Mistakes You Didn't Know You Were Making With Medication
When we're not as well as we'd like to be, medication can often be a stopgap. With modern medicine now providing remedies for a huge amount of health conditions, more than half of all Americans take at least one prescription drug, according to the Health Policy Institute. Additionally, more than 81% of adults look to over-the-counter medicines as "a first response to minor ailments," per Consumer Healthcare Products Association.
With all that use comes large potential for error. The whole point of using medication is to make us better, but taking it incorrectly can do more harm than good. It's estimated that around 1.5 million people each year are harmed by medication errors, with an impact on the economy of over $3.5 billion annually, according to research published by the Journal of Community Hospital Internal Medicine Perspectives.
Taking medication incorrectly doesn't just mean taking too much of it. There's a wide range of mistakes that can be made when taking medication — and some of them are so subtle that you may not even know you're doing them. Let's take a look at some of them now.
Splitting pills
Splitting a pill into two parts to halve the dose seems like a logical thing to do, right? However, this is a common practice that should be avoided unless advised by a doctor or pharmacist.
While cutting a pill can sometimes be okay, any labeled as "enteric-coated tablets" must be taken whole due to its protective coating, Dr. Craig Svensson, Purdue University College of Pharmacy's professor of medicinal chemistry and molecular pharmacology, explained to SingleCare. "Those are designed so the tablet doesn't dissolve until it gets to the intestines so that your stomach is protected." These coatings are often used on pain medication, both prescription and nonprescription.
Splitting time-release or extended-release medication can also be dangerous. As these pills are designed to act over a longer period, cutting them up is hazardous as it can make the medicine act faster and with more potency, Dr. Maria Torroella Carney, who works at Northwell Health as the chief of the division of geriatric and palliative medicine, told the site. These pills are often indicated with an "XR" somewhere in their name or description. It's vital to check with your doctor about any medication you're taking to see if it's safe to split.
Not taking your meds at the designated time
Did you forget to take your meds this morning? It might not seem like too big of a deal to vary the times of the day you take medications, but this can actually have a big impact on their effectiveness. "The body doesn't respond to medications in the same way at different times of the day," Michael Smolensky, University of Texas adjunct professor of biomedical engineering, told the AARP. While Smolensky pointed out that taking certain medications at less optimal times won't necessarily make them ineffective, it can certainly reduce their designed impact or else make them harder to tolerate.
This can be the case for medications that treat some most common conditions out there. Statins used to combat high cholesterol, for example, are most effective taken at bedtime, due to the liver's cholesterol production being highest during the night. Other medications for conditions like osteoarthritis should be taken according to your symptoms. If you're likely to experience joint pain in the afternoon, taking NSAIDs around four to six hours before you suspect your pain will peak will make sure its concentration is highest in your bloodstream when you need it most.
Combining your medications with the wrong foods
Many people take their medication with food in an effort to cushion the impact on the stomach. While certain medications should preferably be taken with a meal, some foods can interact with medication in unexpected ways.
Of course, taking most medication with alcohol is generally not advised, but drinking alcohol while taking any SSRIs used to treat depression, antibiotics like metronidazole, or common pain medication like Tylenol (or anything containing acetaminophen) can cause dangerous side effects like severe vomiting, liver toxicity, and gastrointestinal bleeding (per Everyday Health).
Other food and med combos are a little stranger. Did you know, for example, that combining your statin medication with grapefruit can be risky? "Grapefruit contains a compound that inhibits a common drug-metabolizing enzyme called CYP3A4," Aaron Emmel, clinical pharmacist, told Everyday Health. "Drinking a lot of the juice or eating the fruit inhibits this enzyme, and the drug accumulates in your system, which can be dangerous." And if you're taking warfarin as a blood thinner, avoid kale or anything with large amounts of vitamin K, as this can negate the effect of the drug in your system.
Taking certain meds on a full stomach
Following the instructions printed on your medication bottles is essential. If you are advised to take your pills on an empty stomach, you should do so. Taking certain medications on an empty stomach is advised to minimize other side effects that can come from ingestion, as is the case with Fosamax, a common anti-osteoporosis drug, as it minimizes esophageal irritation and promotes absorption (per The New York Times). Other drugs, like the HIV medication Sustiva, should also be taken on an empty stomach so absorption occurs more effectively, and ideally before bedtime due to the drowsiness it can induce.
But how do you know your stomach is actually empty when you take these meds? Knowing how long to wait after eating can be a bit of a guessing game, but a good rule of thumb is to leave a two-hour window, says the National Institute of Health. This can occur on either side of a meal, by either waiting two hours after eating before taking medication or waiting two hours to eat after taking it. Any instructions that come with your medication should help to clarify timings.
Taking your prescription medications alongside multivitamins or antacids
Vitamin supplements or over-the-counter antacids can often be considered pretty mild compared to other medications. However, you should be careful taking these supplements at the same time as your prescription medications as doing so can change their impact or else cause trouble. "The interaction can increase or decrease the effectiveness of the medicines, cause unexpected side effects, or increase the risk of known side effects," pharmacist Michael J. Gaunt told The Healthy. Even a typically innocuous multivitamin can interact with a surprisingly high number of drugs, as Drugs.com details, including medications used to treat types of cancer and blood-related conditions.
Additionally, antacids, which work to reduce the level of stomach acid in your gastrointestinal system, can interfere with your absorption of some medications. For example, combining antacids with medications like pseudoephedrine (a common decongestant) can cause faster absorption, leading to higher levels of the drug in your blood and potential toxicity, according to RxList.
Using a kitchen spoon to measure medication
Your kid has a cold and they need some cough syrup. So you reach into your drawer, pull out a teaspoon, and measure away. This mistake is one that a lot of people make. However, according to research published in the Pediatrics journal, "Compared with parents who used milliliter-only, parents who used teaspoon or tablespoon units had twice the odds of making an error with the intended and prescribed dose." Indeed, roughly 40% of parents make errors in dosing when using kitchen teaspoons or tablespoons to measure out medication.
In an adult, slight deviations in a dose wouldn't normally be too much of an issue. However, when you're dealing with little ones, every milliliter counts, as pediatrician Cindy Gellner told the University of Utah Health. Even just a small amount of extra medicine can be too much for some kids, explained Gellner, who highlighted another study published in Pediatrics that found that 21% of parents measured out more than twice the normal dose on occasion for their children. To avoid such large margins of error, consider buying a simple plastic oral syringe, which can be found in most drug stores.
Storing your medication in the bathroom
Hands up if you keep your medication in your bathroom cabinet! Okay, that's all of us, right? Unfortunately, we're all getting this one wrong. Keeping your medication in your bathroom means that it'll frequently come into contact with moisture and heat from your shower, bath, and sink, according to Medline Plus. This can reduce the potency of your medications and speed up deterioration. More worryingly, heat and moisture can cause reactions in certain medications. Aspirin, for example, breaks down into salicylic acid and vinegar, which can irritate your stomach.
The same thing can occur if you keep your medication in your kitchen near the stove or sink. To store medication properly, keep it in its original container in a cool, dry place away from direct sunlight — ideally in a sealed box. Always keep it out of sight and reach of children, and make sure to get rid of any drugs that have changed texture or color. Additionally, if your medicine bottle comes with a cotton ball or stopper, throw it away, as this can pull moisture towards the pills, hastening their breakdown.
Paying too much for your prescriptions
The pharmaceuticals industry in the United States is almost incomprehensibly large, with people spending some $539 billion on medication in 2020, according to Statista. With that amount of money, you'd want to make sure you're personally paying the best price you can get for your medication — yet too many people aren't.
"Every time a pharmacist dispenses a medication, they know a lot about other medications for sale that aren't necessarily related to that person's health plan," Shawn Bishop, former senior policy advisor for the U.S. Senate Finance Committee, told CBNC News. However, due to contractual obligations, your pharmacist may be discouraged or unable to promote similar and cheaper alternatives as they may not pertain to your policy.
This can lead consumers to pay much more than they need to on big-name brands when the same concentration of the medication is available at a lower price. Bishop recommends asking your pharmacist questions to see if there are lower-cost alternatives, even if they're not part of your plan. And remember, you might get a better price on the same medication at a different pharmacy, so it doesn't hurt to shop around.
Failing to follow your doctor's directions to the letter
A visit to the doctor often involves a lot of info flying your way at once. If you're finding it hard to remember your healthcare provider or pharmacist's instructions regarding the proper way to take your medications, know that misunderstandings are not uncommon. One study conducted by Northwestern University found that older adults are often confused "by the vague instructions on prescription bottles" (via ScienceDaily).
However, it's important to pay close attention to what your doctor or pharmacist tells you regarding your medication. When in doubt, ask them to repeat themselves, or take a pen and paper to write down their instructions properly. Remember, your medical team wants you to get the best care and to leave feeling confident with the medication you're taking, so an extra minute clarifying their instructions could save you a huge hassle and potential harm later on.
Mixing certain over-the-counter medications together
While prescribed medicines carry a certain weight to them, you may feel that the drugs you can purchase from the shelves are somehow less potent. Not only is this not necessarily the case, but mixing certain over-the-counter medications can be hugely harmful. Taking a combination of ibuprofen, naproxen, and aspirin might not seem like a big deal, but knocking these drugs back together — which all work along the same pathways — can heighten your chances of severe side effects like gastrointestinal bleeding, Tim Davis, pharmacist and National Community Pharmacists Association member, told Men's Health.
Taking cold medicine that contains acetaminophen with Tylenol can also spell disaster. Taking them together will likely cause you to exceed the daily limit of 4 grams of acetaminophen, Jesse R. Catlin, associate professor at California State University, told Men's Health. This can result in liver damage, according to MedicineNet.
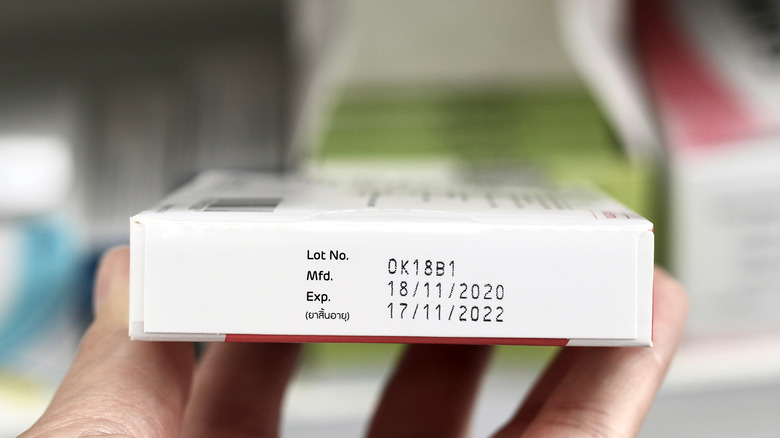
Using expired painkillers
It's easy to think that because your bottle of pills looks fine or isn't giving off a certain smell that an expired food would, that it should be fine to knock back — but it isn't. "People say, 'That drug is only a year past its expiration date; isn't it good?'" Kristen A. Binaso, a spokeswoman for the American Pharmacists Association and pharmacist, told WebMD. The consequences of this, according to Binaso, can be huge. "If you take a pill that's broken down, it may not work — or you may end up in the emergency room because of reaction to a breakdown product. That is really common."
Aside from this, if you were prescribed pain meds years ago, the thing you're taking the medication for now may well be a separate health concern requiring different medications. Holding on to old medication also increases the likelihood that it could be misused by someone else. For that reason, it's always important to dispose of the expired medication safely, by flushing them down the toilet if advised or mixing them with an undesirable substance like dirt or cat litter to reduce pets or children inadvertently consuming them, advises the FDA.
Staying on the same medication for too long
When you've been prescribed a medication, it's not only important to take it as instructed but to stop taking it as instructed too. For a wide range of medications, taking them past the advised period can cause a host of problems. Sleeping pills can be particularly problematic in this regard, as "you can build up a tolerance to them and then the same dose will no longer be effective," Baldwin Park Medical Center family physician Jack Chou explained to WebMD. Taking sleep medication persistently could also be treating the symptom of insomnia as a result of a different condition, like anxiety or sleep apnea, which might need a different course of treatment entirely.
Taking medicine for too long isn't just a problem with prescription medication, either. Over-the-counter decongestant nasal sprays can have counterproductive results if you use the products, intended as a temporary treatment, for too long. "It can actually make your congestion worse," Macary Marciniak, doctor of pharmacy and Eshelman School of Pharmacy professor, told the site.
Taking your medication irregularly
You might not think that missing a dose of your meds here and there is that big of a deal. But the proportion of people that underuse or completely skip their medications is not only huge, but the consequences can be dire.
Nonadherence to medication is a massive problem, with research published in the Cochrane Database of Systematic Reviews finding that people generally take around "half their prescribed doses." What's more, around 20 to 30% of people never even fill their prescriptions in the first place (via The New York Times).
What's the result of this? Approximately 125,000 deaths per year, as well as nonadherence to medication accounting for approximately 10% of all hospitalizations, The Times reported. It's important to understand the impact that not taking your medication could have on your health. As former Surgeon General C. Everett Koop told the publication, "Drugs don't work in patients who don't take them." Any doubts or concerns should be discussed with your doctor.
Stopping your medication early
So your doctor has prescribed you a medication and you're advised to take it for a certain period of time. However, your symptoms clear up long before the end of that time. Surely it would be okay to stop taking your prescription early, right? For a whole host of reasons, this is not advised. Coming off medication should not only be timed correctly but executed correctly.
In the case of antibiotics, for instance, "although you may feel better after a few days, all of the bacterial infection causing the symptoms is probably not yet eradicated until the full course of treatment is completed," Dave Walker, medical advisory board member for MedShadow Foundation and registered pharmacist, explained to The Healthy. The medication is still working behind the scenes, and halting too soon could undo all of the progress made.
When it's time to stop taking a medication, it's also vital to follow your doctor's instructions to a T, particularly if you need to taper off. "Some medications may have adverse effects when stopped suddenly, including SSRIs such as Prozac, which takes time to build in the system to become effective," advised Walker, who says that in the worst-case scenarios, stopping drug intake too quickly can have "severe consequences."