What Your Urine Color Can Tell You About Your Health
Our urine can tell us a lot about our health. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) explains that urine is formed by (and travels through) the urinary system, which is made up of the kidneys, ureters, bladder, and urethra. There are nerves in the bladder that help our brain recognize when the bladder is full. Muscles in between the bladder and urethra called sphincters allow us to hold or let go of our urine.
Urine is a byproduct of blood that has undergone filtration (per Johns Hopkins Medicine). When blood passes through the kidneys and ureters, important substances like sodium, potassium, and water are regulated and kept in balance. At the same time, waste products like urea are filtered out in the form of urine. From the kidneys and ureters, urine collects into the bladder, where it stays until the bladder gets full. Once full, the brain will instruct the bladder to constrict and the sphincters to relax, allowing urine to be squeezed out through the urethra and out of the body.
Normal urine is usually clear and pale yellow in color, does not have a strong smell, and is not foamy or frothy (via WebMD). If you recently noticed a change in your urine, it may be a good idea to let your doctor know. The underlying cause may be harmless in some cases, but other times it can be a sign that something serious is going on.
You may be drinking too much or not enough water
The amount of urine your body makes depends on how much water you drink. The more water you drink, the more urine you produce and excrete, and vice versa. According to Harvard, women should drink around 11 cups of water per day, and men should drink around 16 cups. Being adequately hydrated is important to make sure that your body functions well.
Dehydration occurs when you do not have enough fluid in your body (per MedlinePlus). This can happen if you are not drinking enough, or if you are losing a lot of fluid (e.g., vomiting, diarrhea, excessive sweating). The more dehydrated you are, the more concentrated your urine is. This typically manifests as darker-colored urine or having no urine at all. When the latter happens, seek help immediately, as this is a sign of severe dehydration which can be life-threatening.
On the other hand, there is also such a thing as having too much fluid in the body (i.e., overhydration). This is typically harmless in healthy people, because the body does a good job of excreting excess water (via Merck Manual). A healthy person would have to be drinking at least six gallons of water a day every day for them to overwhelm their kidneys. On the other hand, overhydration in people with underlying conditions like heart failure and chronic kidney disease can be deadly. A good indicator of overhydration is peeing out colorless urine.
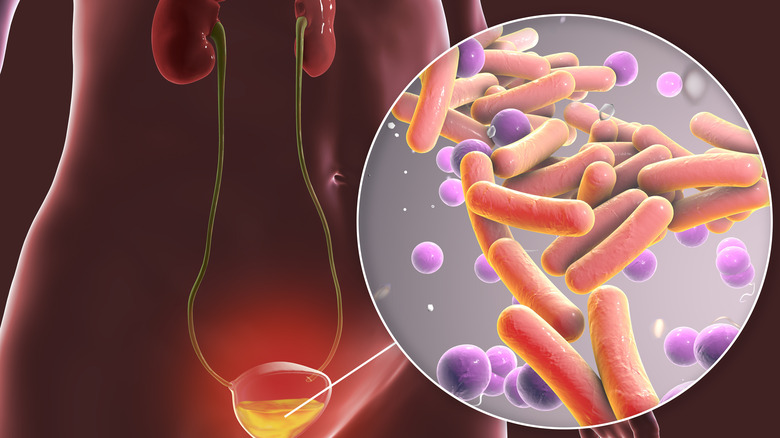
You may have an infection in your urinary tract
All parts of your urinary system can become infected. Cystitis (bladder), pyelonephritis (kidney), and urethritis (urethra) are collectively known as urinary tract infections (UTIs). Urine is typically sterile, but there are certain scenarios where bacteria from outside the body find their way inside and cause problems (via StatPearls).
UTIs are very common. Females are especially susceptible because their urethras are shorter and are in very close proximity to the vagina and anus, which are the primary sources of UTI-causing bacteria (per Cleveland Clinic). You may have a UTI if you are urinating more frequently, have pain or pressure in your lower back or pelvic area, experience pain during urination, have a strong urge to urinate, notice blood in your urine, develop turbid urine, and/or have strong- or foul-smelling urine.
Blood in the urine can look like different things. You may have blood in your urine if the color you see in your toilet bowl is pink, red, brown, or black (via Arkansas Urology). It is important to note, however, that you can still have a UTI even if you do not have blood in your urine. This is especially true if you only have an infection in your urethra and not in your bladder or kidneys (per StatPearls).
Interestingly, although there are several types of bacteria that can cause UTIs, Healthline states that if you get an infection specifically from Pseudomonas aeruginosa, your urine can also turn green, blue, or purple.
Kidney stones may be to blame
The Urology Care Foundation explains that kidney stones can form when there is a high concentration of certain minerals and salts in your urine. When a stone forms, it can remain small and spontaneously pass together with urine without causing any symptoms, or it can progressively grow larger and cause obstruction and other problems somewhere along the urinary tract. The most common type of kidney stones are calcium stones. They typically form in people who have high levels of calcium in their blood, eat too much salt, or do not drink enough water. Other types include uric acid stones (typically seen in people with acidic urine), struvite stones (common in people with chronic UTIs), and cystine stones (caused by an inherited condition).
If you have kidney stones, you may experience sharp pain on your lower back, lower abdomen, or groin, which is typically localized to one side. Similar to UTIs, you may also have the urge to urinate frequently, feel pain when you urinate, see blood in your urine (i.e., pink, red, brown, or black urine), and pass urine that is cloudy and foul-smelling (per Medical News Today). You may also develop fever, chills, nausea, and vomiting. If your kidney stone is small enough (less than 4 millimeters), you may be able to pass it without taking any medications or undergoing any procedures. Otherwise, your doctor may have to perform surgery to break down the stone into smaller pieces, or remove it in one piece.
You may have injury in your kidneys
StatPearls explains that glomerulonephritis is an umbrella term used to refer to a group of disorders that causes damage to one or several parts of the kidneys. Some diseases originate from the kidneys themselves, while others begin elsewhere in the body and subsequently cause damage in the kidneys. In general, they can be classified into two groups: nephritic syndrome and nephrotic syndrome. People with nephritic syndrome have low levels of protein in their urine, trace amounts of blood in the urine, and hypertension. On the other hand, people with nephrotic syndrome have high levels of protein in their urine and swelling throughout their body (due to fluid retention). Both nephritic and nephrotic syndrome can lead to acute or chronic kidney failure (per Amboss).
If you have glomerulonephritis, your urine may be pink, red, or brown because of the presence of blood; or it may be turbid and foamy or bubbly because of the high amounts of protein. Additionally, if you start experiencing muscle cramps at night, fatigue, lack of appetite, trouble sleeping, dry and itchy skin, nausea, and vomiting, this may be an indication that your kidneys are failing, and you should work with your doctor or a referred specialist to help control your condition as soon as possible (via the National Kidney Foundation).
Unfortunately, most types of glomerulonephritis are progressive diseases, which means that you have to make regular visits to your doctor to ensure that your condition is well-managed to avoid further complications.
Your liver may be experiencing some problems
The liver is a large solid organ located in the upper right side of your abdomen. It has multiple roles in the body, which includes metabolism of fat and proteins, storage of vitamins and minerals, filtration of blood, and production of bile and albumin (via Medical News Today).
There are many ways the liver can get damaged. In some cases, problems can arise because of a person's genetics (e.g., hemochromatosis, Wilson's disease) or an autoimmune condition (e.g., primary biliary cholangitis, primary sclerosing cholangitis). However, most of the time they occur due to an acquired disease such as infections (e.g., hepatitis), alcohol abuse, fat accumulation, and several cancers (per Mayo Clinic).
When there is disease in the liver, there can be an interruption in the flow of bile from the liver to the gallbladder. This leads to a condition called cholestasis (via Merck Manual). Under normal circumstances, bile helps the body digest fats and get rid of bilirubin (a pigment formed from the breakdown of old or diseased red blood cells) via the stool. Bilirubin is largely responsible for the brownish color of stool. Therefore, in people with cholestasis, not only is bile flow interrupted, but bilirubin accumulates in the blood as well. Very little or no bilirubin gets excreted in the stool, leading to stools that are pale, white, or very light brown (i.e., acholic stools). The excess bilirubin is instead filtered out in the kidneys, which consequently turns urine dark or tea-colored.
You may have inherited a condition called porphyria
Porphyria is a group of rare, inherited disorders caused by a defect in one of the steps involved in the production of heme (per the American Porphyria Foundation). Heme is found in hemoglobin present in red blood cells, and it is responsible for holding on to oxygen from the lungs and transporting it to the rest of the body. There are eight steps in the process of creating heme, and an abnormality in any one of these steps can lead to porphyria.
When any process gets disrupted, there is an accumulation of the products upstream from where the problem is, and a decreased or absent number of products downstream. In porphyria, the same thing happens where there is an accumulation of porphyrins and/or its precursors in the body, which can cause several problems in the skin, nervous system, liver, and other organs (via the NIDDK).
According to Drugs.com, there are three main types of porphyria: acute, cutaneous, and mixed. Acute porphyrias can cause severe abdominal pain, muscle weakness, numbness, depression, agitation, hallucinations, nausea, vomiting, difficulty breathing, fast heartbeat, high blood pressure, trouble sleeping, and constipation. It can also turn your pee dark or red because of the presence of heme precursors excreted by the kidneys. On the other hand, people with cutaneous porphyria mostly experience skin symptoms such as increased sensitivity to sunlight, itchiness, hyperpigmentation, and increased hair growth. Mixed porphyrias present with a combination of acute and cutaneous symptoms.
It could be other genetic disorders
Alkaptonuria is caused by a deficiency in an enzyme involved in the process of breaking down the amino acid tyrosine (per GeneReviews). It is a very unique condition in that people with this disease will often have dark-colored urine and/or urine that darkens (and sometimes looks black) when it is exposed to air or an alkaline solution for a certain period of time. Other unique features of people who have alkaptonuria include ochronosis, which is blue-black pigmentation of connective tissues such as the white part of the eyes, ears, and tendons.
Alport syndrome is another inherited condition that can alter the color of urine (via StatPearls). Because it is considered a nephritic syndrome, people with this disease often have blood in their urine, making it appear reddish or pinkish. People may also develop hearing loss, vision problems, difficulty swallowing, chest and abdominal pain, vomiting, recurrent chest colds, and shortness of breath.
A condition called blue diaper syndrome (aka familial hypercalcemia) occurs in people who inherit a mutation that prevents the intestines from efficiently breaking down the amino acid tryptophan (per iCliniq). This leads to an accumulation of indican and similar substances, which get excreted from the body through the kidneys. When exposed to air, these compounds get converted to indigo pigments, causing urine to turn bluish. Other symptoms include gut problems (e.g., constipation, appetite loss, vomiting), eye problems, irritability, and failure to appropriately grow and gain weight.
It could be your prostate
The prostate gland is located just below the bladder of males, and it is responsible for several roles that involve reproduction. It produces prostatic fluid, which is an integral part of semen, and it helps create the hormone dihydrotestosterone (DHT) from testosterone, which allows males to develop secondary sexual features like facial hair (via Medical News Today). The prostate also closes the urethra during ejaculation to prevent urine from coming out together with semen.
A common disease of the prostate is benign prostatic hyperplasia (BPH) or enlarged prostate. It is still unclear why this happens, but it is more common in people who are older, have heart disease, are diabetic, are obese, and have close relatives with BPH. Some of the usual symptoms of BPH include urinating more frequently, feeling the urge to urinate often, difficulty with initiating peeing, disrupted and weak urine flow, and feeling like the bladder is not completely empty after peeing. Less frequently, people with BPH may experience urinary tract infections (UTIs), blood in the urine, and inability to urinate (per Mayo Clinic).
Johns Hopkins Medicine adds that although men who have blood in their urine should be suspected of having BPH, most of them will not experience this symptom. Diagnosis of BPH usually involves a thorough history and physical examination, which includes a digital rectal exam (DRE) where a doctor inserts a lubricated gloved finger into the rectum to evaluate the size, shape, and consistency of the prostate gland.
You may have problems with your bowels
According to Baptist Health, bowel problems such as Crohn's disease and diverticulitis can cause urine to appear cloudy and develop foams or bubbles. The presence of air in the urine is called pneumaturia, and it is often seen in people with urinary tract infections (UTIs) or people who have an abnormal connection between their colon and bladder (i.e., enterovesical fistula), per Healthline. Pneumaturia can be accompanied by other symptoms like pain during urination, trouble peeing, and feeling the urge to urinate often. Medscape states that people with enterovesical fistulas may have had them since birth (congenital) or acquired them later on in life as a complication from inflammation, surgery, and/or cancer.
Crohn's disease is a type of inflammatory bowel disease (IBD). Multiple sores form on the wall of the intestines, and as the disease progresses, these sores can tunnel their way into another bowel segment, the bladder wall, the vagina, or the surface of the skin and cause a fistula (per WebMD). Similarly, diverticulitis occurs when pouches in the intestinal wall called diverticula become infected or inflamed (via WebMD). It is common in people who smoke, are older than 40 years old, are overweight, are sedentary, have a diet consisting mostly of fat and red meat, and do not consume enough fiber. Medications like steroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and opioids can also predispose someone to developing diverticulitis.
If it progresses and is left untreated, complications can occur such as the development of abscesses, perforation, fistulas, and strictures.
There may be a tumor in your bladder or kidneys
According to the American Cancer Society, one of the earliest symptoms of bladder cancer is the presence of blood in the urine. This can be seen as red, pink, or orange urine. However, blood will not always be present, and sometimes the amount of blood can be so little that it can only be detected using laboratory tests. Because of this, doctors often check for bladder cancer even if you only see blood in your urine once. Other possible symptoms such as frequent urination, urge to urinate, waking up at night to urinate, and having a weak urinary stream are nonspecific and can also be caused by a variety of other conditions like UTIs, stones in the bladder, enlarged prostate, and overactive bladder.
Similar to bladder cancer, kidney cancer can also cause blood to appear in the urine. Other symptoms can include persistent back or side pain, loss of appetite, unintentional weight loss, and unusual tiredness. These symptoms do not typically appear until the cancer has progressed to later stages, and screening is not typically done unless a person is at a very high risk of developing kidney cancer (via Cancer.net). Some of the things you can do to lower your risk of developing kidney cancer include not smoking, making sure your blood pressure is under control, and maintaining a healthy weight (per Mayo Clinic).
You may have been exposed to too much lead or mercury
The Occupational Safety and Health Administration (OSHA) states that lead and mercury are heavy metals that are considered toxic to our health. Lead overexposure is common in construction work, smelting industries, repair shops for radiators, and firing ranges; meanwhile, mercury overexposure is common in mining and related industries.
These toxic metals are not just exclusively found in the places and occupational environments mentioned above. According to Cleveland Clinic, lead coming from our water pipes can contaminate our water supply, and we can also be exposed to lead found in batteries, paint, and gasoline. On the other hand, mercury is also present in lightbulbs, dental fillings, batteries, seafood, and antiseptics. We can absorb lead and mercury through our skin, inhale them through the air we breathe, and ingest them from the food that we eat and drink.
Nonspecific symptoms of heavy metal toxicity include nausea, vomiting, abdominal pain, diarrhea, shortness of breath, "pins and needles" on the hands and feet, chills, and weakness. Lead poisoning can additionally cause headaches, irritability, aggressiveness, high blood pressure, appetite loss, constipation, sleep problems, and developmental problems in children. Mercury poisoning can lead to muscle weakness, impaired coordination, nerve damage, as well as vision, hearing, and speech problems (per Healthline). The University of California San Diego (UCSD) Health adds that lead and mercury poisoning can also cause urine to turn red or have a pinkish hue, which usually means that there is blood.
You may be exercising too much
Although health experts always recommend exercising to stay healthy and protect yourself from chronic illnesses, there is such a thing as too much exercise. When you overwork your muscles beyond their capabilities, they respond negatively by breaking down and releasing proteins and electrolytes into your circulation. In high numbers, these substances can be very toxic and deadly to your organs. This condition is called rhabdomyolysis (per the Centers for Disease Control and Prevention).
Rhabdomyolysis can also occur after intense or prolonged exposure to heat (e.g., firefighters, smelters, outdoor workers) and crush injuries (e.g., falls, car accidents). Factors that can increase a person's risk of developing rhabdomyolysis include illicit drug use (e.g., cocaine), stimulant use, excessive amounts of alcohol or caffeine, medications and supplements such as antibiotics, antidepressants, and creatine, infections (e.g., HIV, EBV, influenza), and underlying health problems like uncontrolled diabetes and sickle cell disease.
According to the MSD Manual, rhabdomyolysis is a life-threatening medical emergency that can cause the kidneys to fail rapidly. Sometimes, multiple blood clots may also form throughout the body and impair blood flow. A person may feel weakness, and muscle pain in their shoulders, lower back, thighs, or calves; and their urine may look similar to tea (reddish-brown).
To avoid rhabdomyolysis, Harvard Health suggests drinking plenty of water, and avoiding drugs and substances that can increase your risk. Listen to your body and take it easy when executing exercise routines, especially if it is your first time doing so.
Your medications may be the culprit
All of us would agree that taking medications is not exactly an enjoyable thing to do. Not only do you have to actively remember when to take them, you also have to worry about the possible side effects you may get from them. It can also get tricky sometimes to determine if what you are experiencing is caused by medications or something else entirely.
Aside from the usual side effects of medications (e.g., nausea, stomach upset, drowsiness), certain drugs can actually turn urine into all kinds of different colors. According to GoodRx Health, isoniazid, sulfasalazine, and phenazopyridine can turn urine orange. Interestingly, the sweat and tears of people taking sulfasalazine can also become orange. Medications and supplements that can turn urine brown include iron tablets, senna, metronidazole, nitrofurantoin, levodopa, phenytoin, chloroquine, and primaquine. Walrus.com adds that certain medications can also turn urine red. These include heparin, rifampin, methyldopa, phenytoin, doxorubicin, and daunorubicin.
Surprisingly, there are also medications that can turn your urine blue or green. This can be a shocking thing to see when you go to the bathroom, but do not panic. Medications such as amitriptyline, cimetidine, indomethacin, metoclopramide, promethazine, propofol, and methocarbamol can all cause this (per GoodRx Health). Methylene blue, a dye used in several scans and procedures, may also be the cause. If you are concerned, however, it will not hurt to speak with your healthcare provider.
It could be something you ate
We are surrounded by thousands upon thousands of different food choices, both natural and artificial. They come in all shapes, sizes, textures, and colors. Although the color of our stool and urine do not normally follow the color of the food that we eat or drink (which actually makes sense if it did), there are some exceptions to this.
According to MedicineNet, certain food dyes can transform our urine into all kinds of colors, including orange, blue, and green. Additionally, beets, blueberries, and rhubarb can sometimes turn urine red or pink. The Urology Care Foundation adds that eating a lot of asparagus or black licorice can cause your urine to turn all kinds of shades of green. Also, it is well known that eating large amounts of carrots can cause your skin to look orange — but interestingly, they can turn your urine orange as well (via Cleveland Clinic).
Although there is not much to worry about when food or medications change the color of your urine, there are several causes of urine color changes that absolutely need medical attention. If you see an unusual color in your toilet and you are not experiencing anything new or unusual, try to recall what you ate recently or what medications you are taking, and see if any one of those could potentially explain the change in your urine color. As always, it is always best to consult with your doctor if you notice anything different with regard to your health.