the feet also lacks sebaceous glands which secrete antimicrobial substances, which aids the growth of these fungi (via an article published in the Journal of Drugs in Dermatology).
Athlete's foot can appear in four patterns (via WebMD). The most common, interdigital tinea pedis, affects the web spaces between your toes (especially between the third, fourth, and fifth toes). Next, the moccasin type makes the sole of one or both feet thick, dry, scaly, or cracked. This type often goes unnoticed or has subtle symptoms. If athlete's foot appears with painful, itchy, or red blisters, it's vesicular tinea pedis. Ulcerative tinea pedis is rare; it often comes from the worsening of interdigital tinea pedis, resulting in ulcers and erosions (deep sores) in the skin of the affected web spaces. Most people with this type of athlete's foot either have diabetes, peripheral vascular disease, or a weak immune system (per the Journal of Drugs in Dermatology). Whatever type of athlete's foot you may have, there are things that can worsen your symptoms.
Not being proactive about treatment
You can't simply sit back and hope your athlete's foot will go away with time. You need to treat it. Over-the-counter (OTC) topical antifungal medications are usually good at clearing athlete's foot (via Patient). There are several types and brands of these antifungal medications. Meant to be applied on the skin, they come as creams, sprays, powders, or fluids. Most products contain either clotrimazole, econazole, miconazole, ketoconazole, terbinafine, tolnaftate, or undecenoic acid. Your symptoms might clear up quickly once you use these products. But you shouldn't quit the treatment prematurely, as the fungi might still linger on your skin to cause another infection. It's important that you use antifungal treatments for as long as you're advised to.
There are some home remedy options that may be effective or offer some relief. For example, applying tea tree oil, bitter orange oil, or sunflower oil on the affected area might help you get rid of your symptoms (via WebMD). You can also try out gels made from ajoene (from garlic) and Sosa creams. Regular foot soaks with green tea or vinegar can also help with athlete's foot. While any of these remedies may offer some relief, they may not be completely effective at killing the fungi that cause athlete's foot. However, they're still worth trying in addition to using antifungal medications. Just remember to do a patch test to find out if you have a skin reaction to any home remedy you try out.
Using the wrong medication
There are many over-the-counter creams or other forms of topical treatments available for different skin problems, but only an antifungal cream will truly work to get rid of athlete's foot. With that said, antifungal products made from nystatin are not effective against athlete's foot or other tinea infections (per the American Academy of Family Physicians). Nystatin products are effective against candidiasis of the skin, another fungal infection, but tinea-causing dermatophytes are resistant to nystatin.
Using creams containing steroids like hydrocortisone can make your athlete's foot worse, warns the Centers for Disease Control. Steroids are typically the go-to choice for rashes, because they help with redness and itching, even those caused by fungal infections (at least, initially). However, they can lead to more severe redness and itching, since they weaken the skin's immune defenses and allow the spread of the infection. In rare cases, they can even cause infections of deeper structures.
To make things worse, steroid creams alter the appearance of fungal infections, making it hard for medical professionals to be sure that what you have is athlete's foot if you report to a clinic. So, it's best to avoid using steroids for athlete's foot. Some antifungal creams contain steroids, so make sure to ask about this or check the label before using them to treat athlete's foot.
Not seeking medical help when you should
In most cases, athlete's foot will clear up when you use an OTC antifungal product. But if your symptoms get worse or don't improve a few days after antifungal treatment, you should seek help from your health provider (via Healthline).
You should also let your provider know if your athlete's foot keeps coming back. If you have diabetes or any other condition that suppresses your immune system or affects your circulation, you should let your doctor know as soon as you notice symptoms of athlete's foot. It's also worth reporting to a healthcare provider for proactive treatment if you don't want to inadvertently infect others around you (via Balance Health).
Your doctor will diagnose you, and may prescribe topical antifungal medications or antifungal tablets like terbinafine or itraconazole. Tablets are usually given when your athlete's foot is severe or widespread, or if it doesn't respond to topical treatments. However, children, pregnant women, breastfeeding mothers, people with liver disease, and people on certain medications are not prescribed antifungal tablets (via Patient).
Not keeping your feet clean, dry, and naked
Pay extra attention to your foot hygiene when you have athlete's foot. Apart from ensuring that your feet are reasonably clean by washing them at least twice a day, you should try to keep them dry and away from the confinements of socks and covered shoes most of the time.
As fungi enjoy and flourish in warm, moist, and dark places, try to go barefoot or wear open shoes or sandals as much as you can. Note, however, that going barefoot encourages the spread of athlete's foot by contaminating your floors, so you clean your floors properly. Letting your feet breathe prevents you from holding sweat (moisture) close to your skin. With about 250,000 sweat glands, your feet can produce about half a pint of sweat each day. Not letting all that sweat dry out (especially if you have sweaty feet) encourages fungal growth. You should also dry your feet thoroughly every time you wash them to reduce moisture (via Footwear News). Once your athlete's foot starts healing, you can lightly but thoroughly scrub off dead skin while showering. Living fungi, which can reinfect you, remain in dead skin, explains family medicine physician Frederick Hass (via Prevention).
If you need to cover your feet, change your socks frequently (or at least don't repeat a dirty pair) and let covered shoes dry properly before you wear them again. You can also treat your shoes with antifungal powders before wearing them.
Wearing the wrong socks or footwear
Ideally, it's best to avoid wearing socks if you have athlete's foot, as they foster the growth of fungi by making your feet warm, dark, and sweaty. But in case you can't do without a pair of socks, it's best you wear ones that won't worsen your condition.
Per Creepers Socks, use lightweight and breathable socks that allow airflow. You should also go for socks that are fast-drying, taking moisture away from your skin by absorbing it into the fabric (e.g., merino wool socks). It's also best you go for toe socks, as they reduce moistness between the toes. Cotton socks tend to absorb moisture well, but become moist on the skin, making them unadvisable for people with athlete's foot.
As for what shoes to wear, Family Footwear Center advises that you go for breathable shoes with uppers made of non-synthetic materials like breathable mesh, leather, or canvas. You should also wear work boots that have moisture-wicking linings. And if you must wear waterproof shoes, go for styles with internal waterproof membranes that seal out external water but allow evaporation of sweat. Avoid tight shoes; they hold in heat and moisture, and don't leave much freedom to your toes. Shoes that are breathable and have extra room in the toe box allow moisture to evaporate easily. They also give room for foot swelling that comes in the summer and help with insulation in winter.
Using moisturizers or lotions
Normally, you use moisturizers, lotion, or petroleum jelly to hydrate your skin. These products are important because they prevent skin dryness or hardness and maintain the skin's glow. However, they tend to increase the moisture around your feet and make them sweat. And this is even worse if your feet are naturally sweaty.
A rule of thumb when dealing with athlete's foot is that your feet need to remain dry. The affected foot might crack, peel, or look unpleasant. So if you think that it's a good idea to care for your beat-up skin with moisturizers, lotions, or petroleum jelly, don't be tempted to do so. You'll just be applying excess and unnecessary moisture to your foot and fostering the growth of the offending fungus.
Your antifungal cream is likely the only product that would offer you any actual benefit against your athlete's foot, so use them judiciously and skip anything else (via Prevention).
Exposing your feet to even more fungi
When treating athlete's foot, you want to get rid of your fungal infection and not expose your feet to more fungi; thus, measures used to prevent the condition still apply. Avoid walking barefoot in moist places like public bathrooms, saunas, swimming pool areas, or locker rooms (via MedicineNet). Instead, wear open shoes like flip-flops, sauna slippers, or shower shoes. Also, maintain hygiene by cleaning and disinfecting shoes and socks, not sharing shoes, and clipping toenails. Taking these measures not only manages your condition, but will also help prevent anyone close to you from getting infected. Should anyone else get infected, encourage them to get treatment.
While trying to limit your exposure to fungi, you should also be vigilant about your belongings. The spores of the fungi that cause athlete's foot don't land on the floor alone; they can get on your clothes, shoes, gym outfits, bedsheets and towels. So, isolate any item you think might be infected and keep them away from non-infected ones. You should also disinfect affected items properly and frequently by using hot water or disinfectants.
Scratching or picking at the affected site
Because athlete's foot can be itchy and can produce scales on the skin, you might have the urge to scratch or pick at the affected area. Scratching may feel good temporarily, but it won't get rid of the itch — and if you scratch or pick at the infected skin, you might just end up injuring yourself or worsening your discomfort.
Additionally, you can pick up spores of fungi on your fingers when you scratch or pick at the affected skin. Remember, these fungi cause skin infections — and this is not restricted to the soles of your feet. For instance, your hands can also have this fungal infection (via WebMD). You can also unknowingly spread the infection to other parts of your body (such as your groin, nails, or underarms) if you touch them after scratching your feet. If the itchiness is intense, you can soak your feet in cool water to get some relief. Afterwards, dry your feet properly with a towel or blow dryer.
Getting a pedicure
Your feet may not look or feel as pretty as you'd like them to be when you have athlete's foot. This may make you want to get a pedicure to improve their appearance, even by just a bit — but you really, really shouldn't.
For starters, the procedure can hurt you even further if it's abrasive. If you use nail polish on your toes, you can trap moisture and fungi close to your toenails, which may lead to a fungal infection of your toenails, or onychomycosis (via UpToDate). You should also skip using foot peels to exfoliate your feet, as well as other harsh treatments. While they may be effective in getting rid of dry or dead skin, they can irritate and aggravate sites affected by athlete's foot, making your condition worse (via Footwear News).
Generally, it's not a good idea to get a pedicure when you have athlete's foot because you can contribute to the spread of the condition. Most good nail salons will turn you away immediately when they notice signs of the condition, anyway. It's best to set your appointment after you've successfully treated your athlete's foot.
You could have a secondary bacterial infection or cellulitis
A secondary bacterial infection and cellulitis are possible complications of poorly managed athlete's foot, which can make your condition appear worse. Fungal skin infections are superficial, but if your skin breaks or is severely damaged, bacteria (e.g., Staphylococci or Streptococci) can get in and cause a secondary infection (via Wounds Middle East). Secondary bacterial infections can be diagnosed and treated by your healthcare provider.
If bacteria get in through cracked or damaged skin, they can cause a more serious and painful infection known as cellulitis (via Healthline). It is not localized to the skin, as it can affect structures under the skin and spread to the lymph nodes and bloodstream. The affected area becomes hot, tender, swollen, and discolored, and may produce pus. You might also experience fever, nausea, chills, fatigue, dizziness, muscle ache, or increased sweating. Prompt treatment of cellulitis is necessary, because the condition can be life-threatening. Hence, you should report to your healthcare provider if you notice any of these symptoms. Treatment is usually with antibiotics and pain relievers.