Symptoms Of A Stroke You Shouldn't Ignore
The first thing to remember about strokes is that they typically come on suddenly, says Northwestern Medicine, and you may experience several symptoms — such as trouble speaking, weakness or paralysis on one side of your body, and a splitting headache — all at the same time. The second and most important thing to remember is that you should call 911 or your local emergency medical services (EMS) first thing if you suspect you're having a stroke. A stroke occurs when there is a blockage in the brain, causing brain cells to start dying, says the Centers for Disease Control and Prevention (CDC). The longer you wait, the greater the damage to your brain and the lower your chances of recovery –- and even survival.
Why shouldn't you drive yourself to the hospital or have a friend take you? According to the CDC, the EMS team can start treatment while you're being driven to the hospital. They'll know which hospital is best suited to treat stroke patients, and will give the hospital a head's up that you're coming. What's more, you'll most likely get faster care if you arrive in an ambulance. Now, on to the symptoms that should set this race with the clock in motion.
Difficulty speaking or understanding others
The sudden onset of garbled speech, difficulty finding words, or trouble understanding what others are saying may be signs that you're having a stroke in the left side of your brain, which is the control center for speech and language, according to the American Stroke Association. This condition is called aphasia.
There are three types of aphasia: Wernicke's aphasia, Broca's aphasia, and Global aphasia. They are differentiated by the part of the brain's left hemisphere that is damaged and the symptoms that result. For example, you may have Wernicke's aphasia if your words or sentences don't make any sense. You may have Broca's aphasia if you use a word that is almost the word you intend, but not quite.
Other explanations for speaking difficulties include drinking too much alcohol or having a migraine, says WebMD. People with multiple sclerosis also may have trouble speaking. But if your symptoms come on swiftly and you have other stroke symptoms simultaneously, there's a good chance a stroke is underway and you need medical help immediately.
Off-kilter facial features
See someone — or even yourself — with a sagging eyelid or twisted smile and you'll probably think "stroke" right away because asymmetrical facial features are one of the best-known stroke symptoms (via Verywell Health). The symptom is caused by the nerve that controls your facial muscles being damaged when oxygen to your brain is blocked (ischemic stroke) or when bleeding in your brain creates too much pressure (hemorrhagic stroke), according to FacialPalsy UK.
Facial paralysis is also a symptom of Bell's palsy, another common condition, says the National Institute of Neurological Disorders and Stroke (via Healthline). Bell's palsy is caused by inflammation of the nerve that controls your facial muscles, possibly due to a viral infection. It isn't as serious a condition as a stroke, and most people fully recover within several months. One way to differentiate between the two conditions is that stroke-related facial droop is usually accompanied by other stroke symptoms, such as slurred speech, a splitting headache, or trouble walking, says Verywell Health.
Weakness or paralysis on one side of your body
If your right leg suddenly becomes so weak you can't walk, or you can't move your right arm at all, these are both well-known signs that you may be experiencing a stroke, and that the stroke is damaging the part of the brain that directs your muscles to move, according to FlintRehab.
If the symptoms are affecting your right side, it's likely that the stroke is occurring in the left hemisphere of your brain. If the symptoms are on your left side, the right hemisphere of your brain is probably being damaged. Hemiparesis is the term for weakness on one side of your body, and hemiplegia means paralysis on one side of your body.
Numbness in your arms and legs is often thought to be a symptom of a stroke, but it's usually caused by some other kind of nerve damage, says Healthline. However, if numbness is accompanied by the sudden onset of facial paralysis, difficulty speaking, or other stroke symptoms, it's time to get immediate medical attention.
Dizziness, vertigo, and loss of balance
Dizziness by itself is not a red flag for a stroke, but dizziness that's accompanied by vertigo, loss of balance, or other stroke symptoms may signal a brain stem stroke, explains the American Stroke Association. The brain stem controls the central nervous system, including motor skills, and you are at increased risk of this type of stroke if you have diabetes, high blood pressure, heart disease, atrial fibrillation, or are a smoker.
Dizziness and vertigo might seem like very similar symptoms, but there are differences, according to the Cleveland Clinic. Dizziness is an impairment of spatial orientation, and may include lightheadedness and unsteadiness. Vertigo is more a feeling of whirling or spinning. Both are categorized as balance problems. Crystal clear, right? Balance problems are often associated with aging, but you can experience them at any age. In addition to being a possible symptom of a stroke, they can also be caused by inner ear problems, high or low blood pressure, or low blood sugar.
Vision changes
Vision changes are often a symptom of a transient ischemic attack (TIA), also known as a mini-stroke or warning stroke because it tends to be a precursor of a major stroke (via NovaVision). Vision loss associated with a TIA often involves dimming of vision in one eye, but could also manifest as complete loss of vision, blurry vision, or sensitivity to bright light.
The control center for vision is in the brain's occipital lobe at the back of your head, explains Dr. Carole Thomas, a neurologist at Virtua Health. If the stroke affects the right occipital lobe, you may experience vision problems in the left field of vision in both eyes, and if the left occipital lobe is damaged, the vision changes will be in the right field of vision in both eyes. Blindness could occur if the stroke affects both left and right occipital lobes, but that instance is rare.
If you experience sudden vision changes or vision loss, even if the symptoms vanish quickly, seek emergency care immediately. In addition, it's important to get regular vision exams because eye doctors can often detect blood vessel blockages behind the eyes that portend a potential stroke, says the American Academy of Ophthalmology.
Headache
As many as 65% of people who are having a stroke get a bad headache as one of the symptoms, according to Premier Neurology & Wellness Center. But how do you tell if you're just having a normal, run-of-the-mill headache or migraine or if you are having a stroke?
First, a stroke-related headache comes on in minutes or even seconds, rather than inching up on you gradually. The pain may be centered anywhere in your head, such as your forehead or toward the back of your head, depending on where the stroke is taking place in your brain. Stroke-related headache pain may be accompanied by loss of vision or feeling, and many people describe the headache as the worst they've ever had, says Verywell Health. Finally, a stroke-related headache will probably be accompanied by other stroke symptoms, such as garbled speech, asymmetrical facial features, or weakness on one side of your body.
Hiccups
In most cases, hiccups are nothing to worry about. However, if you're experiencing major, serious hiccups that can't be explained by the usual causes, such as drinking carbonated beverages or swallowing air while you're chomping on gum, you may be having a stroke, according to Prevention. Also, if you listen carefully to your body rather than focusing solely on those annoying hiccups, you may detect other cardiovascular symptoms of stroke, such as chest pains, blurred vision, or numbness.
It's time to see your doctor if your hiccups last longer than a couple of days, even if you have no other symptoms. The hiccups may, indeed, be no big deal. But get swift medical attention if your hiccups are accompanied by any other stroke-related symptoms, says J. Chad Hoyle, a neurologist at The Ohio State University Wexner Medical Center. While it's rare that hiccups are a tip-off to a stroke, the mere chance that they might be is worth a trip to the hospital.
Nausea or vomiting
Nausea and vomiting are not the most common symptoms of a stroke, and they may be mistaken for the flu or food poisoning. However, these symptoms could also signal a hemorrhagic stroke, which means there's life-threatening bleeding going on in your brain, according to the Mount Sinai Cerebrovascular Center.
How do you decide whether to hunker down and wait out your symptoms or to call 911? As with the other stroke symptoms, sudden onset of nausea or vomiting should be your go-to clue, says Cleveland Clinic Martin Health. The symptoms come on fast, rather than creeping up on you over hours or days.
One interesting but scary tidbit is that people who experience vomiting when they're having a stroke are more likely to die than people who don't vomit, according to a study published in the British Medical Association's Emergency Medicine Journal. That's as good a reason as any to be on the safe side and get immediate medical attention.
Fatigue, seizures, and other symptoms specific to women
Women and men experience many of the same stroke symptoms, but women have some additional common symptoms, including fatigue, fainting or loss of consciousness, seizures, general weakness, shortness of breath, and even hallucinations, according to the American Stroke Association (via San Antonio Regional Hospital).
"Women more frequently have atypical, vague symptoms," says Dr. Pouja Khatri, neurology professor at the University of Cincinnati and director of the university's stroke team, in American Heart Association News. "They might start with fatigue, confusion or maybe general weakness, as opposed to weakness on one side of the body."
The fact that these symptoms are less commonly associated with strokes may be one reason why women represent almost 60% of stroke deaths in the United States. In addition, women are at higher risk for stroke if they're taking birth control medication or experience high blood pressure during pregnancy, explains the CDC.
Seizures and other stroke symptoms in children
Strokes can occur at any age, although they become more common as you get older. Even children can have strokes, and prenatal and newborn babies are at the highest risk of all children, according to the National Institute of Neurological Disorders and Stroke.
Many of the stroke symptoms seen in babies and children are similar to those experienced by adults, but kids may also exhibit loss of consciousness, seizures, or breathing issues. Strokes in fetuses may result in babies born with cerebral palsy, and strokes during the first year of life, or when symptoms include loss of consciousness or seizures, often cause lifelong disabilities.
If there's good news here, it's that youngsters may be better able to recover from a stroke than adults because their young, flexible brains can more easily regroup and compensate for any disabilities. Speedy diagnosis, treatment, and rehabilitation are keys to minimizing long-lasting problems.
Your ability to move easily or think clearly decreases in a barely noticeable way
Sudden, dramatic symptoms are the calling card of most strokes, but there are also silent strokes that have no symptoms at all. You might notice that you're not feeling as strong as you used to, or that you're having a little more trouble finding the right words, but you may chock it up to normal aging. It isn't until a brain scan such as an MRI or CT is done that white spots are seen on the brain that indicate the scar tissue left by silent strokes. The scans may be used as a diagnostic tool for symptoms like dizziness or headaches.
A scientific statement published in the journal Stroke notes that silent strokes become common as you get older and are a sign that you may be at risk of future strokes. "It is important to go to your family physician if there are concerns about neurological symptoms like weakness or speech difficulty because silent strokes put people at risk not only for future symptomatic strokes but also for cognitive decline and dementia," said one of the statement authors Dr. Eric E. Smith, an associate professor of neurology at the University of Calgary in Alberta, Canada, to the American Heart Association News. People who smoke or have conditions involving the blood vessels are also more likely to experience silent strokes, according to the American Stroke Association.
Stroke symptoms that last from a few minutes to 24 hours
If you have stroke symptoms such as weakness in your arm or dizziness, but the symptoms don't last long, you may have experienced a transient ischemic attack (TIA) or mini stroke. That's when blood is blocked from your brain for a short period of time, and it's often a warning sign that a major stroke is coming soon, explains the American Stroke Association. In fact, the association says "warning stroke" is a more accurate description of a TIA than "mini stroke," because about a third of the people who suffer major strokes have had a TIA during the last year.
A study published in the scientific journal of the American Academy of Neurology found that TIAs are a common precursor of an ischemic or major stroke. Out of 2,416 stroke patients the study examined, 17% experienced a TIA on the day of their stroke, 9% had a TIA on the day before their stroke, and 43% had a TIA sometime within the week of their stroke. Blockages in the brain that cause TIAs usually resolve themselves by breaking up or becoming dislodged, and usually don't harm the brain. But if you experience a TIA, preventive medical treatment is needed within a few hours to fend off a major stroke.
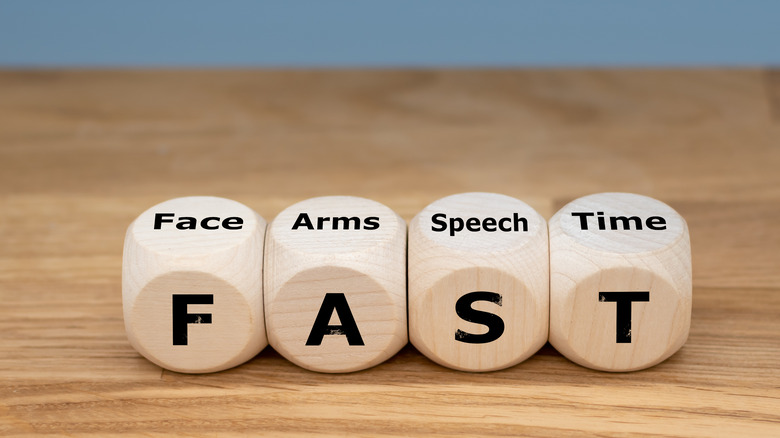
Easy ways to remember -- and make sure you don't ignore -- stroke symptoms
The acronym most commonly used as a way of identifying stroke symptoms and remembering to get help fast is, not surprisingly, FAST (via the CDC). F stands for Face: Are any of the person's facial features drooping or does their smile look weirdly asymmetrical? A stands for Arms: It's your cue to check whether the person can raise both their arms at the same time. Does one arm hang limp or rise to a lesser height than the opposite arm? S stands for Speech: Is the person's speech garbled or slurred? Can they say a simple sentence, or are they having trouble finding words? T stands for Time: Time is of the essence if you notice any of these symptoms. Call 911 or your local emergency medical services (EMS) immediately.
While FAST is the most frequently used acronym for stroke diagnosis, a University of Kentucky Stroke Center study found that 14% of strokes are missed using that acronym (via University Health System), and the more comprehensive acronym to use is BEFAST. B stands for Balance: Are you observing the person wobbling, weaving, or falling? E stands for Eyes: Does the person have blurred, dim, or double vision, and even blindness? These are all also common symptoms of a stroke.
Any unexplainable symptom that comes on suddenly
Many people experience telltale warning signs in the days or weeks prior to a stroke, but ignore them (via Medical City Healthcare). Let's say your vision suddenly becomes blurry for a few minutes, your balance seems a little off one day, or one of your arms feels weak and weird for a bit. Since the symptoms don't last long, they're no big deal, right? Maybe, but maybe not, according to vascular surgeon Marc Salhanick, speaking to Medical City Healthcare.
"Even before FAST, there are some things that you might see beforehand and be able to identify," says Dr. Salhanick. "What tends to happen is that these events start to become closer and closer together. When patients sit back and think about it after they've had a stroke, they say 'oh yes, there was that one time a few weeks ago that I had that blindness and then last week I was maybe having some difficulty talking, but it kind of went away and came back.'"
The bottom line is to trust your intuition and get emergency care right away if there's a chance that your symptoms might indicate a stroke. That trip to the hospital could save your life.