Vasculitis Explained: Everything You Need To Know
Ashton Kutcher recently revealed to the public that several years ago he suffered a flare-up of a condition known as vasculitis, per NPR. It came up as Kutcher and British adventurer Bear Grylls shot the August 8, 2022 episode of National Geographic's "Running Wild with Bear Grylls: The Challenge." Grylls and Kutcher were trekking through a thick wood when Kutcher observed that he found the conditions tricky. In response, Grylls observed that he'd never met a strong person who'd had an easy road — before inquiring as to where that strength comes from for Kutcher.
That's when Kutcher opened up about some of what he went through in his experience with vasculitis. "Like two years ago," Kutcher explained, "I had this weird, super rare form of vasculitis, that like knocked out my vision, it knocked out my hearing, it knocked out like all my equilibrium," the last of which made walking difficult (via Access Online). This went on for about a year, and although there were times when Kutcher wasn't sure if he would ever see, hear, or walk again, he has clarified via Tweet that he is now, indeed, fully recovered. He's even training for the New York City Marathon that will take place on November 6, 2022 (via NPR).
So what exactly is vasculitis? And why did it effect Kutcher's vision, hearing, and balance? Read on as we explore the condition, its symptoms, who is at risk, and its long-term prognosis.
Vasculitis and blood vessels
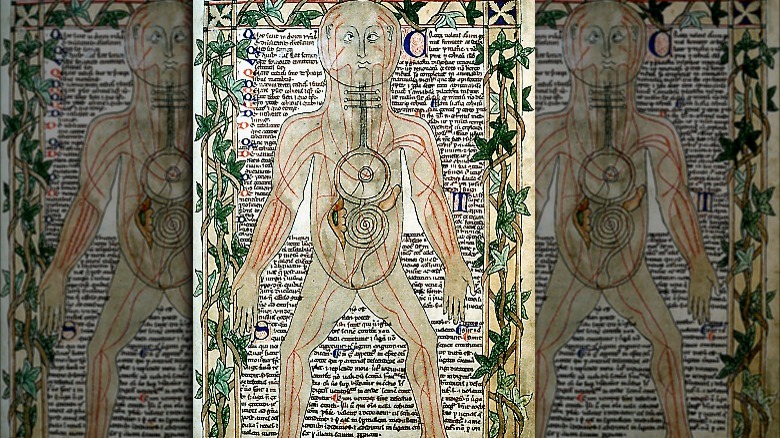
The last time vasculitis was in the spotlight was 2014 (via CBS News), when actor and filmmaker Harold Ramis, 69, died from vasculitis complications. Ramis had been dealing with vasculitis for the last four years of his life. Vasculitis refers to inflammation of the blood vessels, according to Rheumatology. The term, "blood vessels" refers to the tubular channels that transport blood throughout the body to distribute oxygen and nutrients that are vital to the survival and function of all human tissue, according to the Cleveland Clinic. The average human body has about 60,000 miles worth of blood vessels.
Vasculitis doesn't affect all the blood vessels, just select ones, according to Versus Arthritis. Which blood vessels are affected depends upon the type of vasculitis, of which there are many, as discussed below (via NYU Langone Health). Which bodily systems are impacted depends upon which are served by the affected vessels. In all cases, an inflammatory process causes the walls of the affected blood vessels to swell. As a result, blood flow to adjacent tissue is impaired — or even fully blocked — which leads to damage of the tissue and other complications.
Vasculitis can be mild, or it can be life threatening, depending on which blood vessels and tissue are affected and to what degree. It can occur as a sequela of another condition or disease process (secondary vasculitis), or it can occur spontaneously for reasons not immediately apparent (primary vasculitis), according to a 2007 paper published in Arthritis Research & Therapy.
There are many kinds of vasculitis
"Vasculitis" refers to at least 20 different blood vessel inflammation disorders, according to NYU Langone Health. Clinicians categorize them based on size of the vessel involved. Small vessel vasculitis is often associated with autoimmune diseases such as rheumatoid arthritis and lupus and can also affect vessels and related tissue throughout the body (via HSS). For example, granulomatosis with polyangiitis affects the blood vessels of the nose, sinuses, ears, lungs, and kidneys. Kutcher characterized his vasculitis as autoimmune in nature, but that doesn't tell us much because vasculitis is generally considered autoimmune (via WP Hospital).
Examples of medium vessel vasculitis include Kawasaki disease, which primarily affects children and causes swelling of the hands and feet but also peeling of the skin and fever, Buerger's disease, which tends to affect the hands and feet of smokers, and polyarteritis nodosa, the most common type in middle-aged adults, which affects the heart, kidneys skin, muscles, intestines, and peripheral nerves (via the Mayo Clinic).
Large vessel vasculitis affects major arteries (e.g. aortic). Temporal arterial vasculitis, also known as "giant cell arteritis" is the most common vasculitis disorder in adults over the age of 50 (per Johns Hopkins Vasculitis Center). It's known to be associated with vision impairment — as Kutcher dealt with — but so are other forms of vasculitis, including Cogan's syndrome, a large-vessel disorder known to affect hearing and equilibrium, in addition to vision (via Vasculitis Foundation). That said, Kutcher hasn't indicated which type of vasculitis he's dealt with.
Vasculitis causes
Vasculitis can be primary or secondary in nature, per the Mayo Clinic. Secondary vasculitis refers to vasculitis that occurs as a sequela of another disease or condition. Almost any infection has the potential to cause vasculitis because infection triggers an immune response, which inevitably involves some degree of inflammation. However, the most common infections associated with vasculitis include strep, salmonella, herpes 1 and 2, and hepatitis B and C.
According to a 2015 paper published in an Italian medical journal, infection can lead to vasculitis either directly (where the infection will either damage affected blood vessels, causing inflammation) or indirectly (where the immune response triggered by the infection attacks the blood vessels as if they were a pathogen). Many infections may cause vasculitis with a combination of direct and indirect activity. The presence of the human immunodeficiency virus (HIV) in the blood can also trigger vasculitis. So too can reactions to certain drugs. And any autoimmune disease, by its very nature (autoimmune disease causes the immune system to attack the body) has the potential to cause vasculitis. So too do certain blood cancers.
Sometimes vasculitis occurs in the absence of a primary diagnosis. This is known as primary vasculitis, which is sometimes considered idiopathic (i.e., without a known cause). That being said, an underlying condition or stimulus often does exist, although it may take a good bit of medical sleuthing to identify it. Often, it turns out to be infection (though the research is not "fully understood" yet), according to a 2021 paper published in JAMA.
Some medications can put you at risk for vasculitis
A number of medications can cause what is known as drug-induced vasculitis, which, as it sounds, refers to inflammation of the blood vessels as a result of an adverse reaction to a drug (per Springer). The drugs most commonly associated with what is sometimes referred to as "hypersensitivity vasculitis" include propylthiouruacil (which is used to treat hyperthyroidism), hydralazine (which treats high blood pressure), minocycline (used to treat certain bacterial infections), allopurinol (which is used to treat gout), penicillamine (which is used to treat several disorders, including rheumatoid arthritis), sulfasalazine (for rheumatoid arthritis and ulcerative colitis), and antibiotics in the penicillin and the cephalosporin families.
In addition, some drugs used in chemotherapy may cause vasculitis, according to Mussen Healthcare. And illegal drug use has been linked to vasculitis, according to Mussen Healthcare and the authors of a 2016 paper published in Rambam Maimonides Medical Journal.
Hypersensitivity vasculitis can be difficult to identity, in part because it does not present differently from vasculitis due to other causes — including with regard to its severity, according to Springer. In addition, some of the conditions that the drugs most commonly associated with hypersensitivity vasculitis are used in treating conditions that, themselves, are associated with or cause inflammation (e.g., sulfasalazine). But if vasculitis occurs soon after a new drug therapy has been initiated, that may point to hypersensitivity to the drug.
Those who are at risk
As a general matter, vasculitis is an equal opportunity condition. It can happen to literally anyone in possession of blood vessels and an immune system (i.e., everyone), according to the National Heart, Lung, and Blood Institute. However, certain forms of vasculitis are more common in certain age groups and other demographics. For example, Kawasaki disease solely affects young children, primarily male and under the age of five (via the Mayo Clinic). IgA vasculitis is also more common in children and is the most common form of vasculitis seen in children, according to a 2019 paper published in Frontiers in Pediatrics. Buerger's disease tends to affect smokers, but more often in men who are younger than age 45 (per the NHLBI and the Mayo Clinic). Giant cell arteritis (the one that affects the temporal artery) tends to hit older adults per NHLBI.
Cogan's syndrome, the symptoms and classic presentation of which seems to mirror Ashton Kutcher's case, as he has described it (per NPR), tends to strike people between the ages of 2 and 65, per Genetic and Rare Diseases Information Center. But again, Kutcher, now 44, did not share the specifics of his diagnosis, but rather, only that he experienced an autoimmune flare-up of vasculitis that affected his hearing, vision, and equilibrium (via Twitter). Scientists do not know why Cogan's syndrome occurs, but other forms of vasculitis are known to be familial, including Kawasaki disease and granulomatosis with polyangiitis.
The symptoms
Being an inflammatory condition, vasculitis commonly presents with malaise, including fever and fatigue, per Versus Arthritis. Generally speaking, however, the symptoms of any given case of vasculitis will depend upon the specific blood vessels that have become inflamed and the tissues that have been affected. For example, in giant cell arteritis, which affects the temporal artery, headaches, jaw pain, and eye problems may be present. Vasculitis that affects the aortic artery may cause pain in the chest, abdomen, or limbs, as well as weight loss and fever, according to University of Michigan Health. Kawasaki disease may cause swollen lymph nodes, fevers, rashes, red eyes, and cracked lips and tongue. In all cases of vasculitis, disease progression may lead to complications that have their own symptoms, as discussed below.
In describing his experience with vasculitis, Ashton Kutcher reported vision and hearing impairment and equilibrium problems that made walking difficult (via Access Online). Kutcher did not mention what other symptoms that he may have had, or in what order his symptoms presented, so there may be a lot more to what Kutcher went through than what he has stated publicly. For example, if Kutcher's vasculitis was diagnosed as Cogan's syndrome, a form of vasculitis that is known to affect the eyes and the inner ear, then he may have also dealt with headache, joint inflammation, and muscle pain (i.e., myalgia), according to EyeWiki. Cogan syndrome may also involve gastrointestinal symptoms.
Getting diagnosed
As you might surmise at this point, vasculitis can be challenging to recognize and diagnose, especially in its earliest stages, when malaise may be the primary symptom, according to a 2009 paper published in Best Practice & Research Clinical Rheumatology. If you've been feeling unwell, especially if you have recently dealt with an infection, taken a new medication, or have been diagnosed with an autoimmune condition, then it might be useful to discuss your symptoms with your physician.
If your physician has reason to suspect vasculitis, brace yourself for an extensive interview and physical exam that will help to home in on what may be going on, according to National Organization for Rare Disorders. Your physical exam may include blood tests that look for markers of inflammation such as C-reactive protein and antibodies that are associated with vasculitis, like antineutrophil cytoplasmic antibodies and cryoglobulins, according to a 2015 paper published in Frontiers in Immunology. In addition, analysis of blood chemistry may offer clues as to whether an underlying condition that may cause vasculitis is present, including infection and certain blood cancers, per NYU Langone Health.
Imaging tests such as x-ray, CT scan, PET scan, and MRI can pinpoint the specific blood vessels that may be affected, as well as the extent of tissue damage, per the Mayo Clinic. Angiography can also be useful in diagnosing vasculitis, according to NYU Langone. Your doctor may also biopsy affected tissue for signs of damage.
Treatment
Vasculitis is commonly treated with drug therapy, including anti-inflammatory drugs and immuno-suppressing drugs, according to the University of Michigan. Anti-inflammatory drug therapy is the most common "first-line" treatment for vasculitis, especially large vessel vasculitis like Cogan syndrome, and often makes use of a family of steroidal meds known as glucocorticoids. These include cortisone and prednisone (via Healthline). Unfortunately, glucocorticoids are known for causing some unpleasant side effects, including metabolic issues (e.g., increase in blood sugar, calcium malabsorption, and serum cholesterol and triglyceride levels). If used long enough, these drugs may cause symptoms of overexposure to the hormone, cortisol, aka Cushing's Syndrome, according to the American Association of Neurological Surgeons. Cushing's symptoms include irregular menstrual cycles, slow healing, weight gain, and facial edema (i.e., "moon face").
Immuno-suppressors are an alternative that clinicians like to use when adverse effects of anti-inflammatory therapy are an issue, according to Rheumatology. In fact, immuno-suppression drug therapy is sometimes referred to as "steroid sparing." Immuno-suppressing meds include rituximab or cyclophosphamide, the latter of which may be brought in when organ damage is at issue in vasculitis (per Rheumatology).
Per the University of Michigan, initial treatment, aimed at remission (a cessation of active disease) and, if possible, cure, may continue for three to six months. After that, your doctor may switch you to a milder treatment protocol aimed at delaying, preventing, and minimizing the intensity of future flare-ups. Occasionally, surgery is needed to treat damage to blood vessels and tissue.
The prognosis
Some forms of vasculitis are curable, according to NYU Langone Health. Curable cases tend to be limited to idiopathic vasculitis and those caused by an isolated infection or reaction to a medication (via StatPearls). For Buerger's disease, which is associated with cigarette smoking, a cure may be achieved with smoking cessation, according to Johns Hopkins Vasculitis Center. For vasculitis that occurs as an adverse reaction to a medication, ceasing taking the medication may also provide a lifelong cure.
Generally, however, it is difficult for clinicians to predict which cases of vasculitis will cause flare-ups over time. While research continues in this vein, vasculitis is often regarded as a chronic condition, one that the patient and their healthcare team should expect may return one or more times over the course of one's lifetime. Vigilance as to recurring symptoms is recommended, as is regular lab work, which can detect subtle changes in levels of inflammatory markers.
The mortality rate for vasculitis varies based on which vessels and tissues are affected, and to what extent, according to a 2008 paper published in Clinical and Experimental Rheumatology. Kawasaki disease involves a better than 99% likelihood of survival at five years, for example, whereas microscopic polyangiitis involves a survival rate of 45% to 75% at five years. Early deaths from vasculitis are often the result of active disease, causing infection and/or multiple organ failure. Later deaths from vasculitis are sometimes attributable to adverse treatment effects.
Potential complications of vasculitis
The actor and director, Harold Ramis, died in 2014 from complications due to vasculitis. The complications were not specified in any media coverage. However, known complications of vasculitis include damage to organs and bodily systems served by affected blood vessels and infection that arise opportunistically as a result of immuno-suppressing medical therapy, according to the Mayo Clinic. For example, in Cogan Syndrome, permanent hearing loss may result in the absence of effective treatment.
In addition, the effect of vasculitis on the blood vessels is swelling and bulging, which is known as aneurysm, according to Versus Arthritis. One of the risks of aneurysm is rupture, per Mayfield Clinic. When aneurysm ruptures, the leakage of blood may cause damage to adjacent tissue. In addition, a rupture may cause acute deprivation of blood to affected tissue. When this happens in large arteries that supply blood to the brain or heart, risk of death increases. Indeed, as a general rule, the larger the affected blood vessels, the more damage there may be, and the more important the affected tissue, the more serious/life-threatening the damage may be.
Also, blood clots may form in affected blood vessels, per National Organization for Rare Disorders. Vasculitis may also cause atherosclerosis or rapid advancement of existing atherosclerosis, according to a 2007 paper published in Arthritis Research & Therapy.
Can it be prevented?
Medical science has not developed a reliable means of preventing vasculitis as of this writing, per Medscape. However, anything that works to reduce inflammation in the body may help to prevent or reduce inflammation of the blood vessels. While noting that inflammation comprises a critical and complicated system of chemical reactions aimed at defending the body against illness and injury, the University of Wisconsin School of Medicine and Public Health offers a handout detailing various steps that may be taken to reduce levels of unnecessary inflammation. These include not smoking (remember, Buerger's disease may resolve through the cessation of smoking, according to Johns Hopkins Vasculitis Center), and getting adequate exercise and good quality sleep, stress management, and weight management.
In addition, limiting alcohol use may help to reduce inflammation. To wit, pancreatitis, which comprises inflammation of the pancreas and which may be associated with excessive alcohol use (via Drinkaware), is a known catalyst for vasculitis, according to a 2016 case study published in World Journal of Gastroenterology. Incidentally, Ashton Kutcher was hospitalized for pancreatitis around 10 years ago, according to his wife, Mila Kunis (via People). However, whether there is a connection between Kutcher's pancreatitis and his vasculitis is not known publicly.
Finally, anti-inflammatory eating is aimed at preventing and reducing inflammation, per University of Wisconsin, which notes that 60% of chronic illness might be prevented with a healthier diet.
Eating to reduce inflammation
You are what you eat, they say, and this is no less true with regard to your circulatory system (per WebMD). Some of the foods that may improve circulation include cayenne, turmeric, and garlic, according to Healthline. Green tea may also improve circulation, per Mind Body Green. Likewise, the foods we choose to eat or not eat can also affect inflammation, per University of Wisconsin School of Medicine and Public Health, which points out that the Mediterranean Diet offers a prime example of anti-inflammatory eating — and here's what happens to your body when you go on the Mediterranean Diet.
Some people who have already been diagnosed with vasculitis may require a special diet that is intended to support the health of organs and bodily systems that are involved, according to Vasculitis UK. And for those in active treatment for vasculitis, calcium-rich foods may help stave off osteoporosis, which is a risk with steroidal therapy. In the absence of a special diet, Vasculitis UK recommends that preventing vasculitis flare-ups may involve cutting down on starches, processed foods, and grain-fed meat. Conversely, foods rich in omega-3 fats, including certain fatty fishes as well as green leafy vegetables, flaxseeds, and walnuts are known to be beneficial in preventing/curbing autoimmune disease (but be careful about supplements because some fish oil supplements may react adversely with some medication).
If vasculitis sounds scary, please try to remember that it is also very rare, via Nursing made Incredibly Easy.