What You Don't Know About Silent Endometriosis
Millions of women suffer from endometriosis, a disorder affecting as many as 10% of American women ages 25 through 40, per Johns Hopkins Medicine. Endometriosis is a disease where endometrial tissue grows outside a woman's uterus. Common locations it occurs include the ovaries, fallopian tubes, uterus' outer surface, pelvic cavity lining, ligaments supporting the uterus, and spaces between the uterus and the rectum and between the uterus and the bladder. The disease can also be found in less common places, including the bladder, rectum, and intestines.
An alarming 20 to 25% of women with endometriosis have no symptoms — something not commonly known. This is called silent endometriosis, or asymptomatic endometriosis (via Everyday Health). Many times, these women only learn of its presence after struggling with infertility. "On average, women see four or more doctors for their pain before they are diagnosed with endometriosis," Barbara Stegmann, reproductive endocrinologist and infertility specialist, told Best Health Magazine. This is because it's a largely misunderstood and "missed" disease, as it's received little government attention and funding.
With such a lack of awareness regarding this common disease in women — which, if undetected, can progress, leading to infertility or increased risk for endometrial cancer (per Medical News Today) — it's important to shed light on this little-known phenomenon or "Silent Epidemic."
Endometriosis is a misunderstood disease
Endometriosis is largely misunderstood, taking over seven years on average to confirm a diagnosis. "Some women don't realize, there's something called 'silent endo,'" said Christine Metz, medical researcher with the Feinstein Institute, to the 20-Minute Health Talk podcast (via Northwell Health). "Women could have absolutely no pain and have very severe disease and what they call that is 'silent endometriosis.' And many of those women get diagnosed when they have tried to have children for several years and have been not able to do so."
Society generally misunderstands menstruation symptoms. Severe cramping is thought to be typical, leading women to feel they're overreacting. Gynecologist Kimberly Kho at the UT Southwestern Medical Center said this incorrect mindset leads women to normalize the pain and downplay their symptoms. One example comes from "Top Chef" host Padma Lakshmi: "I hid it to a certain degree — not intentionally but ... it's weird to talk about your period all the time."
Endometriosis research is also poorly funded. While the disease costs women globally about $3.7 trillion each year in healthcare costs and lost work, it only received $10 million in federal funding in 2016 — less than many other conditions, per Best Health Magazine. Compare this amount, for instance, to $51 million in research funding for anthrax during the same year, in which there were zero cases. Also to blame is a lack of diagnostic tools (perhaps related to the low funding). As such, the public is generally uneducated about endometriosis. Celmatix, a biotech firm focused on ovarian health, conducted a survey and found that 37% of the women hadn't heard of the disease, while 41% were only vaguely familiar with it.
What are the symptoms of endometriosis?
To better understand silent, or asymptomatic, endometriosis, it's important to know the symptoms common to the disease. Symptoms can surface in different ways, but they most commonly include, according to Johns Hopkins Medicine, severe menstrual cramps in the abdomen, lower back pain, heavy periods, pain during sexual intercourse, painful urination or bowel movements during menstruation, and gastrointestinal issues such as nausea, diarrhea, and constipation. Endometriosis may also cause fatigue (per the Endometriosis Association).
As Johns Hopkins points out, the severity of pain is not indicative of the severity of the disease, as patients with severe pain may have mild endometriosis, whereas patients with minimal pain or no pain — silent endometriosis — may have an advanced form of the disease.
Infertility is also a symptom of endometriosis. In cases of silent endometriosis, infertility is usually the first sign that something is wrong (per Everyday Health). "Sometimes the only symptom is infertility. There's no pain, or regular period cramps and then you try to get pregnant," as gynecologist Jacquelyn Stone told SheKnows. And, as Body + Soul notes, some symptoms — back pain, nausea, and changes in bathroom habits, for example — may be so subtle that you attribute them to something else.
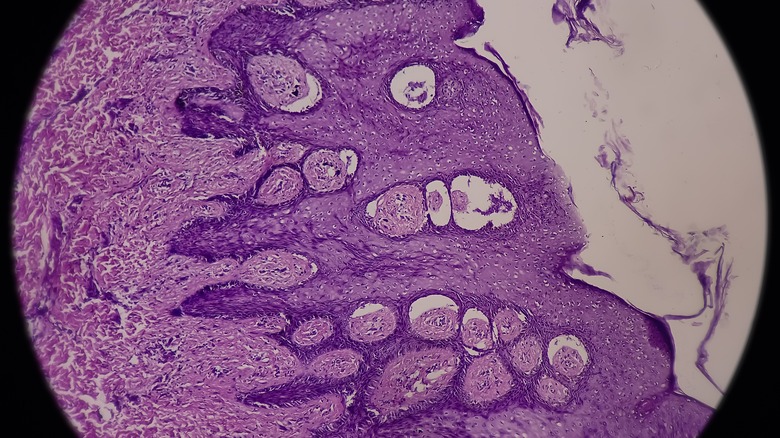
Endometriosis is only diagnosed through laparoscopic surgery
Though there are some tools that can provide clues as to whether a patient has endometriosis, with silent endometriosis' lack of or inconsistent symptoms, the only way a definitive diagnosis can be reached is through laparoscopic surgery (via Body + Soul). This is a minimally invasive procedure where a surgeon views the entire pelvic region through an incision in the wall of the abdomen where a thin tube with a light and lens is inserted.
As gynecologist Dr. Devini Ameratunga explains in Body + Soul, whether your doctor recommends the procedure depends on the physician and each individualized case, with some wanting to order other imaging tests before proceeding with surgery: "There is no specific recipe, and treatment and investigation needs to be individualized. Even in the fertility patient, surgery for endometriosis if suspected may not be the first thing to do. We need to balance symptoms, age of patient, chances of success with surgery and fertility treatment and risks to the patient, amongst other factors."
Silent endometriosis is a common cause of unexplained infertility and recurrent miscarriage
Unexplained infertility is when a woman is unable to conceive naturally or through assisted reproduction with no known cause. It is also used to describe women with recurrent miscarriages that have no apparent cause, per the Journal of Reproduction and Infertility.
Unexplained infertility can be a controversial topic, as some medical professionals don't believe in it — from their perspective, there must be some cause, even if currently unknown (via ReceptivaDX). The lack of testing to diagnose the presence of endometriosis further contributes to the phenomenon of unexplained infertility, as the Journal of Reproduction and Infertility notes. And in many cases of unexplained infertility, the cause is often endometriosis.
Even patients with mild cases can have their chances of a healthy pregnancy reduced. Jennifer Hirshfeld-Cytron, gynecologist and Fertility Preservation director at the Fertility Centers of Illinois, explained to Best Health Magazine how the disease causes infertility: "For those with endometriosis, there are many different fertility challenges that can result — blockage of the fallopian tubes, damage to the egg supply (also known as the ovarian reserve), scar tissue, and adhesions that impact reproductive function, and an overall hostile environment for sperm and eggs to flourish within."
What are some risk factors for silent endometriosis?
Endometriosis can affect any person with a uterus. Though there is no known cause, certain factors may put you at risk. According to Johns Hopkins Medicine, endometriosis can be hereditary, so if your mom or sister has it, you could too. Best Health Magazine reported that ethnicity may even play a role — with a higher prevalence in Asian and Caucasian women.
If you've given birth after age 30 — endometriosis can also sometimes develop from a C-section — or have never given birth (per Meraki Nutrition), this could point to endometriosis. Additional risk factors include menstrual periods lasting longer than seven days, short menstrual cycles of under 27 days, chemical sensitivities, recurring yeast infections, and lifestyle factors, including lack of exercise and caffeine and alcohol use.
Other risk factors are unbalanced hormones, spotting before menstruation, pain during ovulation, and ovarian cysts — particularly "chocolate" cysts (cysts filled with old blood, giving off a brownish appearance, detectable via ultrasound) — as gynecologist Devini Ameratunga informed Body & Soul. Endometriosis also is likely to occur alongside other chronic conditions. A 2002 study from Human Reproduction found that women with known conditions such as thyroid disorders, fibromyalgia, lupus, or rheumatoid arthritis are more likely to also have endometriosis. Indeed, research shows some 20% of women with endometriosis have another chronic condition.
Silent endometriosis can impact egg reserve and egg quality
Women with silent endometriosis generally discover their diagnosis only after struggling with infertility. Endometriosis affects the fertility of 35-50% of those with the disease. According to a review article published in Frontiers in Endocrinology, endometriosis can impact fertility through a lower egg reserve and poor egg quality. The degree to which egg reserve or egg quality is altered depends on the level of the disease's severity. This is based on a rating system from the American Society of Reproductive Medicine, which serves as the standard for measuring the degree of endometriosis disease, as determined by a surgical laparoscopy. Per Johns Hopkins Medicine, these four stages are Stage 1 (minimal), Stage 2 (mild), Stage 3 (moderate), and Stage 4 (severe). Each stage is assessed based on where the endometrial tissue is located, the amount present, the depth of the adhesions, and the size of each.
Those with more advanced stages of endometrial disease may have a lower egg reserve and poorer quality of embryos as a result, whereas those with milder stages of endometriosis may be less affected in terms of egg reserve and quality. According to a review published in Obstetrics and Gynecology Clinics of America, when endometriosis is present, an increase in free radicals can affect the viability of embryos.
Silent endometriosis can impact ovulation and implantation
Endometriosis can also affect someone's ability to become pregnant by impeding the egg fertilization process, or by impeding the process by which a fertilized egg implants into the uterine wall. While endometriosis generally can result in infertility, silent endometriosis presents a greater risk because of the lack of symptoms and progression of the disease.
One study published in Obstetrics and Gynecology Clinics of America proposes several means by which endometriosis harms conception prospects. In cases of natural cycles or ones with intrauterine insemination (IUI, where a man's sperm is inserted directly into a woman's uterus), the presence of endometrial scar tissue can create an inflammatory environment, affecting the fallopian tubes and making conception less likely. This inflammation can also affect sperm quality. Additionally, women with endometriosis have more free radicals in their system, which can throw off ovulation. In situations where an embryo is transferred to the uterus through in-vitro fertilization, the inflammation from undetected endometrial scar tissue and adhesions can impact the endometrium's ability to receive the embryo.
What role might the immune system play in silent endometriosis?
While the medical community doesn't know of a specific cause for endometriosis, research shows that the immune system may play a role. Consider this: According to the Endometriosis Association, if you have an immune condition such as asthma, allergies, sinusitis, or eczema, you may be more likely to also have endometriosis. A weak immune system, evidenced by the presence of one or more immune conditions, may be unable to prevent endometrial tissue from breaking down, according to Meraki Nutrition. One study found that women with endometriosis displayed altered biological processes in regards to the endocrine and immune systems.
Regarding infertility specifically, an emerging field of research known as reproductive immunology studies the role of the immune system in infertility, with research pointing to the idea that, in the case of in-vitro fertilization (IVF), the body may see an embryo as a foreign invader and fight it. The general belief of reproductive immunologists such as Braverman Reproductive Immunology, a leading provider, is that endometriosis, a disorder of the immune system, is usually the reason for multiple unsuccessful embryo transfers (in IVF) or recurrent miscarriage.
Endometriosis can be removed surgically
Laparoscopies are used not only to diagnose endometriosis, but also to surgically remove endometriosis growths to relieve symptoms, improve fertility outcomes, and stop disease progression. It's shown to be successful in many cases. "With surgery, some [issues caused by endometriosis] can be remedied and fertility treatment options such as in vitro fertilization, medically-stimulated cycles, and intrauterine insemination are commonly used by endometriosis patients with success," gynecologist Jennifer Hirshfeld-Cytron shared with Best Health Magazine.
Endometriosis tissue is removed during a laparoscopy through excision or ablation. Per Endometriosis.net, in ablation, endometrial growths are burned off through freezing, heat, electrosurgery, or radiofrequency. In excision, they're cut out from their root. Some specialists find that the tissue is less likely to return with excision. Fewer physicians are trained to do excision, however, and because it's more invasive, the recovery time is longer.
In some cases, physicians choose the method based on other factors, such as the location (excision can be risky and can potentially damage adjacent organs) and depth of the adhesions (ablation can be more effective for surface-level adhesions than deeper ones). One patient advocate for Endometrios.net explained her personal experience, saying, "When I was looking for a specialist to treat my endometriosis, many fellow patients told me that the most effective treatment would be excision surgery. However, when I finally spoke to my specialist, he told me he used both procedures depending on the type of adhesions and their location."
Endometriosis can be treated with medication
Medication is another way that endometriosis can be managed. As Johns Hopkins Medicine notes, this depends largely on whether or not your desire is to get pregnant. Other factors include current symptoms, severity of the disease, tolerance for the medication suggested, and personal preference. It really all depends on the individual case.
Possible medication includes pain meds — including common over-the-counter nonsteroidal anti-inflammatory drugs, such as Ibuprofen — and hormone therapy (though you'd be less likely to have pain with silent endometriosis, with only subtle symptoms, if any). To prevent ovulation and lessen menstrual flow, reducing the opportunities for endometriosis tissue to deposit, your doctor may prescribe birth control pills, which contain estrogen and a synthetic form of progesterone called progestin. You may also be prescribed stand-alone progestin, medication that mimics menopause, or a synthetic male hormone. Hormone therapy, however, is generally used for only a short period of time because of its possible side effects, according to the American Pregnancy Association, which adds that it's best used along with surgery.
Endometriosis may be managed through a variety of holistic methods
Medication is not the only way to keep endometriosis under control. Endometriosis can be managed through a variety of holistic and lifestyle practices, especially when used in combination with other medical treatments. This is especially important after having endometriosis surgery to help prevent the disease from returning or from progressing. Research shows that diet can play a role in the management and even the development of endometriosis, since it's a chronic inflammatory disease. Fruits, vegetables, and fatty fish such as salmon are helpful in fighting endometriosis. One study from Human Reproduction showed that unhealthy fats can contribute to endometriosis risk and can exacerbate the disease.
In addition to dietary changes, other alternative treatments, including acupuncture, vitamins, and herbs, have been shown to benefit those with the disease. There are trained specialists in these areas who are knowledgeable about women's health issues including endometriosis and infertility, per the American Pregnancy Association.
Pregnancy and menopause can provide relief for endometriosis symptoms
Though endometriosis has no cure, its symptoms may lessen and even possibly go away with pregnancy. "With the uterus housing a growing child rather than building endometrial tissue to shed each month during a period, the cause of unpleasant and painful symptoms is absent," as gynecologist Jennifer Hirshfeld-Cytron informed Best Health Magazine. And as the publication points out, becoming pregnant after a struggle with infertility is likely to provide emotional relief as well. Additionally, according to Healthline, the increase in progesterone during pregnancy may help you feel better, as it's believed to suppress and reduce the size of endometrial adhesions. However, everyone is different, and the way your body responds is likely not the same way someone else's would.
In addition, once menopause begins, endometriosis doesn't present as much of a problem to those with apparent symptoms. "Women find that endometriosis symptoms begin to diminish once menopause begins," Hirshfeld-Cytron says (via Best Health Magazine).
Patient advocacy is key when it comes to endometriosis
We can't stress enough the importance of advocating for yourself and others when it comes to silent endometriosis, of which the only sign may be ongoing infertility. It's important to listen to your gut, since "you know your own body better than anyone else does," as nurse Jenneh Bockari wrote for Healthline. If something doesn't feel right, don't hesitate to get a second opinion (or more). Advocating for yourself is empowering. "Everything we go through is a conduit to empower someone else. Advocacy has taught me that," April Christina, blogger and endometriosis advocate, shared via Healthline. "Your voice has the power to make a difference."
There are many ways to advocate. Share your story on a blog or social media platform. Keep a journal to put your thoughts down when your emotions are raw. Bring the journal with you to appointments with your doctor, since it's not easy to remember in the moment everything you might want to say. Or bring someone with you to appointments for support and to help communicate something you might miss. Having someone there with you can help you feel more empowered to speak up. "Every patient with endometriosis deserves an opportunity to be heard, supported, and healed," said Jessica Shields, a gynecological surgeon and professor at the UT Southwestern Medical Center.
There is hope for those with silent endometriosis
For those struggling with endometriosis, hope is on the horizon. "We have come quite a long way in understanding endometriosis, how it affects fertility, and how to treat it," said gynecologist Divya Kelath Shah, assistant professor of clinical obstetrics and gynecology at Penn Medicine. In terms of fertility, she said, "your chances of conceiving are better than they've ever been, so it's worth looking into the many treatment options that are available."
In April 2022, endometriosis patient advocate April Summerford was a guest on an episode of the podcast "20-minute Health Talk," the topic of which was breakthrough research to develop less invasive techniques for endometriosis diagnosis (via Northwell Health). "There's a huge gap between if you think you have this problem and actual diagnosis which, if you think about it, is surgery," Summerford said. "So, I can't wait to have a painless diagnostic test that would tell them, you know, with some confidence if they need to go further with their journey and see what's going on, they would feel a lot better if they knew."